Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Intensiva
versión impresa ISSN 0210-5691
Med. Intensiva vol.36 no.6 ago./sep. 2012
https://dx.doi.org/10.1016/j.medin.2011.10.010
Transpulmonary thermodilution curve and the cross-talk phenomenon
Curva de termodilución transpulmonar y el fenómeno cross-talk
The transpulmonary thermodilution (TPTD) operates via a single thermal indicator technique to determine cardiac index (CI), and derivatives volumetric variables.1 The impact of shunt on CI and volumetric variables derived from TPTD curve has already been studied.2,3 However, other TPTD signal artifacts have also already been evoked,4,5 but their real impact on CI was never established.6 The present case report describes the impact of a cross-talk phenomenon on the TPTD curve and CI measurement values when the technique was assessed using a femoral central venous access in a critically ill patient.
The IRB of Geneva University Hospitals determined that permission is not required for this report. However, permission to present the case was obtained from the patient. A previously healthy 19-year-old man was admitted to our hospital for the management of an acute ischemic stroke following a low-energy skiing accident. The patient initially developed diplopia and unsteady gait, rapidly followed by loss of consciousness. He was intubated on-site and taken to the emergency room. The cerebral CT-scan on admission showed a large hypodense lesion concerning both cerebellar hemispheres, predominantly on the right side, as well as a lesion of the left thalamus, consistent with ischemic stroke. There were signs of tonsillar engagement and compression of the fourth ventricle. Traumatic dissection of the right vertebral artery was suspected. An occipital craniectomy was urgently performed and an external ventricular drain inserted. Postoperatively the patient was transferred to the intensive care unit for ongoing care. Forty-eight hours later a partial cerebellectomy was carried out in order to control elevation of intracranial pressure.
Since a vasopressor therapy with norepinephrine was intermittently necessary to maintain cerebral perfusion pressure and the patient presented a severe sepsis related to a sinusitis, we established an advanced hemodynamic monitoring using a TPTD curve technique (PiCCOTM, Pulsion Medical Systems, Munich, Germany). A left femoral central venous catheter (ARROW international, 7F, 3 lumen, USA,) of 20cm length was already in place since admission to avoid jugular or subclavian veins injuries and to optimize cerebral hemodynamics of a neurosurgical patient. Thus, we inserted a 20-cm-long PiCCOTM catheter (Pulsiocath; PiCCOTM, Pulsion Medical Systems, Munich, Germany) in the right femoral artery using Seldinger's technique in order to complete the device setup (Figure 1).

Figure 1. The transpulmonary thermodilution (TPTD) curve prior to draw back the right femoral PiCCOTM catheter.
Please note that the TPTD curve is characterized by a premature as well as a late peak with
a dilution appearing large and biphasic (CI value=1.15Lmin-1m-2).
The thermodilution curves initially observed appeared early and biphasic ("camel-curve" type, Figure 1), with an incomprehensibly low CI, when compared to the normal CI value obtained by echocardiography Doppler. Regarding the present situation, the requested attending physician assumed that the close and matched positioning of venous and arterial femoral catheters of equal length (20cm) was responsible for the arising of a signal interference (known as cross-talk phenomenon). To resolve the present artifact, he asked the resident to draw back the right femoral PiCCOTM catheter by 8cm (Figure 2). Following this repositioning of the PiCCOTM catheter, we observed a common TPTD curve with normal uniphasic shape, signal delay and CI value (Figure 2).
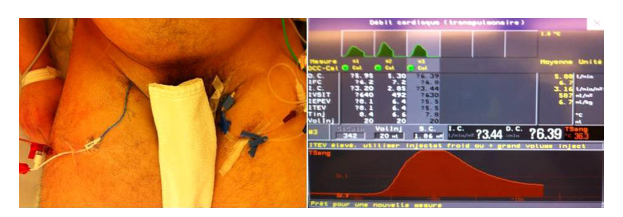
Figure 2. The transpulmonary thermodilution (TPTD) curve after the right femoral PiCCOTM catheter
has been repositioned. Please note that the premature peak disappeared with a dilution
appearing normal and less large (CI value=3.44Lmin-1m-2).
Venous-arterial thermodilution artifacts may be responsible for an early detection of the thermal indicator. As far as we know, this is the first observation of an early and biphasic "camel-curve" type, related to the anatomical contiguity of large vessels impacting CI values (Figure 1).
