My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.60 n.4 May. 2007
Athermal robotic technique of radical prostatectomy: an assistants perspective.
Anil Mandhani, Roy Berryhill Jr. and Ash K. Tewari.
Robotic Prostatectomy Program & Urology Oncology Outcomes. Weill Medical College at Cornell University New York Presbyterian Hospital. Brady Urological Institute. New York, USA
SUMMARY
Robotic radical prostatectomy is fast getting popular as an alternative to the open and laparoscopic radical prostatectomy. Planning for port placement and the assistants role are the two crucial yardsticks for the success of this procedure. Ideal port placement for radical robotic prostatectomy is not only crucial for the surgeon at the console but also for the patient side assistant. A better assistance could enhance the functional outcome of the procedure and at the same time could increase the comfort level of the surgeon at the console. This article describes the role of an assistant in robotic radical prostatectomy.
Key words: Robotic radical prostatectomy. Port placement. Assistant. Fourth arm.
Introducción
Real-time, 3-dimensional vision, motion scaling for tremor filtration and wristed instruments with 7 degrees of freedom for movement give the robotic-assisted radical prostatectomy (RRP) an edge over the laparoscopic approach. These advantages result in better precision and accuracy of the dissection and reconstruction of this deep seated organ in the pelvis, the prostate.
As robotic surgery simulates open surgery yet upholds the advantages of minimally invasive surgery, the learning curve for a skilled open but laparoscopically inexperienced surgeon is much shorter than conventional laparoscopy. In one study the learning curve was estimated to be 8-12 cases for RRP versus 80-100 cases for laparoscopic radical prostatectomy (LRP) (1). This short learning curve could not be achieved without a laparoscopically skilled patient-side assistant.
The console and robotic arms in a robotic system are often described with the master and slave analogy. This is not entirely accurate as the master and console are not entirely dependent on the robotic arms but rather the additional skills of a laparoscopically trained patient-side assistant. Therefore the role of assistant is not only to strengthen the performance of the surgeon at the console but also to ensure safety, ease and speed of surgery. Assistant tasks include the preoperative workup, patient positioning and port placement planning, all needed for the most proficient and productive assistance. Herein we describe the role of the patient-side assistant in setting up the operating room and readying the patient for RRP.
Is the left-side assistant redundant with a 4-arm robot?
Many academic centers utilize two assistants for the RRP, selected from residents or fellows. The necessity of the 1st assistant is not disputed for the complex procedure. But with the recent addition of 4-arm robotic systems the role of 2nd assistant is being debated.
The 4-arm da Vinci robot (Intuitive Surgical, Sunnyvale, California) has been introduced and is gaining popularity. The 4th arm can be placed on either side of the patient supplanting the use of one patient-side assistant. In fact, Sundaram et al have shown that the 4th arm can effectively be used in lieu of a left-side assistant (2). Similarly, use of the 4th arm has been described in retroperitoneal RRP, using it as a right-side assistant (3). The operating surgeon switches between the right working arm and the fourth arm by stepping on the console clutch pedal. This 4th arm uses a grasping forceps to hold the tissue and then the arm is locked in position to retract and rotate the prostate (3).
One argument for the 4th arm is the lack of close patient-side assistant communication and supervision from the console (2). But this line of reasoning is essentially moot for the RRP since the prostate cannot be removed without patient-side assistance.
We feel that having a human assistant provides invaluable help in terms of giving interactive retraction instead of the fixed retraction provided by the 4th robotic arm. Having a 4th robotic arm can also disrupt the traditional learning curve, the surgeon often progressing in gradual transition from left side to right side and finally to the console. This learning method is especially valuable for new surgeons, providing the optimal feedback for understanding each essential and critical step of the RRP.
Preparing the patient for surgery:
Apart from stopping blood thinners, the most effective preoperative preparation is to encourage patients to reduce weight and adopt an exercise mentality. Prior abdominal scars should be carefully noted as they may alter the site for creating the pneumoperitoneum using either a veress needle or Hassans technique of direct visualization. Careful scar observation may, in fact, help planning for necessary adhesionolysis. As an assistant, one should be aware of common anesthesia precautions such as insertion of a nasogastric tube or propping up the head in Trendelenberg position. Fluid restriction is particularly important during the operation so as to avoid congestion of the face and neck and similarly flooding the operating field with excessive urine output.
