Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Medicina Intensiva
versão impressa ISSN 0210-5691
Med. Intensiva vol.35 no.4 Mai. 2011
First influenza season after the 2009 pandemic influenza: report of the first 300 ICU admissions in Spain
Primera epidemia de gripe estacional después de la pandemia por gripe A en 2009: descripción de los primeros 300 ingresos en UCI españolas
A. Rodrígueza, I. Martin-Loechesa, J. Bonastreb, P. Olaecheac, F. Álvarez-Lermad, R. Zaragozae, J. Guerrerof, J. Blancog, F. Gordoh, F. Pozoi, J. Lorentej, J. Carratalák, M. Corderol, J. Rellom, A. Estebani, C. Leónn, SEMICYUC-CIBERES-REIPI working group*
aHospital Joan XXIII, Critical Care Department, IISPV, URV, CIBER Enfermedades Respiratorias, Tarragona, Spain
bHospital La Fe, Critical Care Department, CIBER Enfermedades Respiratorias, Valencia, Spain
cHospital Galdakao-Usansolo, Critical Care Department, CIBER Enfermedades Respiratorias, Vizcaya, Spain
dHospital del Mar, Critical Care Department, CIBER Enfermedades Respiratorias, Barcelona, Spain
eHospital Dr. Peset, Critical Care Department, Valencia, Spain
fHospital Gregorio Marañón, Critical Care Department, CIBER Enfermedades Respiratorias, Madrid, Spain
gHospital Rio Hortega, Critical Care Department, CIBER Enfermedades Respiratorias, Valladolid, Spain
hHospital del Henares, Critical Care Department, Madrid, Spain
iPulmonology Department, Hospital 12 de Octubre, Madrid, Spain
jHospital de Getafe, Critical Care Department, CIBER Enfermedades Respiratorias, Madird, Spain
kHospital de Bellvitge, Infectious Disease Department, REIPI, L'Hospitalet de Llobregat, Barcelona, Spain
lHospital Virgen del Rocío, Infectious Disease Department, REIPI, Sevilla, Spain
mHospital Vall d'Hebron, Critical Care Department, IRVH, CIBER Enfermedades Respiratorias, Barcelona, Spain
nCritical Care Department, Hospital Universitario de Valme, Sevilla, Spain
* Members are listed in the acknowledgements section.
Supported by Instituto de Salud Carlos III (Ministry of Science and Innovation).
ABSTRACT
Introduction: During the 2009 influenza pandemic, several reports were published, nevertheless, data on the clinical profiles of critically ill patients with the new virus infection during this second outbreak are still lacking.
Material methods: Prospective, observational, multi-center study conducted in 148 Spanish intensive care units (ICU) during epidemiological weeks 50-52 of 2010 and weeks 1-4 of 2011.
Results: Three hundred patients admitted to an intensive care unit (ICU) with confirmed An/H1N1 infection were analyzed. The median age was 49 years [IQR=38-58] and 62% were male. The mean APACHE II score was 16.9±7.5 and the mean SOFA score was 6.3±3.5 on admission. Comorbidities were present in 76% (n=228) of cases and 111 (37.4%) patients were reportedly obese and 59 (20%) were COPD. The main presentation was viral pneumonia with severe hypoxemia in 65.7% (n=197) of the patients whereas co-infection was identified in 54 (18%) patients. All patients received antiviral treatment and initiated empirically in 194 patients (65.3%), however only 53 patients (17.6%) received early antiviral treatment. Vaccination was only administered in 22 (7.3%) patients. Sixty-seven of 200 patients with ICU discharge died. Haematological disease, severity of illness, infiltrates in chest X-ray and need for mechanical ventilation were variables independently associated with ICU mortality.
Conclusions: In patients admitted to the ICU in the post-pandemic seasonal influenza outbreak vaccination was poorly implemented and appear to have higher frequency of severe comorbidities, severity of illness, incidence of primary viral pneumonia and increased mortality when compared with those observed in the 2009 pandemic outbreak.
Key words: An/H1N1 influenza, Critically ill patients, Prognostic.
RESUMEN
Introducción: Durante la pandemia de gripe A, se publicaron diferentes comunicaciones. No obstante, el perfil clínico de los pacientes críticos afectados por este virus durante este segundo brote epidémico es poco conocido.
Material y métodos: Estudio prospectivo, observacional y multicéntrico realizado en 148 UCI españolas entre las semanas epidemiológicas 50 de 2010 y 4 de 2011.
Resultados: Se incluyó a los primeros 300 pacientes ingresados en UCI con infección confirmada por An/H1N1. La media de edad fue de 49 [38-58] años y el 62% eran varones. La media de APACHE II fue 16,9±7,5, con una media de SOFA de 6,3±3,5. El 76% (n=228) de los pacientes presentaron alguna comorbilidad, 111 (37,4%) eran obesos y 59 (20%) presentaban EPOC. La presentación clínica más habitual fue la neumonía viral con hipoxemia severa (65,7%; n=197), mientras que se observó coinfección en 54 pacientes (18%). Todos recibieron tratamiento antiviral, de forma empírica en 194 (65,3%). Sólo 53 pacientes (17,6%) recibieron tratamiento antiviral precoz; 22 pacientes (7,3%) estaban vacunados. Cumplieron su evolución en UCI 200 pacientes, y fallecieron 67 de ellos. La enfermedad hematológica, la gravedad general, los infiltrados en la radiografía de tórax y la necesidad de ventilación mecánica fueron las variables asociadas de forma independiente con la mortalidad.
