My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.60 n.2 Mar. 2007
Laparoscopic adrenalectomy for adrenal myelolipoma
Adrenalectomía laparoscópica por mielolipoma suprarrenal
Octavio A. Castillo1,2, Gonzalo Vitagliano1, Oscar Cortes1, Rafael Sánchez-Salas1 and Leonardo Arellano3
From the Section of Endourology and Laparoscopic Urology. Department of Urology1. Clínica Santa Maria, Department of Urology. School of Medicine. Universidad de Chile2 and Department of Pathology. School of Medicine. Universidad de Chile3. Santiago de Chile. Chile.
SUMMARY
Objetive: To evaluate the results of laparoscopic adrenalectomy for adrenal myelolipoma in a single center.
Methods: Between November 1999 and February 2006, 226 laparoscopic adrenalectomies were performed at our institution. 19 specimens corresponded with adrenal myelolipomas (8%). Mean patient age was 53.8 years (range 35 to 75) with male-to-female ratio 2:1. Clinical data was prospectively collected. Patient characteristics, lesion size evaluated by CT scan or MRI, surgical technique, operative time, operative blood loss, complications, conversion to open surgery and hospital stay were reviewed.
Results: Nineteen adrenal myelolipomas were laparoscopically treated in eighteen patients. 16 lesions were located on the right adrenal gland (84%). Mean surgical time was 84.7 minutes (range 45 to 150). Average bleeding was 25.8 ml (range 0 to 300). Only one patient required a blood transfusion. There were no intraoperative complications or conversions to open surgery. Average hospital stay was 2.1 days (range 1 to 4); no complications were registered during the immediate postoperative period. Pathology reports confirmed all specimens as myelolipomas. Mean maximum tumor diameter was 8.6 cm (range 4.5 to 14).
Conclusions: Adrenal myelolipoma is an infrequent, benign entity which can occasionally become symptomatic due to spontaneous hemorrhage. Typical radiographic presentation permits conservative management in asymptomatic small masses. In cases where surgical treatment is advocated, laparoscopic surgery is a safe and feasible technique with reasonable operating time as well as limited blood loss, hospital stay and convalescence.
Key words: Laparoscopy. Myelolipoma. Adrenal. Adrenal tumor.
RESUMEN
Evaluar los resultados de la adrenalectomía laparoscópica por mielolipoma suprarrenal en un único centro.
Métodos: Entre noviembre de 1999 y febrero del 2006 se realizaron 226 adrenalectomías laparoscópicas en nuestra institución. Diecinueve casos fueron mielolipomas (8%). La edad media de los pacientes fue de 53,8 años (rango de 35 a 75) con una relación varónes: mujeres de 2:1. Los datos clínicos se recogieron de forma prospectiva. Se revisan las características del paciente, tamaño de la lesión evaluado por TAC o resonancia magnética nuclear, técnica quirúrgica, tiempo operatorio, sangrado estimado, complicaciones, conversión a cirugía abierta y estancias hospitalarias.
Resultados: Diecinueve mielolipomas suprarrenales fueron tratados en 18 pacientes. Dieciocho tumores estaban localizados en la glándula suprarrenal derecha (84%). El tiempo operatorio medio fue de 84,7 minutos (rango de 45 a 150). El sangrado estimado medio fue de 25,8 ml. (0-300). Solamente un paciente necesitó transfusión sanguínea. No hubo complicaciones intraoperatorias o conversiones a cirugía abierta. La estancia hospitalaria media fue de 2,1 días (1-4); no se registraron complicaciones en el postoperatorio inmediato. El estudio anatomopatológico confirmó todos los casos como mielolipomas. El tamaño máximo medio fue de 8,6 cm de diámetro (4,5 - 14).
Conclusiones: El mielolipoma suprarrenal es un tumor benigno, poco frecuente, que puede ocasionalmente hacerse sintomático por hemorragia espontánea. La presentación radiológica típica permite un manejo conservador en tumores pequeños asintomáticos. En los casos en los que se recomienda tratamiento quirúrgico la cirugía laparoscópica es una técnica segura y factible, con un tiempo operatorio razonable, un sangrado limitado y unos tiempos cortos de estancia hospitalaria y de convalecencia.
Palabras clave: Laparoscopia. Mielolipoma. Suprarrenal. Tumor suprarrenal.