The assistant must also look for laxity of the scrotal skin, anticipating pneumoscrotum. (Figure 1) Pneumoscrotum develops in many patients but for some, this is significant, probably depending on a patent processus vaginalis or subclinical hernia. We have observed that in elderly people, where the scrotal skin is lax and a significant pneumoscrotum develops, patients have developed a painful postoperative, non-infective inflammatory scrotal edema. This could be minimized by giving strong scrotal support in the immediate postoperative period.
Positioning of the patient:
Before putting the patient to sleep, the supine patients buttocks are positioned a little beyond the leg break of the table so as to compensate for an expected cephalad slide of patient in extreme Trendelenberg. This avoids repositioning once the patient is anesthetized. The patients legs are also supported in stirrups and kept in lithotomy position. After applying lower extremity sequential compression device cuffs, the arms of the patient are secured to the patients side. Both hands are also protected using egg crate foam resting on the arm sleds. The sleds are positioned to give enough space for the assistants and to avoid inadvertent pressure on the hands by robotic arms (B and D in Figure 2). Similarly foam and adhesive tape is used to support both shoulders in a crisscross manner over the chest, counteracting the gravity effects on the patient in the extreme Trendelenberg position (C in Figure 2). Custom-made foam, or a Shea headrest, is kept over the face to protect the intubation tube and to avoid inadvertent injury to the face (A in Figure 2).
In patients with restricted movement of abduction and flexion at the hip joint, preoperative positioning simulation is advisable. For these special patients, instead of using stirrups in the convention manner, spreader bars or leg support at the table edge should be used, depending upon the height of the patient. (Figure 3)
Port placement:
Port placement is an integral part of the surgery and success of the procedure depends on this intricate task. Every surgeon has a different approach but, as a rule, if one sticks to the scientific basis for endoscopic instrumentation, the surgical procedure invariably succeeds.
Like conventional laparoscopy, the variety of available instruments is limited and reaching every target tissue is challenging. In robotic radical prostatectomy the vesicoourethral anastomosis is typically the farthest limit for the robotic instruments. This length is invariably dependent upon the functional length of each robotic instrument. Once the camera and robotic ports are in place, the port placement decisions are final and later change is not feasible or, at the least, potentially harmful. A lack of strategy or any unplanned port placement would divert the attention of the surgeon from the nuances of technique and instead keep the surgeon struggling to reach surgical targets and jeopardize the surgical goals.
The camera port position has been carefully described by Hemal et al to be at 2.5 cm below the level of the umbilicus (4). However, this cannot be applied as a universal rule. The umbilical position varies depending on the height and weight of the patient and the port position must be appropriately adapted to each body type.
In one study of anatomical geometric analysis, the pubic symphysis was reported to be the optimal landmark for calculating the placement of robotic ports. The prescribed 18 cm from the pubic symphysis was based on the then available functional length of the robotic arm (5). Similarly, the distance between any two robotic ports in transverse axis was suggested to be 11 - 24 cm, quite a divergent range (5, 6).
In conventional laparoscopy, for the ideal suturing position, Rassweiller et al suggested that the angle between two working arms should be approximately 45º (6). But this 45º angle does not apply to robotic arms since the 7 degrees of movement available at the instrument tip allows the suture needle to move in any direction, obviating the need for an ideal angle. The distance between two working arms is important for avoiding collision and rollover between robotic arms and assistant arms and to gain a maximum range of movement.