Conclusiones: Los pacientes críticos ingresados en UCI durante el brote estacional de gripe pospandémica evidenciaron escaso nivel de vacunación, mayor frecuencia de comorbilidades, un nivel gravedad más elevado, mayor incidencia de neumonía viral primaria y una mortalidad superior en comparación con lo observado durante la pandemia de 2009.
Palabras clave: Nueva Gripe An/H1N1, Pacientes críticos, Pronóstico.
Introduction
During the 2009 influenza pandemic caused by the A(H1N1) 2009 virus, several reports were published regarding the presentation of this disease with severe acute respiratory symptoms in hospitalized patients1-4. Rapidly progressive viral pneumonia represents the primary cause of intensive care unit (ICU) admission with mortality rates ranging from 17.3% to 46% among different sites1-3,5-9. This disease represented a challenge for critical care physicians worldwide. In the 2010-11 winter a seasonal outbreak of influenza has been detected in Spain with most cases caused by the former A/H1N1 2009 pandemic virus, currently called "new A/H1N1 virus" (An/H1N1). Data on the clinical profiles of critically ill patients with the virus An/H1N1 infection during this outbreak are still lacking. Here, we present our experience in a series of the first 300 critically ill patients admitted to Spanish ICUs.
Material and methods
This prospective, observational cohort study of ICU patients was conducted across 148 ICUs in Spain. Data were obtained from a voluntary registry created by the Spanish Society of Intensive Care Medicine (SEMICYUC), the Spanish Network for Research on Infectious Disease (REIPI) and the Spanish Biomedical Research Center Network on Respiratory Diseases (CIBERES). The study was approved by the Joan XXIII University Hospital Ethics Committee (IRB NEUMAGRIP/11809). Patient identification remained anonymous and the informed consent requirement was waived due to the observational nature of the study.
Data were reported by the attending physician reviewing medical charts and radiological and laboratory records. In this case series, data on all patients within the cohort consecutively diagnosed with An/H1N1 influenza between epidemiological weeks 50-52 of 2010 and weeks 1-4 of 2011 are presented (Figure 1). Children under 15 years old were not enrolled in the registry. The An/H1N1 infection was confirmed by means of realtime reverse-transcription-polymerase chain reaction (RT-PCR) on either nasopharyngeal swab samples or tracheal secretions ordered by the attending physicians at ICU admission. An/H1N1 testing was performed in each institution or centralized in a reference laboratory when local resources were not available. A confirmed case was defined as an acute respiratory illness with laboratory-confirmed An/H1N1. Only confirmed cases were included in the current report.
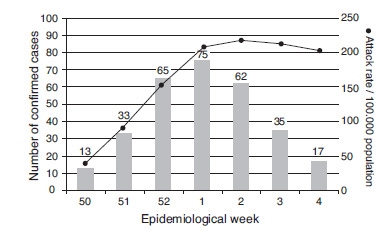
Figure 1. Number of confirmed cases of An/H1N1
virus infection admitted to intensive care unit and
clinical attack rate in Spain (solid line).
The ICU admission criteria and treatment decisions for all patients, including determination of the need for intubation and type of antibiotic or antiviral therapy administered, were not standardized and were made by the attending physician. Systemic corticosteroid use was implemented when patients developed shock (hydrocortisone), or coadjuvant treatment was used for pneumonia (methylprednisolone). Orally administered oseltamivir (150mg/24h or 300mg/24h) or intravenous zanamivir (600mg/12h) was chosen by the attending physician.
Definitions
Primary viral pneumonia was defined in patients presenting illness with acute respiratory distress and unequivocal alveolar opacities involving two or more lobes with negative respiratory and blood bacterial cultures during the acute phase of influenza virus infection5.
Community-Acquired Respiratory Co-infection (CARC) was defined as any infection diagnosed within the first 2 days of hospitalization10. Infections occurring later were considered nosocomial11. Definition of Hospital-Acquired Pneumoniae (HAP) was based on current American Thoracic Society and Infectious Disease Society of America guidelines12. Patients who presented healthcare-associated pneumonia (HCAP) were excluded from the present study12. Obese patients were defined as those with a body mass index (BMI) over 3013.
Patient who had previously received Influenza A (H1N1) 2009 monovalent or seasonal influenza 2010-11 vaccination were considered to be "vaccinated".
Statistical analysis
Discrete variables are expressed as counts (percentage) and continuous variables as means±standard deviation (SD) or medians [25th to 75th interquartile range (IQR)]. For the demographic and clinical characteristics of the patients, differences between groups were assessed using the χ2 test and Fisher's exact test for categorical variables and the Student's t-test or Mann-Whitney U test for continuous variables. Stepwise logistic regression analysis was used to determine the impact of each variable on ICU mortality. The variables included in the multivariate model were those that showed significant differences in the univariate analysis (Table 2), including the variable "vaccination condition" due to its potential clinical interest. Risk is expressed as odds ratio (OR) and its 95% confidence interval (CI).