The TPTD is a hemodynamic monitoring system gaining recognition and wide usage in the intensive care setting.7 It operates via a single thermal indicator technique to determine extra vascular lung water, cardiac output, and volumetric variables. In our case, CI measurements were obtained after central venous injections of 20ml of cooled (4oC) 0.9% saline via the femoral approach while the thermistor tip on the femoral artery catheter measured the downstream temperature change within the arterial system.8 Cardiac output was then calculated by analysis of the temperature change of the TPTD curve using the Stewart-Hamilton method.
Schmidt and colleagues studied the effect of the femoral venous catheter site on TPTD variables and found that the TPTD curve obtained by a cold saline bolus provides clinically reliable CI and extravascular lung water index values.8 In this interesting study the length of the venous catheters used was not provided in the article.5 However, the authors acknowledged this limitation and affirmed that central venous catheters were longer (length of 30cm) than the PiCCOTM arterial catheter (length of 20cm) and all TPTD curves had a normal shape.9
In the present case, CI values were abnormally low before the right femoral PiCCOTM catheter was withdrawn by 8cm (Figure 1 and Figure 2). This finding is rational as, in this setting; one part of the cold saline solution injected through the femoral venous catheter induced significant temperature changes in the close artery (vessels contiguity). This phenomenon produced a curve appearing large and biphasic shaped by a premature as well as a late peak. The time interval between the two peaks was necessarily longer than a right-to-left intracardiac shunt related to an atrial septal defect,2 since the late peak represents the authentic blood transit time of the TPTD curve (Figure 1 and Figure 2). As the thermal bolus is detected twice (early artifact and expected detection) the area under the curve of TPTD curve was larger and consequently the CI lower. The detection of a common TPTD curve with CI values closely reflecting the patient cardiac function once the arterial catheter had been isolated from the injection site, clearly support our assumption.
In clinical practice, when treating neurosurgical critically ill patients, the use of a femoral central venous catheter is a secure approach as the present line position does not affect jugular venous return and potentially intracranial pressure. However, like in our case, the use of a femoral venous catheter longer than the femoral artery catheter is recommended to avoid a cross-talk phenomenon and its impact on CI values.
R. Keller, N. Goettel, K. Bendjelid
Intensive Care Service, Geneva University Hospitals, Geneva, Switzerland
Bibliografía
1. Bendjelid K, Giraud R, Siegenthaler N, Michard F. Validation of a new transpulmonary thermodilution system to assess global end-diastolic volume and extravascular lung water. Crit Care. 2010; 14:R209. [ Links ]
2. Giraud R, Siegenthaler N, Park C, Beutler S, Bendjelid K. Transpulmonary thermodilution curves for detection of shunt. Intensive Care Med. 2010; 36:1083-6. [ Links ]
3. Michard F, Alaya S, Medkour F. Monitoring right-to-left intracardiac shunt in acute respiratory distress syndrome. Crit Care Med. 2004; 32:308-9. [ Links ]
4. Michard F. Looking at transpulmonary thermodilution curves: the cross-talk phenomenon. Chest. 2004; 126:656-7. [ Links ]
5. Bendjelid K. Avoiding the cross-talk phenomenon when assessing cardiac output using the transpulmonary thermodilution technique via the femoral vein access. Crit Care Med. 2007; 35:2670. [author reply] [ Links ].
6. Cole RP. Interpretation of transpulmonary thermodilution curves. Chest. 2005; 127:1459-60. [author reply 60] [ Links ].
7. Hamzaoui O, Monnet X, Richard C, Osman D, Chemla D, Teboul JL. Effects of changes in vascular tone on the agreement between pulse contour and transpulmonary thermodilution cardiac output measurements within an up to 6-hour calibration-free period. Crit Care Med. 2008; 36:434-40. [ Links ]
8. Schmidt S, Westhoff TH, Hofmann C, Schaefer JH, Zidek W, Compton F, et al. Effect of the venous catheter site on transpulmonary thermodilution measurement variables. Crit Care Med. 2007; 35:783-6. [ Links ]
9. Schmidt S, Westhoff TH, Compton F, Zidek W, van der Giet M. Avoiding the cross-talk phenomenon when assessing cardiac output using the transpulmonary thermodilution technique via the femoral vein access. Crit Care Med. 2007; 35:2670. [ Links ]
![]() Correspondence:
Correspondence:
Karim.Bendjelid@hcuge.ch
(K. Bendjelid).












 Curriculum ScienTI
Curriculum ScienTI