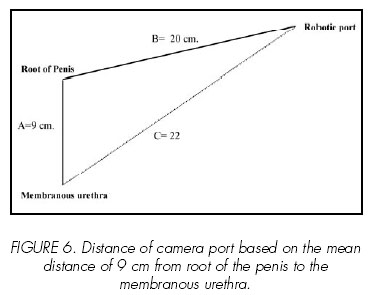
As the pubic symphysis is difficult to feel in obese patients we use the root of the penis as our landmark for calculating the distance for the camera port. We follow the simple rule of 20 strategy irrespective of the patients body size and height. The root of the penis is an easily visualized landmark, corresponds well with the membranous urethra, and its position remains static even after pneumoperitoneum, making it an ideal landmark (Figure 4). With the functional arm length of our current robotic instruments being exactly 30 cm (Figure 5), we calculate a safe distance of 20 cm between the camera port and the root of the penis based on MRI study this distance gave a save trajectory of robotic port well within its functional length (Figure 6). In our last 120 cases we have not encountered any problem with this calculation, irrespective of the height and BMI of the patients.
Once the pneumoperitoneum is established, the robotic arm ports are placed at 20 cm from the root of the penis and 20 cm apart from each other in the transverse axis. Therefore, due to the difficulty in feeling the pubic symphysis of obese patients and the difference in the level of the umbilicus according to patient height and weight, we consider the root of the penis as the ideal landmark (Figure 4).
Camera port and creation of pneumoperitoneum:
Creating a pneumoperitoneum is similar for robotic and non-robotic assisted laparoscopic procedures. We insert a bladed 12 mm trocar (Ethicon, Somerville, New Jersey) with the direction of blade in the midline. This blade orientation is necessary since the fascia is further incised vertically at the end of the case in order to properly retrieve the final specimen. In obese patients, it is always better to use a long port for the camera arm trocar. This will help avoid inadvertent port dislodgment due to the extreme pitch and yaw movements of the camera arm.
Direction of entry for robotic ports:
All trocars should be inserted with its cannula perpendicular to the skin surface. This gives a wide range of motion for the instruments, especially the robotic ports, as the instruments need to be moved from one extreme, such as the right iliac vessels, to the opposite side to reflect the sigmoid colon. (Figure 7). Obliquely placed robotic ports tent the peritoneum and restrict instrument movements, not only complicating the apical dissection but also causing difficulty with the vesicourethral anastomosis, particularly while taking lateral stitches.
Placement of assistant ports:
Assistant ports (12 mm for the right and 5 mm for the left) are usually at or cephalad to the level of the robotic ports and should be 1.5 inches or 2 fingers length proximal to the superior iliac crest. (Figure 8). Ports too close to the iliac crest will allow instrument passage dangerously close to the iliac vessels. These ports should always be placed only after making sure that the reflection of colon is not on a trajectory with the cannula through the peritoneum. This is accomplished by pressing with a finger on the abdomen at the planned trocar site and visualizing the indentation from inside the peritoneal cavity. Our assistant ports are dilating ports which require extra force for their entry into the peritoneal cavity. Therefore, ports should be inserted with caution using one hand to prevent rapid entry and under direct vision.
Suction port:
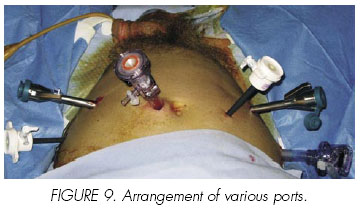
The suction port is a 5 mm port and is inserted at the lateral edge of the rectus abdominis in order to avoid inadvertent injury to the inferior epigastric vessels. This suction port is best at or cephalad to the level of camera port, using a long suction cannula to reach the distant membranous urethra. (Figures 8, 9). By keeping the camera port just left of the umbilicus there remains a sufficient space between the camera port and right robotic port. We use a total of six trocars, with three ports to the right of the camera and only two ports to the left. If the suction port is positioned too low, movements of the left robotic instruments are hamperd, creating discomfort for the right-side assistant. An extreme cephalad port would cause the suction tip to traverse more of the abdomen, increasing the risk of collision with the intestines. This is particularly dangerous for an assistant lacking experience in conventional laparoscopy.
