Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nefrología (Madrid)
versión On-line ISSN 1989-2284versión impresa ISSN 0211-6995
Nefrología (Madr.) vol.33 no.2 Cantabria 2013
https://dx.doi.org/10.3265/Nefrologia.pre2012.Oct.11188
DOI: 10.3265/Nefrologia.pre2012.Oct.11188
ORIGINALES
Study of nephrotic syndrome in children: Importance of light, immunoflourescence and electron microscopic observations to a correct classification of glomerulopathies
Estudio del síndrome nefrótico infantil: importancia de las observaciones microscópicas de luz, inmunofluorescencia y electrones para una correcta clasificación de las glomerulopatías
Muhammed Mubarak, Javed Kazi
Histopathology Department. Sindh Institute of Urology and Transplantation (SIUT). Karachi, Sindh (Pakistan)
ABSTRACT
Objective: To evaluate the contribution of electron microscopy (EM) to the accurate diagnosis of glomerulopathies in childhood nephrotic syndrome (NS) in a developing country.
Methods: The study was carried out at the Histopathology Department, Sindh Institute of Urology and Transplantation (SIUT) from April 2007 to March 2008. All children (≤18 years) presenting with NS were included. Patients' demographic, clinical, laboratory, and biopsy data were retrieved from case records and biopsy reports. Renal biopsies were studied by light microscopy, immunoflourescence, and EM.
Results: The mean age of 74 children was 11.34±4.85 years. EM was useful in 97.2% of cases, being essential in 31% and helpful in 66.2% cases.
Conclusion: The results demonstrate that the ultrastructural study is both helpful and essential to a correct classification of glomerular diseases underlying NS in children in nearly all cases and whenever feasible this should be used in the pathologic evaluation of renal biopsies.
Key words: Children, Nephrotic syndrome, Renal biopsy, Morphological patterns, Ultrastructural study.
RESUMEN
Objetivo: Evaluar la contribución de la microscopía electrónica (ME) al diagnóstico preciso de las glomerulopatías en el síndrome nefrótico (SN) infantil en un país en vías de desarrollo.
Método: El estudio se realizó en el Departamento de Histopatología del Instituto Sindh de Urología y de Trasplante (SIUT) desde abril de 2007 a marzo de 2008. En él se incluyeron todos los niños (≤ 18 años) que presentaban SN. Los datos demográficos, clínicos, de laboratorio y de la biopsia de los pacientes se obtuvieron a partir de expedientes de casos e informes de la biopsia. Las biopsias renales se estudiaron mediante microscopía de luz, inmunofluorescencia y ME.
Resultados: La media de edad de 74 niños era de 11,34 ± 4,85 años. La ME resultó útil en el 97,2 % de los casos, siendo esencial en el 31 % y constituyendo una ayuda en el 66,2 % de los casos.
Conclusión: Los resultados demuestran que el estudio ultraestructural es de utilidad y resulta esencial para la correcta clasificación de las enfermedades glomerulares subyacentes al SN infantil en casi todos los casos; por lo tanto, debería utilizarse en la evaluación patológica de biopsias renales siempre que fuera posible.
Palabras clave: Niños, Síndrome nefrótico, Biopsia renal, Patrones morfológicos, Estudio ultraestructural.