Data analyses were performed using SPSS 15.0 for windows (SPSS, Chicago, IL, USA). Values of P<.05 were considered to indicate statistical significance.
Results
Data from the first 300 adults admitted to Spanish ICUs during the winter of 2010-11 due to An/H1N1 infection are the focus of the present report. Patients were young (median 49 years) and 62% were male. The mean APACHE II score was 16.9±7.5 and the mean SOFA score was 6.3±3.5 on admission. The baseline characteristics of the population are shown in Table 1. Comorbidities were present in 76% (n=228) of cases. The main comorbid condition reported was obesity in 111 patients (37.4%) followed by chronic obstructive pulmonary disease (COPD) (n=59; 20%), diabetes mellitus (n=45; 15.2%) and haematological disease (n=37, 12.5%) (Figure 2).
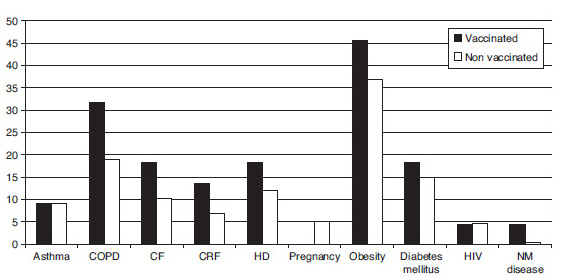
Figure 2. Most common comorbidities reported in confirmed cases of An/H1N1 virus infections,
differentiating vaccinated patients from those who were not. CF: cardiovascular disease;
COPD: chronic obstructive pulmonary disease; CRF: chronic renal failure; HD: hematological disease;
HIV: human immunodeficiency virus infection; NM disease: neuromuscular disease.
The main presentation was viral pneumonia with severe hypoxemia that was present in 65.7% (n=197) of the patients. Forty (13.3%) patients had COPD exacerbation or severe asthma, and CARC was identified in 54 (18%) patients. Streptococcus pneumoniae (n=21), Pseudomonas aeruginosa (n=6), Staphylococcus aureus (n=6) and Streptococcus pyogenes (n=4) were the most frequent microorganisms isolated.
Two-hundred and thirty-seven patients (79%) required mechanical ventilation (MV). Non-invasive ventilation was used in 105 (35%), and failed in 53 patients (50.5%). One-hundred fifty-three patients (51.0%) required vasopressor drugs at ICU admission and 54 (18%) developed acute kidney injury. Forty-one (13.6%) of them received renal replacement techniques.
All patients received antiviral treatment for a median duration of 7 [6-10] days, which was initiated empirically in 194 patients (65.3%). Two-hundred and eighty-five (95%) received oseltamivir, whereas zanamivir was administered in 15 (5%) patients. Finally, eight patients (2.7%) received both antiviral drugs. The median time between the onset of symptoms and the first administered antiviral dose was 5 [3-7] days, with a dose of 75mg/day in 50.3% (n=151) of cases. Only 53 patients (17.6%) received early antiviral treatment (<48 h from symptoms onset).
One-hundred and thirty-one patients (43.6%) received early corticosteroid therapy at ICU admission for a median of duration of 7 [5-10], with 10.6% (n=32) representing coadjuvant therapy for septic shock.
Interestingly, 278 (92.6%) of the patients had not been vaccinated. Vaccinated patients were older (P<.05) and with higher delay between hospital and ICU admission (Table 1). No significant differences in comorbidities were observed between patients with or without vaccination (Figure 2).
As of February 15 2011, 200 patients (66.6%) had been discharged from the ICU and 67 of them (33.5%) had died. The mortality rate was not different between patients who received vaccination (18.2%) compared to those who did not (22.6%; P=.79; OR=1.32; 95%CI, 0.45-3.84). The 4 vaccinated patients who died had significant comorbidities (severe immunosuppression due to lung -n=1- bone marrow transplantation -n=1- and acute leukaemia -n=2-). Among patients who underwent invasive mechanical ventilation (n=117), the mortality was very high (n=62; 53%).
The characteristics of patients at ICU admission according to survival or death (n=200) are shown in Table 2. Patients who died presented higher APACHE II and SOFA scores at ICU admission. No differences in comorbidities were observed except for haematological disease (OR=1.9; 95%CI, 1.5-3.3) and human immunodeficiency virus infection (OR=6.9; 95%CI, 1.1-44.7) which were more frequent in non-survivors. Obesity was associated with a better prognosis (OR=0.8; 95%CI, 0.6-0.9). Development of shock (OR=2; 95%CI, 1.6-2.6); acute kidney injury (AKI) (OR=1.9; 95%CI, 1.4-2.8), need for invasive MV (OR=1.9; 95%CI, 1.6-2.4), number of quadrant infiltrates in chest X-ray (2.6 vs. 1.9; P<.05), steroid therapy (OR=1.3; 95%CI, 1.1-1.7) and CARC (OR=1.6; 95%CI, 1.1-2.4) were most frequent in non-survivors. APACHE II score, SOFA score, infiltrates in chest X-ray, invasive MV, shock at ICU admission, AKI, CARC, hematological disease, HIV infection and vaccination were variables included in the multivariate analysis to determine their association with the mortality. Stepwise logistic regression analysis showed that APACHE II score by point of increase (OR=1.07; 95%CI, 1.01-1.14; P=.02), infiltrates in chest X-ray by quadrant (OR=1.6; 95%CI, 1.08-2.4; P=.01), haematological disease (OR=4.5; 95%CI, 1.2-17.5; P=.02) and invasive MV (OR=9.4; 95%CI, 2.9-30.8; P<.001) were variables independently associated with mortality. The multivariate models had a Hosmer-Lemeshow goodness-of-fit test score of 13.04 (P=.11).