Introduction
Myelolipomas are rare, benign tumors that can usually be found in the adrenal gland, although myelolipomatous foci can be present on other suprarenal diseases or in extra-adrenal locations (1). These tumors were initially described by Giercke in 1905, and 24 years later Oberling coined the term myelolipoma (1). Myelolipomas are composed of mature adipocytes and normal hematopoietic tissue, and although they do not represent a hematopoietic source, they contain precursors of white and red blood cells, such as megakaryocytes. The lesion itself is not hormonally active; however, reports do exist on the presence of myelolipomatous tissue in patients with functional adrenal disorders such as Cushings syndrome, congenital adrenal hyperplasia and Conns syndrome (2,3).
The incidence of adrenal myelolipomas is reported as 0.08% to 0.2% at autopsy (4). With the vast use of noninvasive imaging such as ultrasound (US), computerized tomography (CT) and magnetic resonance (MRI), the incidental detection of these lesions has become more common, reaching frequencies up to 7% of adrenal incidental masses (5). No potential malignancy for adrenal myelolipoma has been proved, although great number of incidentally discovered lesions are small and asymptomatic, reports are not infrequent for cases of voluminous symptomatic lesions, or of those that generate complications such as spontaneous retroperitoneal hemorrhage (6-9). Symptomatic lesions should be treated and the classic approach has been open surgery (1,7-10). With the advent of minimally invasive surgery, laparoscopic adrenalectomy has shown a considerable decrease in surgically derived morbidity, as well as in hospital stay and convalescence. Although many large laparoscopic adrenalectomy series include cases of myelolipomas we believe this is the first report on the outcomes of laparoscopic adrenalectomy exclusively for myelolipoma (11-14,17).
Materials and methods
Between November 1999 and February 2006, 226 laparoscopic adrenalectomies were performed by the same surgeon (O.A.C) at our institution. Out of the 226 adrenalectomies, 19 were myelolipomas (8%). One patient underwent bilateral laparoscopic adrenalectomy. Mean patient age was 53.8 years (range 35 to 75) with male-to-female ratio 2:1. Data was prospectively collected. Patient characteristics, lesion size evaluated by CT scan or MRI, surgical technique, operative time, intraoperative bleeding, complications, conversion to open surgery and hospital stay were reviewed.
Surgical technique: All procedures were carried out transperitoneally. When left side adrenalectomy is performed, three trocars are placed 3 cm below the costal rim: a 10 mm trocar on the medial axillary line for the camera, a second 10 mm trocar on the posterior axillary line and a third 5 mm trocar on the median clavicular line as working ports. In these cases is necessary to incise the splenocolic ligament to mobilize the splenic angle of the colon. The spleen and the tail of the pancreas are mobilized medially for adrenal gland visualization. Due to the transperitoneal approach, adequate exposition of adrenal tumor implies complete mobilization of the spleen. For right side procedures a fourth 5 mm trocar is added in the epigastrium for liver retraction. Also, in these cases, the triangular hepatic ligament is sectioned to mobilize the liver. Peritoneum is incised transversally along the liver border and dissection is carried out laterally along Toldts line and medially over the inferior vena cava. In both, the right and left sides, the adrenal vein is dissected, clipped and divided as the first step of the operation.
Results
A total of 18 patients (12 male and 6 female) underwent 19 laparoscopic adrenalectomies for myelolipoma. Complete endocrine evaluation was performed in all patients to rule out a functional adrenal tumor. All tumors were incidentally diagnosed by abdominal imaging and surgery was indicated. No fine needle biopsy was performed in any case. Mean tumor size was 8.6 cm (range 4.5 – 14). Medical conditions associated in this series were diabetes (3 patients), HTA (3 patients) and morbid obesity (3 patients). 16 lesion were located on the right adrenal gland (84%) and 3 lesion on the left gland. Mean surgical time was 84.7 minutes (range 45 to 150). Mean blood loss was 25.8 ml (range 0 to 300); blood loss was estimated by the anesthesiologist and considered 0 cc when there was no measurable blood loss in the suction / irrigation device. Only one patient required a blood transfusion due to a low preoperative blood count. There were no intraoperative complications or conversions to open surgery. Mean hospital stay was 2.1 days (range 1 to 4); and there were no postoperative complications. Final pathology confirmed all specimens as myelolipomas. Table I summarizes patient characteristics and operative results.
Discussion
Myelolipomas are small, asymptomatic hormonally inactive tumors. They typically, do not reach over 5 cm in their maximum diameter. The benign nature of these lesions has been established. Nevertheless remains unclear how this tumor actually develops. The most widely accepted theory is adrenocortical cell metaplasia of the reticuloendothelial cells of blood capillaries in response to stimuli, such as necrosis, infection or stress.18 In our series many of the myelolipomas were found in patients with other medical conditions such as hypertension, diabetes mellitus and obesity. There is no proved link between these conditions and myelolipomas, yet elderly patients undergo imaging studies for other reasons, facilitating incidental diagnosis. Occasionally, there are clinical symptoms, such as abdominal or flank pain. Spontaneous retroperitoneal hemorrhage in association with myelolipoma has been described (7,10). In our series no patient was diagnosed with this presentation.