Introduction
Diagnostic renal pathology is an integrative process, wherein an accurate diagnosis of glomerular diseases, requires a correlative approach incorporating the clinical data, the serologic tests and the complete pathologic evaluation of renal biopsy by light microscopy (LM), immunoflourescence (IF), and electron microscopy (EM).1,2 The ultrastructural examination has been used for the accurate diagnosis of glomerulopathies for more than four decades, and its diagnostic value is well established in this subspecialty of diagnostic pathology.3-18 More recently, its routine use in renal biopsies has come under critical appraisal in view of its prohibitive cost and technician- intensive nature, with variable results reported by different researchers.12-15 Most of these studies have been conducted in developed countries and in adult patients. Only few studies are available on the current position of EM in the investigation of renal biopsies in developing countries and still fewer, on the utility of EM in the study of childhood renal diseases.14,16-18 EM facility, with its huge initial and maintenance costs, is found only in a few centers in most of the developing countries or not at all. Pakistan too, being a developing country, lacks widespread availability of EM facilities.8-10 However, Histopathology laboratory at Sindh Institute of Urology and Transplantation (SIUT) is equipped with all the necessary diagnostic modalities required for the accurate evaluation of renal biopsies, including IF and EM. In recent reviews of completely worked-up renal biopsies in patients with nephrotic syndrome (NS), we have found that the pattern of glomerular diseases, in both the children and the adults, is more akin to that reported recently in developed parts of the world, rather than the tropical pattern reported in earlier studies from Pakistan.8,9,19,20 It is of note, that the later studies were based on LM study of renal biopsies only. We have earlier reported on the role of IF and EM in the evaluation of renal biopsies in NS in a study that included both the children and the adults.10 In that study, we did not attempt to evaluate separately the role of EM for either the adults or the children. Since, age is an important determinant of the glomerular lesions underlying NS and the lesions differ markedly among the children and the adults, we contemplated to evaluate the relevance of ultrastructural study in the accurate evaluation of renal biopsies of the glomerulopathies underlying NS in children from Pakistan.
Materials and methods
This was a descriptive, observational study carried out at the Department of Histopathology, Sindh Institute of Urology and Transplantation (SIUT) from April 2007 to March 2008. The study was approved by the ethical review committee of SIUT. Seventy four consecutive children (≤18 years) with NS and in whom adequate renal biopsy material was available for LM, IF and EM examination, were included in the study. Renal allograft biopsies as well as native renal biopsies performed for other indications, such as, acute renal failure (ARF) were excluded. Patients' demographic, clinical and laboratory data, including age, sex, renal functions and 24-h urinary protein were retrieved from case files. LM, IF, EM findings and final diagnosis was retrieved from original renal biopsy reports.
Renal Biopsies: Renal biopsies were undertaken in all cases using Tru-cut needle under ultrasound guidance after obtaining informed consent from patients or their parents. Two cores were obtained in each case, one for LM and other for IF and EM examination. The renal biopsies were processed for LM examination according to established protocols, as described in detail in our earlier study.10
LM: For LM, routinely 10 serial sections are cut and stained by hematoxylin and eosin (H&E), Masson's trichrome, periodic acid-Schiff (PAS) and silver methenamine stains. Further special stains were done, if needed.
IF: Tissue specimens were snap-frozen, sections cut and stained by fluorescein isothiocynate (FITC)-conjugated antisera specific for IgG, IgA, IgM, C3, and C1q (Dako, Glostrup, Denmark). Staining reactions were graded semiquantitatively as 0 to 3+ and distribution described as membranous or mesangial in a granular or linear pattern, as described previously.10
EM: Tissue samples for EM were processed according to established techniques.10 Briefly, EM tissue was fixed in 4% glutaraldehyde, postfixed in 1% osmium tetroxide at 0.02 M Sorenson Phosphate buffer at pH 7.4, processed for electron microscopy and embedded in Eponate resin (PELCO International, Redding, CA, USA). Ultra-thin sections (100nm) were cut on Leica ultramicrotome. Sections were stained with Uranyl acetate and Lead citrate and examined with a JEM 1200 EX II electron microscope (JEOL, Tokyo, Japan). The diagnostic role of the EM study was considered essential if the final diagnosis could not have been reached in the absence of EM study. The contribution was considered helpful in cases, in which, although the diagnosis could have been reached based on the combined LM and IF studies, the EM confirmed the diagnosis, especially by excluding diagnoses based exclusively on EM findings. EM study was considered noncontributory if the final diagnosis could have been reached with out it.10
Final Diagnosis: The final correlative diagnosis of glomerular diseases was based on renal biopsy findings by LM, IF and EM and the correlation of these pathologic findings with the clinical, laboratory and serological results. Established diagnostic criteria were used for the diagnosis of specific glomerular diseases.11
Data analysis
Data was analyzed using the Statistical Package for Social Sciences (SPSS) version 10 computer program (SPSS, Chicago, IL, USA). Descriptive statistics such as mean ±SD were used for continuous variables and numbers (percentages) for categorical data.