Discussion
To the best of our knowledge, this is the first study that presents a relatively large number of patients admitted to the ICU for severe infection due to the An/ H1N1 virus in the 2010-11 seasonal influenza outbreak, this being in the post-pandemic period.
In our series, the presenting features of An/H1N1 influenza during the winter of 2010-11 were quite similar to those described in the past 2009 A/H1N1 virus infection pandemic. Nevertheless some aspects need to be pointed out.
In this report, the severity of disease in patients (APACHE II score 16.9) was greater than that observed during the 2009 pandemic (APACHE II 13.8; P<.001)5. The frequency of comorbidities in the current series (76% of patients) was also higher than that observed in the 2009 pandemic (69.6%; P=.01)5-7. While obesity remained the most frequent comorbidity, there was an increase in the number of patients with haematological disease during the 2010-11 seasonal influenza outbreak compared to the pandemic period. This was the fourth most frequent comorbidity and it was the only one independently associated with mortality in the multivariate analysis.
Primary viral pneumonia was significantly more frequent (63.2%) during the 2010-11 seasonal influenza outbreak compared with recently published data for the previous (2009 pandemic) outbreak (54.8%; P<.01)10. The rapid progression of pulmonary viral infection from respiratory failure to Acute Respiratory Distress Syndrome (ARDS) may be related to a significant increase in the need for MV in the current seasonal outbreak (79%) compared to the 2009 pandemic outbreak (61.5%; P<.01)14. The mortality rate of ventilated patients was very high (53%) in the present study and invasive MV was independently associated with mortality in the multivariate analysis.
The implementation of early (<2 days) antiviral therapy was associated with a lower mortality rate in ventilated patients with 2009 H1N114. While all patients received antiviral treatment, the present study showed a one-day delay (5 days instead of 4 days) in the administration of antiviral agents compared to previous studies14.
All these variables must be considered in order to explain the higher mortality observed in the current seasonal outbreak (33%) compared to that reported during the 2009 pandemic (21%; P<.01)14. Although in the present study only haematological disease, the need for MV, APACHE II score and number of quadrants infiltrates in chest X-ray were factors associated with mortality, other variables cannot be excluded given that the study may be underpowered to identify other factors also associated with mortality.
The use of corticosteroids in the present report was very high (43% of cases). WHO guidelines for the management of human infection with pandemic (H1N1) Influenza A infection recommend that corticosteroid therapy should not be used routinely. Recently, Martin-Loeches et al15 showed that the early use did not result in better outcomes and may be associated with an increased risk of super-imposed infections.
Many studies have demonstrated temporal relationships between influenza activity and CARC. During past pandemics, the bacteria most often recovered were common colonizers of the upper respiratory tracts of healthy persons, i.e., Haemoohilus influenzae, S. pneumoniae, S. pyogenes or Staphylococcus aureus16-18. Moreover, substantial laboratory evidence for synergism between influenza A and bacterial microorganisms has been suggested19. During the 2010-11 seasonal influenza outbreak, CARC was present in 18% of cases, this prevalence being similar to that reported in the 2009 outbreak (17.5%)10.
Finally, in the present report, 92.6% of the patients admitted to the ICU were not vaccinated. The presentation of ARDS with severe refractory hypoxemia is particularly common in patients with this disease process and might be linked to an abnormal immune response20. Vaccination induces broad and improved cross protection against severe illness of multiple subtypes of influenza A virus. While vaccination has been a matter of debate, there has nevertheless been no evidence of harm or serious side effects in the vaccine trials that were conducted. In our study, the 4 vaccinated patients who died had severe risk factors and death was related to serious underlying comorbidities; given their immunosuppression status, it is possible that an inadequate immune response to the influenza vaccine had occurred. Moreover, Pregnancy was significantly associated with primary viral pneumonia due to An/H1N121 and it was recognized as important risk factor for developed severe hypoxemia. However, all pregnant women included in the present report were not vaccinated. No definitive conclusions can be drawn about the impact of vaccination based on our results given the small number of vaccinated patients included in the study. However, vaccinated patients seemed to have a more favorable outcome as evidenced by briefer stays in the ICU (4 days) and hospital (5 days) and fewer day under mechanical ventilation (5 days) (Table 1). Future studies are needed to clarify the impact of vaccination on outcome in critically ill patients.