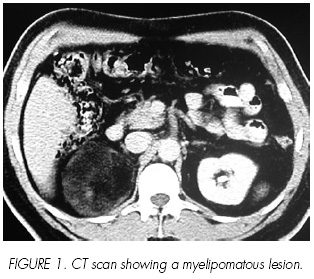
A large series of myelolipomas reported by Kenney et al.1 provides an extensive description of the tomographic characteristics of these lesions. They found that in the total number of patients studied (n=74) an area of fat attenuation appeared in the CT. The measuring in areas that visually looked like fat fluctuated from –130 to –23 HU (average of –74 HU). After administering contrast, there was an average increase of 26 HU. In their series, the majority of the lesions were represented by fat in at least 50% of their extension, in one third of the cases this percentage exceeded 90%, and in only 5 cases it was below 10%. Also, in the CT images some degree of calcification was found in 24% of the lesions, and a complete or partial pseudocapsule between the mass itself and the surrounding retroperitoneal fat in 75% of the cases. The series reported by El-Mekresh et al.10, showed that CT features a homogeneous and well outlined fatty mass in 8 myelolipoma patients, with an average attenuation of –70 HU. In the majority of cases, the tomographic characteristics of the lesions allow for a diagnosis, even in the presence of hemorrhage and/or calcification. When CT images are equivocal MRI imaging will not offer any advantage, in these cases some authors suggest performing fine needle aspiration biopsy (15,16) (Figure 1).
Differential diagnosis of myelolipoma includes: retroperitoneal lipoma, liposarcoma, exophytic renal angiomyolipoma, adrenal adenoma, adrenal metastais and primary adrenal malignancy. With multiflat images it is usually possible to exclude a renal angiomyolipoma. Retroperitoneal liposarcomas usually can be excluded since they are nonhomogeneous and infiltrative (8). In our series MRI or fine needle aspiration biopsy was not performed due to the fact that all masses were over 4.5 cm and malignancy could not be discarded.
Histological examination of myelolipoma show mature fatty tissue with interspersed hematopoietic elements consisting of myeloid and erythoid precursors as well as megakaryocytes (1,7,8). The apparent pseudo-capsule of these tumors seen through CT corresponds to the thin ring of residual cortex adjacent to the suprarenal capsule and not to a genuine capsule of the myelolipoma itself (1). When a suspicious mass is symptomatic or when diagnosis is not clear, surgical exploration becomes necessary. Traditionally the classic approach to this pathology has been open surgery (7-10) (Figure 2). Ever since its introduction by Gagner in 1992, laparoscopic adrenalectomy has become the standard of care for the treatment of functioning and nonfunctioning adrenal tumors (19). Many authors have verified a decrease in perioperative morbidity and convalescence when compared to open surgery (11-14,16,17). Many series of laparoscopic adrenalectomies indicated for multiple adrenal pathologies include cases of adrenal myelolipoma. Novitzky et al. (12) reported two cases of laparoscopic adrenalectomy for myelolipoma in a series of 24 patients with masses of over 5 cm in diameter. Gagner et al. (13) also included 2 patients with adrenal myelolipoma in their series of 100 consecutive laparoscopic adrenalectomies and Gill et al. (11) in a series of 9 patients selected for a protocol on ambulatory laparoscopic adrenalectomy, report a 4.1 cm myelolipoma. However there are no specific reports showing the results of laparoscopic adrenalectomy for suprarenal myelolipoma.
Herein, we present our series of laparoscopic adrenalectomies for adrenal myelolipoma. All tumors were 4.5 cm or bigger in diameter; tumor size did not preclude the indication for laparoscopic approach. We believe that the presence of the pseudocapsule in adrenal myelolipomas facilitates mass dissection as well as vascular control, making laparoscopic surgery for these tumors technically less complex and permitting the management of masses over 5 cm.
Current imaging technology allows for the detection of myelolipoma with a very low index of false negative results and it has been well established that asymptomatic myelolipomas should be observed. Our series reflect the experience accumulated in 7 years. During this time, significant technological advances were made in the field of imaging. This evolution has provided more reliable radiological diagnosis allowing safe observation of this benign pathology. However, the majority of these advances were not available when most of the cases were diagnosed. Also, myelolipomas in our series were usually larger than 6 cm and adrenal carcinoma could not be discarded.