Results
The demographic characteristics of 74 children showed the mean age of 11.34±4.85 years (range: 2-18 years). There were 38 (51.4%) males and 36 (48.6%) females, with a male-to-female ratio of 1.65:1. All children presented with NS. The mean 24-h urinary protein excretion was 4.73±0.84g (range: 3.3-6.9g). The mean serum albumin was 1.7±0.7g/100ml (range: 0.6-3.8g). Hematuria was detected in 15 (20.2%) cases. Positive antinuclear antibody (ANA) test was found in 8 (10.8%) cases and anti-dsDNA in none. Low complement factor C3 was found in 17 (22.9%) cases and low C4 in 12 (16.2%) cases. Hepatitis B surface antigen (HBsAg) and anti-hepatitis C virus (HCV) was detected in one case each. Anti-streptolysin O (ASO) titer was elevated in two cases.
The morphological patterns observed on LM in all children with NS are shown in Table 1. As is evident, the focal and segmental sclerosing lesion was the most common morphological pattern, followed by minor changes and mesangial proliferative pattern. These three patterns together accounted for 85% of all the morphological patterns observed on LM in children with NS. Other morphological appearances were rare. The final diagnoses arrived at by combining the LM, IF and EM studies with the clinical and the serological results, are shown in Table 2. It is apparent from these tables that the morphological patterns of glomerular injury as seen on LM are not synonymous with the final diagnoses, the later can only be reached by a correlative approach combining information from LM, IF and EM study with the clinical, laboratory and serological data. Regarding the specific diseases, it is apparent that FSGS is the most common disease in children presenting with NS, followed by minimal change disease (MCD) and IgM nephropathy (IgMN). Finally, the contribution of the EM study of renal biopsies to the final diagnostic categories is shown in Table 3. This clearly shows that the EM study is useful in a vast preponderance of cases of glomerular diseases in childhood NS.
Table 1. Morphologic findings observed on light microscopy in renal biopsies in 74 children
with idiopathic nephrotic syndrome. 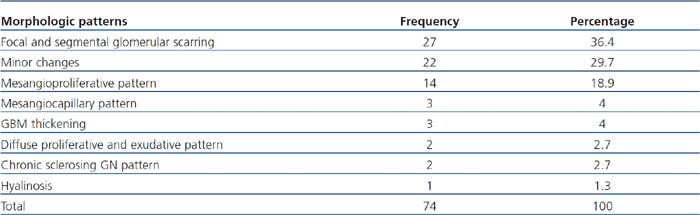
GBM: glomerular basement membrane.
Table 2. Final diagnosis based on correlating LM, IF and EM with clinical and serologic
findings in 74 children with nephrotic syndrome. 
EM: electron microscopy; GN: glomerulonephritis; IF: immunofluorescence; LM: light microscopy.
Table 3. Contribution of electron microscopic study to the final diagnosis of glomerular diseases
in 74 children with nephrotic syndrome. 
GN: glomerulonephritis.