The short follow up of the patients is a limitation of this study that should be further addressed. Indeed, the mortality rate in the present series could be underestimated given that 100 patients remained in the ICU at the time of this report, with a median follow up of 30 days in those patients. However, it is important to report in a timely manner our clinical experience with patients infected with the An/H1N1 virus to be aware of their clinical characteristics and possible differences with the previous 2009 outbreak, all of them pointing to a greater severity of illness and higher mortality as seen in the current series. In addition, early information on how recommendations on the management of critically ill patients with An/H1N1virus infection (i.e, on the use of antiviral agents or on the administration of corticosteroids) are being followed is of immediate practical relevance.
In conclusion, patients admitted to the ICU in the 2010-11 seasonal influenza outbreak appear to have a higher severity of illness, higher frequency of severe comorbidities, higher incidence of primary viral pneumonia and increased mortality compared with those observed in the 2009 pandemic outbreak. Hematological disease, severity of illness at ICU admission, number of quadrants infiltrates in chest X-ray and the requirement for mechanical ventilation were variables independently associated with mortality. Vaccination appears to be associated with improved outcomes. This report is aimed at providing a general description of the first An/H1N1 influenza patients admitted to Spanish ICUs. Further in-depth studies with a larger sample size are needed to confirm these preliminary results.
Conflict of interests
Authors declare no conflict of interests regarding the present manuscript.
Authors' contributions
AR assisted in the design of the study, coordinated patient recruitment, analyzed and interpreted the data, and with IML assisted in writing the paper. JB, PO, FAL, RZ, JG, JB, FG, JR made an important contribution to acquisition and analysis of data. JC, JL, IML and EC were involved in revising it critically for important intellectual content. CL, FP and AE made a substantial contribution to the conception and interpretation of data, and revised the final manuscript version. They all approved the final version to be published.
H1N1 SEMICYUC/REIPI/CIBERES Working Group investigators
Andalucía: Pedro Cobo (Hospital Punta de Europa, Algeciras); Javier Martins (Hospital Santa Ana Motril, Granada); Cecilia Carbayo (Hospital Torrecardenas, Almería); Emilio Robles-Musso, Antonio Cárdenas, Javier Fierro (Hospital del Poniente, Almería); Dolores Ocaña Fernández (Hospital Huercal, Overa, Almería); Rafael Sierra (Hospital Puerta del Mar, Cádiz); M. Jesús Huertos (Hospital Puerto Real, Cádiz); Juan Carlos Pozo, R. Guerrero (Hospital Reina Sofía, Córdoba); Enrique Márquez (Hospital Infanta Elena, Huelva); Manuel Rodríguez-Carvajal (Hospital Juan Ramón Jiménez, Huelva); Ángel Estella (Hospital del SAS de Jerez, Jerez de la Frontera); José Pomares, José Luis Ballesteros (Hospital Universitario San Cecilio, Granada); Yolanda Fernández, Francisco Lobato, José F. Prieto, José Albofedo-Sánchez (Hospital Costa del Sol, Marbella); Pilar Martínez; María Victoria de la Torre; María Nieto (Hospital Virgen de la Victoria, Málaga); Miguel Ángel Díaz Castellanos (Hospital Santa Ana de Motril, Granada); Guillermo Sevilla (Clínica Sagrado Corazón, Sevilla); José Garnacho-Montero, Rafael Hinojosa, Esteban Fernández (Hospital Virgen del Rocío, Sevilla); Ana Loza, Cristóbal León (Hospital Universitario Nuestra Señora de Valme, Sevilla); Ángel Arenzana (Hospital Virgen de la Macarena, Sevilla), Dolores Ocaña (Hospital de la Inmaculada, Sevilla); Inés Navarrete (Hospital Virgen de las Nieves, Granada); Medhi Zaheri Beryanaki (Hospital de Antequera); Ignacio Sánchez (Hospital NISA Sevilla ALJARAFE, Sevilla).
Aragón: Manuel Luis Avellanas, Arantxa Lander, S. Garrido Ramírez de Arellano, M.I. Marquina Lacueva (Hospital San Jorge, Huesca); Pilar Luque, Elena Plumed Serrano, Juan Francisco Martín Lázaro (Hospital Lozano Blesa, Zaragoza); Ignacio González (Hospital Miquel Servet, Zaragoza); Jose M. Montón (Hospital Obispo Polanco, Teruel); Paloma Dorado Regil (Hospital Royo Villanova, Zaragoza).
Asturias: Lisardo Iglesias, Carmen Pascual González (Hospital Universitario Central de Asturias [HUCA], Oviedo); Quiroga (Hospital De Cabueñes, Gijón); Águeda García-Rodríguez (Hospital Valle del Nalón, Langreo).
Baleares: Lorenzo Socias, Pedro Ibánez, Marcío Borges-Sa, A. Socias, A. Del Castillo (Hospital Son Llàtzer, Palma de Mallorca); Ricard Jordà Marcos (Clínica Rotger, Palma de Mallorca); José M. Bonell (USP, Clínica Palmaplanas, Palma de Mallorca); Ignacio Amestarán (Hospital Son Dureta, Palma de Mallorca).
Canarias: Sergio Ruiz-Santana, Juan José Díaz (Hospital Dr. Negrín, Las Palmas de Gran Canaria); Sisón (Hospital Doctor José Molina, Lanzarote); David Hernández, Ana Trujillo, Luis Regalado (Hospital General La Palma, La Palma); Leonardo Lorente (Hospital Universitario de Canarias, Tenerife); Mar Martín (Hospital de La Candelaria, Tenerife); Sergio Martínez, J.J. Cáceres (Hospital Insular de Gran Canaria).
