Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Archivos Españoles de Urología (Ed. impresa)
versión impresa ISSN 0004-0614
Arch. Esp. Urol. vol.62 no.2 mar. 2009
Mullerianosis of the urinary bladder: a rare entity
Mullerianosis vesical: una entidad muy infrecuente
Nicolás Alberto Cruz Guerra, María Dolores Gómez Raposo1, María Jesús Baizan Garcia2, Sara Belén Prieto Nogal, Andrés Gago Juan and Máximo Porto Sierra
Urology, Gynecology1, Pathological Anatomy2 Departments. Zamora. Zamora. Spain.
SUMMARY
Objectives: To report a new case of bladder mullerianosis.
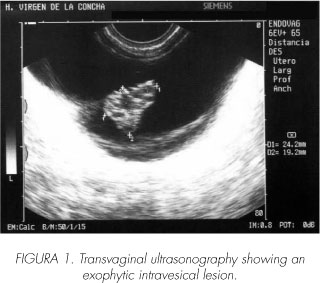
Method: We present the case of a 30 year old female patient with history of miscarriage, who refers voiding disturbances with menstruations. Vaginal ultrasound showed an exophytic bladder lesion, which was confirmed by cistoscopy. Endoscopic resection was indicated.
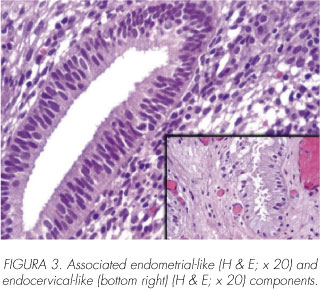
Results: The pathological study of tissues obtained showed mixed glandular structures with predominant tubaric-like type, in association with endometrial- and endocervical-like elements. No evidence of endoscopic relapse after one year of follow-up.
Conclusions: We contribute with a new case of bladder mullerianosis. We emphasize the scarcity of its published reports. We support the option of an endoscopic surgery for these patients.
Key words: Mullerianosis. Bladder. Surgery.
RESUMEN
Objetivo: Descripción de un nuevo caso de mullerianosis vesical.
Método: Presentamos el caso de una paciente mujer de 30 años con antecedentes de aborto, que refiere molestias miccionales coincidiendo con las menstruaciones. Una ecografía vaginal demostró la existencia de lesión exofítica vesical, confirmada posteriormente por cistoscopia. Se indicó resección transuretral.
Resultados: En el estudio histopatológico de los tejidos obtenidos se objetivó un componente glandular mixto de tipo predominantemente tubárico, con elementos endometriales y endocervicales asociados. No evidencia de recidiva endoscópica tras un año de seguimiento.
Conclusiones: Aportamos un nuevo caso de mullerianosis vesical. Destacamos el escaso número de casos publicados. Defendemos la opción quirúrgica endoscópica en estas pacientes.
Palabras clave: Mullerianosis. Vejiga. Cirugía.
Introduction
Bladder endometriosis, as an example of ectopic gynecological tissue, is a well known entity in Urology, despite of a relatively limited amount of reports. What urologists usually have less knowledge about is the possibility - although in unfrequent fashion - of association between endocervical and tubaric epithelium at the same patient, as in the following case.
Case report
We report the case of a 30 years old woman, smoker of six cigarettes per day, with history of miscarriage two and a half years before being studied by the Ginecology department for infertility. In this context, during the performance of a vaginal ecography, an exophytic intravesical lesion was detected, aproximately 24 mm in diameter, and located at right posterolateral wall, with tabications inside (Figure 1).
She was sent to the Urology department, where she referred certain voiding disturbances coinciding with menstruations, without macroscopic haematuria nor other accompanying manifestations. Blood laboratory values were normal, and urine test showed 18 rbc/ mL as single significant outcome. An intravenous pielography was indicated, without abnormal findings; and cistoscopy was performed as well, showing an exophitic lesion, an endoscopic field in size, located at right posterior bladder wall, with pseudocystic surface.
Transurethral resection of that lesion was indicated, achieved in a complete fashion, and with good postoperatory evolution. The pathological study showed a bladder wall coated with focally hyperplastic endothelium, as well as morphologically predominant tubaric-like glandular structures inside the lamina propria and muscular layer, and less frequent endometrial and endo-cervical-like components, what matched with the diagnose of bladder mullerianosis (Figures 2 y 3).
After one year of follow-up, our patient remains symptom-free, and with no evidence of endoscopic relapse at checkups performed afterwards.
Discussion
Mullerian implants at urinary bladder is a fact with significant report availability throughout urological literature. With difference, the most frequent entity comprises presence of endometrial rests - endometriosis -, and its spanish published series has been recently compiled in a throrough fashion (1). however, faced with the description of accompanying endocervical- and/ or endosalpingial-like bladder implants in some patients, the term "mullerianosis" was established by Young y Clement (2), being defined as the combination of at least two of those mentioned tissue types.