Discussion
The current study is an important contribution to the field of pediatric nephropathology for several reasons; it is the first study from any developing country and from Pakistan on this subject and the second to the only published study from USA on children presenting with NS.14 Moreover, to our knowledge, it is the largest study ever reported on the role of ultrastructural study in the pathologic evaluation of renal biopsies in childhood NS. The previously mentioned, and the exclusive, study on this subject from the USA had included 48 children.14
Overall, the EM study was useful in 97.2% of cases, being essential in 31% and helpful in 66.2% cases of childhood NS. It was noncontributory in only 2.7% cases. These results show that the EM study is more useful in children with NS in comparison to adults. Studies performed in adults have concluded that EM evaluation contributed significantly to the final diagnosis of 50% consecutive renal biopsies.12 When compared with a study from US evaluating the contribution of EM to the final diagnosis of childhood NS, our results are concordant with that study.14 The later study found ultrastructural examination useful in all cases and essential in 73% of cases.14 The contribution was not identical in all cases, however, being essential in some cases and helpful in others,14 a finding similar to that found in our study.
Regarding specific diseases, the findings from the current study demonstrate that FSGS is the leading cause of NS in this cohort of children. This is concordant with several recent studies from around the world, which show that the incidence of this lesion is on the rise in children with NS9. In our previous analysis of percutaneous native renal biopsies over 14 year period, this lesion closely followed MCD in children as a cause of idiopathic NS (INS).9 In that study, we did not analyze the changing trends of the glomerular disease over the study period. The evidence from the current study suggests that FSGS has likely surpassed MCD as the leading cause of INS in the pediatric population, as reported previously in the adults from our center.8 However, it is worth mentioning here that the biopsy indications in the present study included all cases of NS as compared to the INS in the former study.9 This along with a small size of the sample may have influenced the results of the current study. The diagnosis of FSGS is primarily based on morphological findings on LM, but the EM study, like IF, was helpful in all cases of FSGS in confirming the widespread loss of foot processes of the podocytes and in excluding the secondary causes of FSGS.
MCD was the second most frequent lesion underlying NS in children in this study. It used to be the leading cause of INS in children, but many researchers have found a declining prevalence of this lesion throughout the world in recent years.9 The EM study was essential for the diagnosis of this disease, in that it demonstrated the most important morphological lesion of the disease, i.e., the fusion of foot processes. Although, the diagnosis of MCD can be suspected on LM and IF examinations, it is only the EM study that conclusively establishes its diagnosis, as shown in Figure 1. We acknowledge the fact the potential role of EM in establishing a diagnosis of MCD in a pediatric population is not without controversy, especially, in the perspective of developing countries. The definitions of essential and helpful roles of EM have been derived from studies done in developed countries, and may not be equally relevant for resource constrained developing countries. It could be argued that children presenting with nephrotic-range proteinuria and a normal appearing renal biopsy on LM could be presumed to have MCD. By this argument, EM would not be essential in establishing a diagnosis of MCD. Nevertheless, standard of care in Western countries would dictate that EM is deemed essential.

Figure 1. Portions of two capillary loops showing extensive fusion
of foot processes in a case of minimal change disease.
Glomerular basement membrane is normal. No electron dense deposits are seen.
(Transmission electron microscopy, uranyl acetate and lead citrate, x 8,000)
IgMN has also emerged as an important cause of idiopathic NS in children in our part of the world.9,21 EM was helpful in cases of IgMN in children by excluding other potential causes of NS and in demonstrating mesangial expansion and electron dense deposits in the mesangium. Similar arguments also hold true for the usefulness of EM in cases of IgA nephropathy (IgAN), occasionally presenting with NS in children.
Lupus nephritis (LN) is an important cause of renal morbidity and mortality in older children and teenagers.22 The diagnosis and clinical management of patients with LN can be a challenge from a clinicopathological point of view. Correlating the LM, IF, and EM findings within the clinical context of LN is essential for the optimal clinical management. In some of these patients, the EM study provides the key information that can not be otherwise obtained.23 We found the EM study helpful in all cases of LN in the children presenting with NS, as reported in previous studies.23
The two other groups of glomerular diseases for which the EM study was essential were the mesangiocapillary GN (MPGN) and the hereditary glomperulopathies. EM is essential for the accurate categorization of the subtypes of MPGN, as shown in Figure 2. Similarly, EM study is essential for the correct diagnosis of all cases of hereditary glomerular diseases.10 We found one case each of Alport's syndrome (Figure 3) and tthin basement membrane disease (TBMD) in this series. It is interesting to note that TBMD typically does not cause NS, but occasional cases have been described with nephrotic range proteinuria.24 Additionally, the diagnosis of TBMD can not be based solely on morphological criteria, as many cases of Alport's syndrome, can present with this phenotype. Genetic and pedigree analysis can resolve the differential in such cases. No family history was available of renal disease in our case and genetic testing could not be done due to non-availability of this facility.