Cantabria: Borja Suberviola, P. Ugarte (Hospital Universitario Marqués de Valdecilla, Santander).
Castilla-La Mancha: Fernando García-López (Hospital General, Albacete); Ángel Álvaro Alonso, Antonio Pasilla (Hospital General La Mancha Centro, Alcázar de San Juan); M. Luisa Gómez Grande (Hospital General de Ciudad Real, Ciudad Real); Antonio Albaya (Hospital Universitario de Guadalajara, Guadalajara); Alfonso Canabal, Luis Marina, (Hospital Virgen de la Salud, Toledo); Almudena Simón (Hospital Nuestra Señora del Prado, Toledo); José María Añón (Hospital Virgen de la Luz, Cuenca).
Castilla y León: Juan B. López Messa (Complejo Asistencial de Palencia, Palencia), M. Jesús López Pueyo, M.V. Ortiz (Hospital General Yagüe, Burgos); Zulema Ferreras (Hospital Universitario de Salamanca, Salamanca); Santiago Macias (Hospital General de Segovia, Segovia); José Ángel Berezo, Jesús Blanco Varela (Hospital Universitario Río Hortega, Valladolid), A. Andaluz Ojeda (Hospital Universitario, Valladolid); Antonio Álvarez Terrero (Hospital Virgen de la Concha, Zamora); Fabiola Tena Ezpeleta (Hospital Santa Bárbara, Soria); Zulema Páez, Álvaro García (Hospital Virgen Vega, Salamanca).
Cataluña: Rosa M. Catalán (Hospital General de Vic, Vic); Miquel Ferrer, Antoni Torres, Catia Cilloniz (Hospital Clínic, Barcelona); Sandra Barbadillo (Hospital General de Catalunya-CAPIO, Barcelona); Lluís Cabré, Ignacio Baeza (Hospital de Barcelona, Barcelona); Assumpta Rovira (Hospital General de L'Hospitalet, L'Hospitalet de Llobregat); Francisco Álvarez-Lerma, Antonia Vázquez, Joan Nolla (Hospital del Mar, Barcelona); Francisco Fernández, Joaquim Ramón Cervelló; Raquel Iglesia (Centro Médico Delfos, Barcelona); Rafael Mañez, J. Ballús, Rosa M. Granada (Hospital de Bellvitge, L'Hospitalet de Llobregat); Jordi Vallés, Marta Ortiz, C. Guía (Hospital de Sabadell, Sabadell); Fernando Arméstar, Joaquim Páez (Hospital Dos de Mayo, Barcelona); Jordi Almirall, Xavier Balanzo (Hospital de Mataró, Mataró); Jordi Rello, Elena Arnau, Marcos Pérez, César Laborda, Jesica Souto, Mercedes Palomar (Hospital Vall d'Hebron, Barcelona); Iñaki Catalán (Hospital Sant Joan de Déu, Manresa); Josep M. Sirvent, Cristina Ferri, Nerea López de Arbina (Hospital Josep Trueta, Girona); Mariona Badía, Montserrat Valverdú-Vidal, Fernando Barcenilla (Hospital Arnau de Vilanova, Lleida); Mònica Magret (Hospital Sant Joan de Reus, Reus); M.F. Esteban, José Luna (Hospital Verge de la Cinta, Tortosa); Juan M. Nava, J. González de Molina (Hospital Universitario Mútua de Terrassa, Terrassa); Zoran Josic (Hospital de Igualada, Igualada); Francisco Gurri, Paula Rodríguez (Hospital Quirón, Barcelona); Alejandro Rodríguez, Thiago Lisboa, Ángel Pobo, Sandra Trefler (Hospital Universitario Joan XXIII, Tarragona); Rosa María Díaz (Hospital San Camil, Sant Pere de Ribes, Barcelona); Eduard Mesalles (Hospital Germans Trias i Pujol, Badalona); Diego de Mendoza (Hospital M. Broggi, Sant Joan Despí).
Extremadura: Juliá-Narváez José (Hospital Infanta Cristina, Badajoz), Alberto Fernández-Zapata, Teresa Recio, Abilio Arrascaeta, M. José García-Ramos, Elena Gallego (Hospital San Pedro de Alcántara, Cáceres); Fernándo Bueno (Hospital Virgen del Puerto, Plasencia); Mercedes Díaz (Hospital de Mérida, Mérida).
Galicia: M. Lourdes Cordero, José A. Pastor, Luis Álvarez-Rocha (CHUAC, A Coruña); Dolores Vila (Hospital Do Meixoeiro, Vigo); Ana Díaz Lamas (Hospital Arquitecto Marcide, Ferrol); Javier Blanco Pérez, M. Ortiz Piquer (Hospital Xeral-Calde, Lugo); Eleuterio Merayo, Víctor José López-Ciudad, Juan Cortes Cañones, Eva Vilaboy, José Villar Chao (Complejo Hospitalario de Ourense, Ourense); Eva Maria Saborido (Hospital Montecelo, Pontevedra); Raul José González (H. Miguel Domínguez, Pontevedra); Santiago Freita, Enrique Alemparte, Ana Ortega (Complejo Hospitalario de Pontevedra, Pontevedra); Ana María López, Julio Canabal, Enrique Ferres (Clínica Universitaria Santiago de Compostela, Santiago).
