My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.62 n.4 May. 2009
Laparoscopic radical cystectomy with vaginal specimen extraction. Case report
Cistectomía radical laparoscópica con extracción de pieza por vagina. Caso clínico
Gonzalo Vitagliano, Nicolas Villasante, Juan Paterlini, Carlos Ameri and Osvaldo Mazza.
Oncologic Section. Urology Department. German Hospital. Buenos Aires. Argentina.
SUMMARY
Objective: To report a case of laparoscopic radical cystectomy and pelvic lymphadenectomy with vaginal extraction of the surgical specimen in an elderly patient with muscle invasive bladder tumor.
Method: A 78 year old patient with history of hematuria was diagnosed of muscle invasive bladder cancer. Laparoscopic radical cystectomy and pelvic lymphadenectomy with vaginal extraction of the surgical specimen was performed without incident.
Results: Operative time was 240 minutes, surgical bleeding was 200 ml and hospital stay 8 days. The patient evolved uneventfully and remains disease free after 9 months of follow-up.
Conclusion: Laparoscopic radical cystectomy provides adequate oncologic results with decreased morbidity, making this surgery an attractive alternative for the management of patients in a delicate condition.
Key words: Laparoscopy. Cystectomy. Bladder cancer.
RESUMEN
Objetivo: Presentar la utilidad de una técnica minimamente invasiva como herramienta terapéutica en el tratamiento de un paciente de edad avanzada portador de cáncer de vejiga musculoinvasor.
Método: Paciente femenina de 78 años con cáncer de vejiga avanzado que debuta con hematuria. Se realiza cistectomía radical con linfadenectomía pelviana por vía laparoscópica con extracción de pieza quirúrgica por vía vaginal.
Resultados: El tiempo operatorio fue de 240 minutos con un sangrado de 200 ml y una estadía hospitalaria de 8 días. La paciente evolucionó favorablemente y tras un seguimiento de 6 meses se encuentra sin evidencia de recidiva tumoral.
Conclusión: El bajo impacto quirúrgico permite que este abordaje pueda ser utilizado en casos seleccionados para evitar la severa morbilidad indefectiblemente asociada a la progresión local del cáncer de vejiga avanzado.
Palabras clave: Laparoscopia. Cistectomía. Cáncer de vejiga.
Introduction
Annually more than 54.000 new cases of bladder cancer are diagnosed and more than 5.000 cases of specific cancer related deaths are reported in the United States of America. Estimates suggest that in 2020 more than 20% of the population will be more than 65 years old. This increase in population longevity is associated to an important raise in the incidence of bladder cancer. Besides the high mortality rate of this disease, bladder cancer is associated with a significant morbidity due to severe irritative symptoms, urinary tract obstruction and haematuria (1).
The management of this disease in the elderly represents for the urologist a real dilemma. Not only chronological age should be taken into consideration when evaluating these patients. Biological age and associated co morbidities are very important elements to be considered.
Radical cystectomy continues to be the gold standard treatment for muscle invasive bladder cancer, although it is a high-risk operation due to its perioperative complications (2). Other treatments considering bladder preservation have been proposed for patients with high-risk co morbidities. These alternative treatments lack the oncological results offered by the radical surgery and also have important morbidity (1, 3).
In our institution radical cystectomy continues being the principal indication in the presence of muscle invasive bladder cancer regardless patient's age. We present a case of laparoscopic radical cystectomy and pelvic lymphadenectomy in a 78-year-old female with muscle invasive bladder cancer, in which the specimen was removed through the vaginal fundus.
Case report
A 78 years old female patient, with history of hysterectomy due to uterine miomatosis, arterial hypertension, chronic gastritis and severe smoking during 40 years, presented an episode of macroscopic hematuria 10 years ago, followed by the diagnosis of an exofitic bladder lesion. In that occasion transurethral resection (TUR) was performed. The patient presented short-term recurrence that required multiple TURs. The last biopsy informed anaplasic trabecular carcinoma.
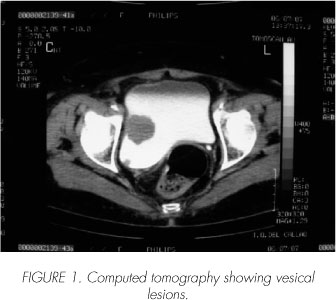
The patient makes a second opinion appointment in the urology unit of this institution. New control tests are required. Ultrasound showed a 35 x 28 x 33 mm right lateral wall solid nodular image and another 10 x 9 x 9 mm right posterior lateral polipoid image. CT scan showed severe right renal atrophy. No lymphatic invasion was found. Bladder lesions were as seen in sonography (Figure 1). Bone scan was normal. Laparoscopic radical cystectomy and pelvic bilateral lymphadenectomy with left cutaneous ureterostomy was indicated. Castillo et al technique was used (4).