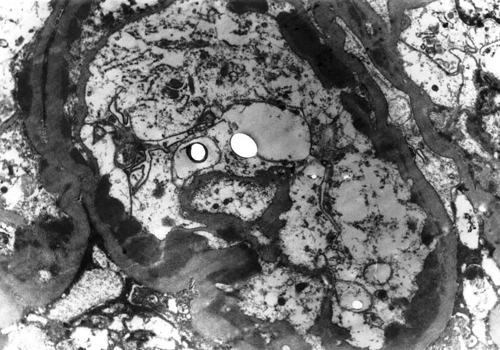
Figure 2. Peripheral capillary loops showing numerous electron dense deposits in
subendothelial location in a case of mesangiocapillary glomerulonephritis, type I.
(Transmission electron microscopy, uranyl acetate and lead citrate, ×10,000)

Figure 3. Medium magnification view of glomerular basement membrane (GBM)
showing focal thickening and rarefaction of the lamina densa of the GBM in
a case of Alport syndrome.
Foot processes are partially fused. (Transmission electron microscopy, uranyl
acetate and lead citrate, x 25,000)
In conclusion, the findings from this study show that the EM study is both helpful and essential in the diagnosis of the specific glomerulopathies causing NS in children in nearly all cases and should be employed routinely in the pathologic investigation of renal biopsy material whenever possible or at least the tissue for such study procured and preserved appropriately. The contribution of the ultrastructural study to the investigation of the renal biopsies in childhood NS in a developing country like Pakistan is as pertinent as in the developed countries. In the developing countries, establishment of national reference renal pathology laboratories with the EM facilities, may be a feasible option where the renal samples from other laboratories can be sent for analysis, till such facilities are widely available.
Acknowledgements
We acknowledge with gratitude the help and efforts of Dr. Syed Wajahat Ali Rizvi, EM consultant, and Perveen Akhter, EM technologist, in obtaining the EM data in time.
Conflicts of interest
The authors declare that there is no conflict of interest associated with this manuscript.
References
1. Furness PN, Kazi JI. Laboratory investigation of renal biopsy specimen. J Nephrol Urol Transplant 1998;1:19-26. [ Links ]
2. Turner DR. Advances in understanding the morphology of glomerular disease. J Clin Pathol 1981;34:1207-13. [ Links ]
3. Furness PN, Boyd S. Electron microscopy and immunocytochemistry in the assessment of renal biopsy specimens: actual and optimal practice. J Clin Pathol 1996;49:233-7. [ Links ]
4. Furness PN. ACP Best Practice No. 160. Renal biopsy specimens. J Clin Pathol 2000;53:433-8. [ Links ]
5. Tighe JR, Jones NF. The diagnostic value of routine electron microscopy of renal biopsies. Proc Roy Soc Med 1970;47:126-8. [ Links ]
6. Spargo BH. Practical use of electron microscopy for the diagnosis of glomerular disease. Hum Pathol 1975;6:405-20. [ Links ]
7. Dische FE, Parsons V. Experience in the diagnosis of glomerulonephritis using combined light microscopical, ultrastructural and immunofluorescence techniques-an analysis of 134 cases. Histopathology 1977;1:331-62. [ Links ]
8. Kazi JI, Mubarak M, Kazi JI, Mubarak M, Ahmed E, Akhter F, et al. Spectrum of glomerulonephritides in adults with nephrotic syndrome in Pakistan. Clin Exp Nephrol 2009;13:38-43. [ Links ]