La Rioja: José Luis Monzón, Félix Goñi (Hospital San Pedro, Logroño).
Madrid: Frutos Del Nogal Sáez, M. Blasco Navalpotro (Hospital Severo Ochoa, Madrid); M. Carmen García-Torrejón (Hospital Infanta Elena, Madrid); César Pérez-Calvo, Diego López (Fundación Jiménez Díaz, Madrid); Luis Arnaiz, S. Sánchez-Alonso, Carlos Velayos, (Hospital Fuenlabrada, Madrid); Francisco del Río, Miguel Ángel González (Hospital Clínico San Carlos, Madrid); María Cruz Martín, José M. Molina (Hospital Nuestra Señora de América, Madrid); Juan Carlos Montejo, Mercedes Catalán (Hospital Universitario 12 de Octubre, Madrid); Patricia Albert, Ana de Pablo (Hospital del Sureste, Arganda del Rey); José Eugenio Guerrero, María Zurita, Jaime Benitez Peyrat (Hospital Gregorio Marañón, Madrid); Enrique Cerdá, Manuel Álvarez, Carlos Pey (Hospital Infanta Cristina, Madrid); Montse Rodríguez, Eduardo Palencia (Hospital Infanta Leonor, Madrid); Rafael Caballero (Hospital de San Rafael, Madrid); Concepción Vaquero, Francisco Mariscal, S. García, (Hospital Infanta Sofía, Madrid); Nieves Carrasco (Hospital Universitario La Princesa, Madrid); Isidro Prieto, A. Liétor, R. Ramos (Hospital Ramón y Cajal, Madrid); Beatriz Galván, Juan C. Figueira, M. Cruz Soriano (Hospital La Paz, Madrid); P. Galdós, Bárbara Balandin Moreno (Hospital Puerta de Hierro, Madrid); Fernández del Cabo (Hospital Monte Príncipe, Madrid); Cecilia Hermosa, Federico Gordo (Hospital de Henares, Madrid); Alejandro Algora (Hospital Universitario Fundación Alcorcón, Madrid); Amparo Paredes (Hospital Sur de Alcorcón, Madrid); J.A. Cambronero (Hospital Universitario Príncipe de Asturias, Madrid); Sonia Gómez-Rosado (Hospital de Móstoles, Madrid); Luis Miguel Prado López (Hospital Sanitas La Zarzuela, Madrid); A. Esteban, J.A. Lorente, N. Nin (Hospital de Getafe, Madrid).
Murcia: Sofía Martínez (Hospital Santa María del Rosell, Murcia); F. Felices Abad (Hospital Universitario Reina Sofía, Murcia); Mariano Martínez (Hospital Universitario Virgen de la Arrixaca, Murcia); Sergio Manuel Butí, Bernardo Gil Rueda, Francisco García (Hospital Morales Messeguer, Murcia).
Navarra: Laura Macaya, Enrique Maraví-Poma, I. Jimenez Urra, L. Macaya Redin, A. Tellería (Hospital Virgen del Camino, Pamplona); Josu Insansti (Hospital de Navarra, Pamplona).
País Vasco: Nagore González, Pilar Marco, Loreto Vidaur (Hospital de Donostia, San Sebastián); B. Santamaría, Tomás Rodríguez (Hospital de Basurto, Bilbao); Juan Carlos Vergara, Jose Ramon Iruretagoyena Amiano (Hospital de Cruces, Bilbao); Alberto Manzano (Hospital Santiago Apóstol, Vitoria); Carlos Castillo Arenal (Hospital Txagorritxu, Vitoria); Pedro María Olaechea, Higinio Martín (Hospital Galdakao-Usansolo, Vizcaya).
Valencia: José Blanquer (Hospital Clinic Universitari, Valencia); Roberto Reig Valero, A. Belenger, Susana Altaba (Hospital General de Castellón, Castellón); Bernabé Álvarez-Sánchez (Hospital General de Alicante, Alicante); Santiago Alberto Picos (Hospital Torrevieja Salud, Alicante); Ángel Sánchez-Miralles (Hospital San Juan, Alicante); Juan Bonastre, M. Palamo, Javier Cebrian, José Cuñat (Hospital La Fe, Valencia); Belén Romero (Hospital de Manises, Valencia); Rafael Zaragoza, Constantino Tormo (Hospital Dr. Peset, Valencia); Virgilio Paricio (Hospital de Requena, Valencia); Asunción Marques, S. Sánchez-Morcillo, S. Tormo (Hospital de la Ribera, Valencia); J. Latour (H.G. Universitario de Elche, Valencia); M. Ángel García (Hospital de Sagunto, Castellón).
Andorra: Antoli Ribas (Hospital Nuestra Señora de Meritxell, Andorra).