Docking the robot:
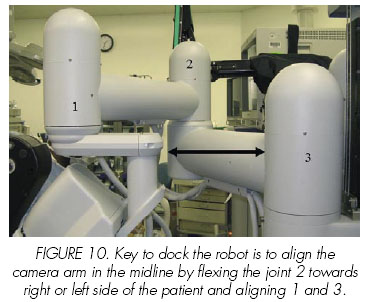
Before docking the robot at the patient, the assistant should make sure that the camera arm is vertically straight and flexed with the 2nd joint towards the left side of the patient (Figure 10). For a right-handed surgeon at the console, the dominant robotic arm (right arm) moves more than the non-dominant arm. The distance between the posts of the 1st and 3rd joint should be equal to about 2 fists. This distance invariably establishes the floor position of the robot tower core. With this ideal arrangement, the distance from of the center column of the robot to the edge of the table is usually from 50 to 60 cm.
This careful tower positioning helps in obtaining an ergonomically similar position of the robotic arms, mimicking that of human arms during open surgery. While docking the robot, the assistant should make sure the any mobile overhead operating room lights are not in the path of the incoming, sterilely-draped robotic arms. The camera arm should be docked first and robotic instruments should be inserted slowly under direct vision with the robotic arm clutched. A natural position is achieved by lateralizing the instrument arms of the robot after the robot is docked to the trocars. To lateralize a robotic arm, the first setup joint is depressed and moved to its most lateral and highest position.
Role of an assistant:
The assistant role is very important in reducing the total time in the operating room. With the above described suggestions, total time from skin incision to start of the console can be minimized to 8 - 12 minutes
Basic principle of instrument exchange by assistant:
According to the principles of conventional laparoscopy, most instrument exchanges are made without actually seeing the entire trajectory. Overshooting of the assistant instruments may injure the opposite iliac vessels and/or colon as its entry is blind. So the assistant must have a specific trajectory in mind while exchanging instruments. This is best achieved by directing the instrument towards penis, generally with an anterior inclination, and in a slow, smooth motion. Careful attention should be made to respect any resistance, however slight, while advancing the instruments.
Right side assistant:
The right-side assistant plays a crucial part in the procedure. The basic knowledge of conventional laparoscopy helps in facilitating the procedural complexity and contributes to patient safety. Mute communication between the surgeon at the console and the right-side assistant speeds up the procedure and surgery becomes a visual treat to watch.
With the athermal technique of RPP, clip application using Hem-o-lock clips (Weck Closure Systems, Research Triangle Park, North Carolina) is a crucial step for the right-side assistant. The amount of tissue the console surgeon attempts to dissect should lead the assistant to choose between 5 mm and 10 mm Hem-o-lock clips. Using the suction port for scissors saves time by eliminating the step of cutting the stitch from the right assistant port and exchanging the shears with the needle driver for needle removal. If the suction port is used for the scissors then the instrument should be advanced close to the anterior abdominal wall and towards penis so as not to injure bowel.
When removing needles one should retract the instrument slowly until the needle has safely entered the cannula and then, with a smooth but swift motion, the needle should be taken out of the port. Any resistant when the needle enters the cannula should cause the assistant to stop and methodically repeat the move. If, despite repeated attempts, resistance is still felt, the console surgeon should help the assistant by directing the camera at the cannula. An experienced console surgeon may even advance the camera lens inside the assistant cannula for accurate retrieval of a misplaced needle inside the port.
Suction and irrigation:
Suction/irrigation is one of the most important and difficult-to-master tasks for the right-side assistant. Suction should be intermittent to prevent loss of pneumoperitoneum. The tip of the suction cannula should be kept close to the operating area so that smoke can be sucked directly without fogging the vision. Similarly, irrigation under pressure helps keep the field clear, especially for venous bleeding.
While irrigating one should direct the force of stream away from the lens or under cover of a tissue layer so as to avoid spraying droplets onto the lens. This suction/irrigation maneuver requires coordination with the movements of the console surgeon. Excessive suction may cause loss of the pneumoperitoneum with the subsequent risk of the robotic ports, since they are fixed to the robotic arms, being dislodged from the abdomen. This unwanted effect could require extra operating time to reestablish the port and risk the inadvertent enlargement of the fascial incision.