9. Mubarak M, Lanewala A, Kazi JI, Akhter F, Sher A, Fayyaz A, et al. Histopathological spectrum of childhood nephrotic syndrome in Pakistan. Clin Exp Nephrol 2009;13:589-93. [ Links ]
10. Mubarak M, Kazi JI. Role of immunoflourescence and electron microscopy inthe evaluation of renal biopsies in nephrotic syndrome in a developing country. Ultrastruct Pathol 2009;33:260-4. [ Links ]
11. Churg J, Bernstein J, Glassock RJ. Renal disease: Classification and atlas of glomerular disease. 2nd ed. New York: Igaku-Shoin;1995. p. 1-359. [ Links ]
12. Haas MA. Reevaluation of routine electron microscopy in the examination of native renal biopsies. J Am Soc Nephrol 1997;8:70-6. [ Links ]
13. Pearson JM, McWilliam LJ, Coyne JD, Curry A. Value of electron microscopy in diagnosis of renal disease. J Clin Pathol 1994;10:209-15. [ Links ]
14. Rivera A, Magliato S, Meleg-Smith S. Value of electron microscopy in the diagnosis of childhood nephrotic syndrome. Ultrastruct Pathol 2001;25:313-20. [ Links ]
15. Collan Y, Hirsimaki P, Aho H, Wuorela M, Sundsrtrom J, Tertti R, et al. Value of electron microscopy in kidney biopsy diagnosis. Ultrastruct Pathol 2005;29:461-8. [ Links ]
16. Wagrowska-Danilewicz M, Danilewicz M. Current position of electron microscopy in the diagnosis of glomerular diseases. Pol J Pathol 2007;58:87-92. [ Links ]
17. Sementilli A, Moura LA, Franco MF. The role of electron microscopy for the diagnosis of glomerulopathies. Sao Paulo Med J 2004;122:104-9. [ Links ]
18. Elhefnawy NG. Contribution of electron microscopy to the final diagnosis ofrenal biopsies in Egyptian patients. Pathol Oncol Res 2010;17:121-5. [ Links ]
19. Jamal Q, Jafarey NA, Naqvi AJ. A review of 1508 percutaneous renal biopsies. J Pak Med Assoc 1988;38:272-5. [ Links ]
20. Muzaffar M, Mushtaq S, Khadim MT, Mamoon N. Morphological pattern of glomerular diseases in patients with nephrotic syndrome in Northern Pakistan.Pak Armed Forces Med J 1997;47:3-6. [ Links ]
21. Mubarak M, Kazi JI, Malik S, Lanewala A, Hashmi S. Clinicopathologic characteristics and steroid response of IgM nephropathy in children presenting with idiopathic nephrotic syndrome. APMIS 2011;119:180-6. [ Links ]
22. Marks SD, Sebire NJ, Pilkington C, Tullus K. Clinicopathological correlations of paediatric lupus nephritis. Pediatr Nephrol 2007;22:77-83. [ Links ]
23. Herrera GA. The value of electron microscopy in the diagnosis and clinical management of lupus nephritis. Ultrastruct Pathol 1999;23:63-77. [ Links ]
24. Voskarides K, Damianou L, Neocleous V, Zouvani I, Christodoulidou S, Hadjiconstantinou V, et al. COLA3/COLA4 mutations producing focal segmental glomerulosclerosis and renal failure in thin basement membrane nephropathy. J Am Soc Nephrol 2007;18:3004-16. [ Links ]
![]() Correspondence:
Correspondence:
Muhammed Mubarak
Histopathology Department
Sindh Institute of Urology and Transplantation (SIUT)
74200, Karachi, Sindh, Pakistan
E-mail: drmubaraksiut@yahoo.com
E-mail: drmubaraksiut@gmail.com
Enviado a Revisar: 6 Oct. 2011
Aceptado el: 29 Oct. 2012