The variant comprising simultaneous endometrial, endo-cervical and endosalpingial rests, like in our case report, has scarcely described, usually in form of single case, apart from the mentioned 1996 original publication. The same as an isolated endometrial form, its origin has been subject of several theories, two of which may be emphasized nowadays: firstly, the possibility of an implant from extraurinary origin leaving the corresponding ginecological organs is suggested (3); however, existence of simultaneous mullerian tissue from different anatomical origin, frequently located at hormonosensitive bladder areas such as posterior wall, can support a potential metaplastic tissular mechanism for that entity (4), and a growing amount of authors agree with this last option (5,6).
The most frequent clinical reported manifestations of mullerianosis are irritative voiding symptoms (7) and haematuria (8), affecting female patients througout the third or early fourth decades of life, and usually linked to menstruation cycle. This unspecific sintomatology makes image-based diagnosis - specially ultrasonography - and cistoscopy, necessary to confirm or not the presence of bladder lesion. A pseudocystic endoscopic look raises the differential diagnosis with other entities (8) such as cystic/ glandular cystopathy or isolated endometriosis - especially in this last case because of a chocolate-like liquid content when cutting its surface. Final diagnosis of mullerianosis is based on pathological study of obtained tissues (2), showing - in several proportions according to the different cases - glandular structures coated with a single layer of column-like endometrial-type epithelium, endocervical-type - with cilia and mucinous secretion -, and tubaric-type - with pseudopapilar structures -. Frequent invasion of deeper layers of the bladder wall is a distinguising feature of mullerian implants compared with other benign lesions such as nephrogenic adenoma and the abovementioned cystic/ glandular cystopathy (8).
We support the endoscopical surgical option from a double point of view: diagnostic and therapeutical effectiveness, as reported by other authors (7,8). Adyuvant hormonotherapy was not considered in our case cause o an apparently complete resection of the lesion, the patient's persistent wish of pregnancy in a short-term, as well as pathological predominance of non-endometrial mullerian glands, theoretically less hormonosensitive (9). The relapse of the lesion has not been yet reported, although its follow-up is recommended because of its logical absence of data based on large series, especially if a report showing a case complicated with endometrioid carcinoma (10) is taken into account.
Conclusion
Mullerianosis represents an entity that, in spite of its unfrequency, should be considered among those differential diagnosis for benign bladder lesions. The scarcity of reports makes the future publication of a growing number of cases be necessary for better knowledge of its main features and natural history.
 Correspondence:
Correspondence:
Nicolás Alberto Cruz Guerra
Av. de los Reyes Católicos, 5 bajo izda.
49021 Zamora. (Spain).
ncruz_g@hotmail.com
Accepted for publication: January 7th, 2008.
References and recomended readings (*of special interest, **of outstanding interest)
1. Pastor Navarro H, Donate Moreno MJ, Giménez Bachs J M et al. Endometriosis vesical. Revisión de la literatura, con especial referencia a la española y aportación de dos nuevos casos. Arch Esp Urol 2006; 59: 111-22. [ Links ]
**2. Young RH, Clement PB. Müllerianosis of the urinary bladder. Mod Pathol 1996; 9: 731-737. [ Links ]
3. Javert CT. Pathogenesis of endometriosis based on endometrial homeoplasia, direct extension, exfoliation and implantation, lymphatic and hematogenous metastasis including 5 cases reports of endometrial tissue in pelvic lymph nodes. Cancer 1949; 2: 399410. [ Links ]
4. Krestchmer HI. Endometriosis of the bladder. J Urol 1945, 53: 459-65. [ Links ]
5. Batt RE, Smith RA, Buck Louis GM, et al. Müllerianosis. Histol Histopathol 2007; 22: 1161-1166. [ Links ]
6. Koren J, Mensikova J, Mukensnabl P, et al. Mullerianosis of the urinary bladder: report of a case with suggested metaplastic origin. Virchows Arch 2006; 449: 268-271. [ Links ]
7. Tomada N, Silva J, Vendeira P, et al. [Bladder mullerianosis: a case report]. Acta Urológica 2006; 23: 59-61. [ Links ]
*8. Kim HJ, Lee TJ, Kim MK, et al. Muellerianosis of the urinary bladder, endocervicosis type: a case report. J Korean Med Sci 2001; 16: 123-126. [ Links ]
9. Cao ZY, Eppenberger U, Roos W, et al. Cytosol estrogen and progesterone receptor levels measured in normal and pathological tissue of endometrium, endocervical mucosa and cervical vaginal portion. Arch Gynecol 1983; 233: 109-119. [ Links ]
10. Garavan F, Grainger R, Jeffers M. Endometrioid carcinoma of the urinary bladder complicating vesical Mullerianosis: a case report and review of the literature. Virchows Arch 2004; 444: 587-589. [ Links ]











 texto en
texto en