Left-side assistant:
One of the crucial roles played by the left side assistant is to supply an appropriate lens (30 degree up, 30 degree down, or 0 degree), on demand, which is clean and warmed close to or exceeding body temperature. The strategy of lens use we follow is using a 30º up lens for initial bladder and prostate mobilization. This is followed by a 0º lens for defattening of the anterior surface of the prostate, exposing the endopelvic fascia, taking the initial dorsal venous complex (DVC) bunching suture, taking the proximal bladder neck suture by bimanual pinch (7), posterior and anterior apical prostate dissection and the vesicourethral anastomosis. A 30º down lens is used for the bladder neck incision, seminal vesical and vasa dissection, control of the prostate pedicles, and neurovascular bundle dissection. On an average there are three to four lens changes in a typical procedure (8).
The left-side assistant also plays an important role in giving traction during the dissection of the posterior bladder neck, the vas deferens and seminal vesicals (A, B, C in Figure 11), contra lateral neurovascular bundle (NVM), Denonvillier fasica, and the posterior aspect of the prostatic apex (D in Figure 11). This traction is very crucial for the athermal technique of RRP as the console surgeon requires the use of both hands to dissect the lateral prostatic pedicles, the tissue around the NVB, and to create space for applying clips for vascular control (B, C in Figure 11).
Another crucial juncture is during the vesicourethral anastomosis. At this point, the left-side assistant moves the Foley catheter tip in and out of the urethral stump while the console surgeon is taking bites from the membranous urethra. The right-side assistant could also accomplish this step but periodic suction/irrigation is invariably needed in addition to retracting/securing the anastomotic suture in between bites.
Specimen retrieval and port closure:
An Endocatch device is deployed from the right-side 12 mm port just after the prostate is isolated. The string attached to the endobag is left hanging outside the right-side assistant port. After the console procedure is complete, the long thread of the endobag is held with endoscopic grasping forceps and fed back through the right-side assistant port, into the camera port under direct vision and the string is taken out of the abdomen through this camera trocar. The paraumbilical camera port incision is then enlarged, depending on the volume of the prostate, and specimen bag is removed. As robotic ports as self-dilating, they are not closed so as the 5 mm ports. Right side 12 mm, we still close it using endoclose device.
![]() Correspondence:
Correspondence:
Anil Mandhani, M.D.
525 East 68th Street
Starr 900
New York, NY 10021
U.S.A.
anilpall@yahoo.com
anm9118@nyp.org
References and recommended readings (*of special interest, **of outstanding interest)
*1. AHLERING, T.E.; SKARECKY, D.; LEE, D. y cols.: Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: initial experience with laparoscopic radical prostatectomy. J. Urol., 170: 1738, 2003. [ Links ]
2. SUNDARAM, C.P.; KOCH, M.O.; GARDNER, T. y cols.: Utility of the fourth arm to facilitate robot assisted laparoscopic radical prostatectomy. BJU, 95: 183, 2005. [ Links ]
3. ESPOSITO, M.P.; ILBEIGI, P.; AHMED, M. y cols.: Use of fourth arm in Da Vinci robot assisted extra peritoneal laparoscopic prostatectomy: novel technique. Urology, 66: 649, 2005. [ Links ]
4. HEMAL, A.; EUN, D.; TEWARI, A. y cols.: Nuances in the optimum placement of ports in pelvic and upper urinary tract surgery using the Da Vinci robot. Urol. Clin. N. Am., 31: 683, 2004. [ Links ]
*5. PICK, D.L.; LEE, D.I.; SKARECKY, D.W. y cols.: Anatomic Guide for Port Placement for Da Vinci Robotic Radical Prostatectomy. J. Endourol., 18: 572, 2004. [ Links ]
6. RASSWEILER, J.; FREDE, T.; GUILLONEAU, B.: Advanced laparoscopy. Eur. Urol., 42: 1, 2002. [ Links ]
7. TEWARI, A.K.; RAO, S.: Anatomical foundations and surgical maneuvers for precise identification of the prostatovesical junction during robotic radial prostatectomy. BJU Int., 98: 833, 2006. [ Links ]
*8. TEWARI, A.; PEABODY, J.; SARLE, R. y cols.: Technique of Da Vinci robot-assisted anatomic radical prostatectomy. Urology, 60: 569, 2002. [ Links ]











 text in
text in