Conclusions
Adrenal myelolipoma is an infrequent, benign entity which can occasionally become symptomatic due to tumor size or spontaneous hemorrhage. Typical radiographic presentation permits conservative management in asymptomatic small masses. Controversy remains on surgical indication. When surgery is indicated, laparoscopy should be considered the standard of care.
Bibliografía y lecturas recomendadas (*lectura de interés y ** lectura fundamental)
*1. KENNEY, P.J.; WAGNER, B.J.; RAO, P. et al: Myelolipoma: CT and Pathologic Features. Radiology, 208: 87, 1998. [ Links ]
2. DIECKMANN, K.P.; HAMM, B.; PICKARTZ, H. et al: Adrenal myelolipoma: clinical, radiologic, and histologic features. Urology, 29: 1, 1987. [ Links ]
3. OLIVA, A.; DUARTE, B.; HAMMADEH, R. et al: Myelolipoma and endocrine dysfunction. Surgery, 103: 711, 1988. [ Links ]
4. OLSSON, C.A.; KRANE, R.J.; KLUGO, R.C. et al: Adrenal myelolipoma. Surgery, 73: 665, 1973. [ Links ]
5. ASO, Y.; HOMMA, Y.: A survey on incidental adrenal tumors in Japan. J. Urol., 147:1478, 1992. [ Links ]
*6. MEAGLIA, J.P.; SCHMIDT, J.D.: Natural history of an adrenal myelolipoma. J. Urol., 147:1089, 1992. [ Links ]
*7. LAMONT, J.P.; LIEBERMAN, Z.H.; STEPHENS, J.S.: Giant Adrenal Myelolipoma. Am. Surg., 68: 392, 2002. [ Links ]
8. LAWLER, L.P.; PICKHARDT, P.J.: Giant Adrenal Myelolipoma presenting with Spontaneus Hemorrhage. CT, MR and Pathology Correlation. Ir. Med. J., 94: 231, 2001. [ Links ]
9. BISHOFF, J.T.; WAGUESPACK, R.L.; LYNCH, S.C.; et al: Bilateral Symptomatic Adrenal Myelolipoma. J. Urol., 158: 1517, 1997. [ Links ]
10. EL-MEKRESH, M.M.; ABDEL-GAWAD, M.; EL-DIASTY, T. et al: Clinical, radiological and histological features of adrenal myelolipoma: review and experience with a further eight cases. Br. J. Urol., 78: 345, 1996. [ Links ]
11. GILL, I.S.; HOBART, M.G.; SCHWEIZER, D. et al: Outpatient Adrenalectomy. J. Urol., 163: 717, 2000. [ Links ]
**12. NOVITSKY, Y.W.; CZERNIACH, D.R.; KERCHER, K.W. et al: Feasibility of laparoscopic adrenalectomy for large adrenal masses. Surg. Laparosc. Endosc. Percutan Tech, 13: 106, 2003. [ Links ]
13. GAGNER, M.; POMP, A.; HENIFORD, B. et al: Laparoscopic Adrenalectomy: Lessons Learned From 100 Consecutive Procedures. Ann. Surg., 226: 238, 1997. [ Links ]
**14. HOBART, M.G.; GILL, I.S.; SCHWEIZER, D. et al: Laparoscopic Adrenalectomy for Large-Volume (> or = 5 cm) Adrenal Masses. J. Endourol., 14: 149, 2000. [ Links ]
15. MUSANTE, F.; DERCHI, L.E.; BAZZOCCHI, M. et al: MR Imaging of Adrenal Myelolipomas. J. Compt. Assist. Tomogr., 15: 111, 1991. [ Links ]
16. WINFIELD, H.N.; HAMILTON, B.D.; BRAVO, E.L. et al: Laparoscopic Adrenalectomy: The Preferred Choice? A Comparison to Open Adrenalectomy. J. Urol., 160: 325, 1998. [ Links ]
**17. GILL, I.S.: The Case for Laparoscopic Adrenalectomy. J. Urol., 166: 429, 2001. [ Links ]
**18. HAN, M.; BURNETT, A.; FISHMAN, E.K. et al: The natural history and treatment of adrenal myelolipoma. J. Urol, 157: 1213, 1997. [ Links ]
**19. GAGNER, M.; LACROIX, A.; PRINZ, R.A. et al: Early experience with laparoscopic approach for adrenalectomy. Surgery. Dec;114:1120; discussion 1124-5. 1993. [ Links ]
![]() Correspondence:
Correspondence:
Octavio Castillo
Section of Endourology and Laparoscopic Urology
Department of Urology
Clínica Santa María
Avenida Santa María 0500
7530234 Providencia,
Santiago de Chile. (Chile).
octaviocastillo@vtr.net
Trabajo recibido: 28 de agosto 2006