Surgical Technique:
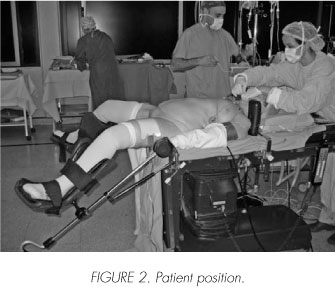
A third generation cephalosporin was administrated during anesthetic induction. We use a modified lithotomic position allowing for maximum Trendelemburg (Figure 2). We puncture with a Veress needle through a supraumbilical incision to generate a 15-mmHg pneumoperitoneum. Ports are placed in forming a "W" as described in the corresponding technique (Figure 3). The rectovesical pouch peritoneum is horizontally sectioned. This section continues bilaterally between the spermatic vessels and the umbilical ligament forming an imaginary "H". Both ureters are sectioned, paying special attention to the blood supply of the left ureter.
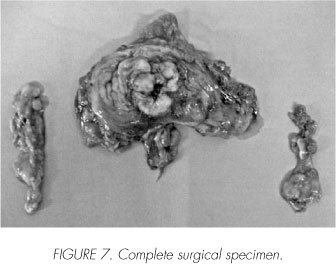
Frozen section segments of these are sent to pathology with negative result for malignancy. Lymphadenectomy is begun at the common iliac artery, reaching distal to the external iliac vessels, including the obturator bundle and laterally reaching the genitofemoral nerves. After dissecting and exposing the posterior vaginal pouch the vesical pedicle is identified, ligated and sectioned. Once the Retzius space is entered, the lateral and anterior margins of the bladder are freed and the urethral approach can begin. We use an inverted "U" incision above the urethra on the anterior vaginal wall (Figure 4). Through this incision we finish liberating completely our specimen and proceed to extract it along with both lymphadenectomies (Figures 5, 6 and 7). The anterior vaginal wall is closed intracorporeally and externally. After the drain tube is put in place, the left ureter is exteriorized through the ipsilateral pararectal port incision.



Operating time was 240 minutes and surgical bleeding was 200 ml. The patient evolved uneventfully and was discharged home on postoperative day 8. A 9-month follow-up has been without evidence of tumour recurrence.
Discusión
Recent studies show acceptable morbidity in elderly patients undergoing radical open cystectomy. Current reports show that no significant differences exist in minor and mayor complications between high risk advanced age patients (29% and 5% respectively) and the general population (35,9% and 4,9% respectively). In elderly patients with or without significant co morbidities, radical cystectomy proved to provide local disease control and extended life expectancy.
Since the first report from Parra et al in 1992, laparoscopic radical cystectomy has evolved to a secure, standardized and reproducible technique. Decreased time to first oral intake, decreased analgesic requirements and shorter hospital stay along with superior cosmetics favour laparoscopic versus open radical cystectomy. However, oncological equivalency has only been proved recently (3,4).
Classic laparoscopic radical cystectomy is associated with a 6 cm minilaparotomy incision. This incision is used for surgical specimen extraction and urinary reservoir creation. In the case reported, the decreased morbidity of laparoscopic radical cystectomy allowed for its employment in an elderly patient. A urinary reservoir was thought to add unnecessary morbidity, and ureteral exteriorization of the only working renal unit was done through an ipsilateral port incision. After the urethra had been freed, the vagina was used to extract the surgical specimen therefore avoiding any abdominal incision.
We believe this mini-invasive approach can be used in elderly patients and in selected cases making it possible to avoid unnecessary morbidity associated to classic open radical cystecotmy.
 Correspondence:
Correspondence:
Gonzalo Vitagliano
Zabala, 2664 3o B
Código postal 1426
Capital Federal. Buenos Aires. (Argentina)
gonzalovitagliano@hotmail.com
Accepted for publication: April 6th, 2008.
References and recommended readings (*of special interest, **of outstanding interest)
**1.Farnham SB, Cookson MS, Alberts G, Smith JA Jr, Chang SS. Benefit of radical cystectomy in the elderly patient with significant co-morbilities. Urol Oncol. 2004; 22(3): 178-81. [ Links ]
2. Ghoneim MA, el-Mekresh MM, el-Baz MA, et al. Radical cystectomy for carcinoma of the bladder: critical evaluation of the results in 1,026 cases. J Urol 1997; 158: 393-399. [ Links ]
*3. Zebic N, Weinknecht S, Kroepfl D. Radical cystectomy in the patients aged > or = to 75 years: an updated review of patients treated with curative and palliative intent. BJU Int. 2005; 95(9): 1211-4. [ Links ]
**4. Castillo O, Cabello Benavento R, Briones Mardones G, Hernández Fernández C. Radical laparoscopic cystectomy. Actas Urol Esp. 2006; 30(5):531-40. [ Links ]
**5. Haber GP and Gill IS. Laparoscopic radical cystectomy for cancer: oncological outcomes at up to 5 years. BJU Int 2007; 100: 137-142. [ Links ]











 text in
text in 