Bibliografía
1. Pérez-Padilla R, De la Rosa-Zamboni D, Ponce de León S, Hernández M, Quiñones-Falconi F, Bautista E, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009; 361:680-9. [ Links ]
2. Rodríguez A, Socias L, Guerrero JE, Figueira JC, González N, Maraví-Poma E, et al, GETGAG/SEMICYUC (Spanish working Group on severe pandemic influenza A). Pandemic Influenza A in the ICU: Experience in Spain and Latin America. Med Intensiva. 2010; 34:87-94. [ Links ]
3. Nin N, Soto L, Hurtado J, Lorente JA, Buroni M, Arancibia F, et al. Clinical characteristics and outcomes of patients with 2009 influenza A(H1N1) virus infection with respiratory failure requiring mechanical ventilation. J Crit Care. 2010 Aug 3 [Epub ahead of print] PMID:20688465. [ Links ]
4. Rodríguez A, Lisboa T, Díaz E, Rello J, León C. From safety to prevention: A(H1N1) influenza, a new challenge for intensivits. Med Intensiva. 2009; 33:265-6. [ Links ]
5. Rello J, Rodríguez A, Ibañez P, Socias L, Cebrian J, Marques A, et al. Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1)v in Spain. Crit Care. 2009; 13:R148. [ Links ]
6. Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, et al. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009; 302:1872-9. [ Links ]
7. The ANZIC Influenza Investigators. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med. 2009; 361:1925-34. [ Links ]
8. Estenssoro E, Ríos FG, Apezteguía C, Reina R, Neira J, Ceraso D, et al. Pandemic 2009 Influenza A(H1N1) in Argentina: A Study of 337 Patients on Mechanical Ventilation. Am J Respir Crit Care Med. 2010; 182:41-8. [ Links ]
9. Martín-Loeches I, Rodríguez A, Bonastre J, Zaragoza R, Sierra R, Marques A, et al. Severe pandemic (H1N1)v influenza A infection. Report on the first death in Spain. Respirology. 2010 [Epub ahead of print]. doi:10.1111/j.1440-1843-2010.01874.x. [ Links ]
10. Martín-Loeches I, Sanchez-Corral A, Díaz E, Granada RM, Zaragoza R, Villavicencio C, et al. Community-acquired respiratory co-infection (CARC) in critically ill patients infected with pandemic 2009 influenza A (H1N1) virus infection. Chest. 2011; 139:555-62. [ Links ]
11. Bruneel F, Hocqueloux L, Alberti C, Wolff M, Chevret S, Bédos JP, et al. The clinical spectrum of severe imported falciparum malaria in the intensive care unit: report of 188 cases in adults. Am J Respir Crit Care Med. 2003; 167:684-9. [ Links ]
12. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388-416. [ Links ]
13. Díaz E, Rodríguez A, Martín-Loeches I, Lorente L, Del Mar Martín M, Pozo JC, et al. Impact of obesity in patients infected with new influenza A (H1N1)v. Chest. 2011; 139:382-6. [ Links ]
14. Rodríguez A, Díaz E, Martín-Loeches I, Sandiumenge A, Canadell L, Díaz JJ, et al. Impact of early oseltamivir treatment on outcome in critically ill patients with 2009 pandemic influenza A. J Antimicrob Chemother. 2011 [Epub ahead of print]. doi:10.1093/jac/dkq511. [ Links ]
15. Martín-Loeches I, Lisboa T, Rhodes A, Moreno RP, Silva E, Sprung C, et al. Use of early corticosteroid therapy on ICU admission in patients affected by severe pandemic (H1N1)v influenza A infection. Intensive Care Med. 2011; 37:272-83. [ Links ]
16. Hall MW. Inflammatory diseases of the respiratory tract (bronchitis, influenza, bronchopneumonia, lobar pneumonia). In: Communicable diseases, vol. IX. The Medical Department of the United States Army in the World War; 1928. Washington: The Surgeon General's Office (cited 2008 May 30). Available from: http://history.amedd.army.mil/booksdocs/wwi/communicablediseases/chapter2.1.htm. [ Links ]
17. Brundage JF. Interactions between influenza and bacterial respiratory pathogens: implications for pandemic preparedness. Lancet Infect Dis. 2006; 6:303-12. [ Links ]
18. Morens DM, Fauci AS. The 1918 influenza pandemic: insights for the 21st century. J Infect Dis. 2007; 195:1018-28. [ Links ]
19. McCullers JA. Insights into the interaction between influenza virus and pneumococcus. Clin Microbiol Rev. 2006; 19:571-82. [ Links ]
20. Bermejo-Martin JF, Ortiz de Lejarazu R, Pumarola T, Rello J, Almansa R, Ramirez P, et al. Th1 and Th17 hypercytokinemia as early host response signature in severe pandemic influenza. Crit Care. 2009; 13:R201. [ Links ]
21. Maraví-Poma E, Martin-Loeches I, Regidor E, Laplaza C, Cambra K, Aldunate S, et al. Severe 2009 H1N1 influenza in pregnant women in Spain. Crit Care Med. 2011 [Epub ahead of print]. PMID:212633317. [ Links ]
![]() Correspondence:
Correspondence:
Correo electrónico: ahr1161@yahoo.es
(A. Rodríguez)
Received 8 March 2011
Accepted 10 March 2011














