INTRODUCTION
The small-bowel accomplishes complex and intricate absorptive, digestive, defense, neuromotor, endocrine and metabolic functions. It is the largest endocrine organ and produces peptides that regulate the metabolism of glucose; appetite and food ingestion; gastric, biliary and pancreatic secretions; gastrointestinal motility and immune function (1,2). The Gut-associated Lymphoid Tissue (GALT) is one of the largest lymphoid organs, containing up to 70% of the body's total number of immune cells, and the inductor for the mucosal-associated lymphoid tissue (MALT) 2,3. Furthermore, small-bowel plays a central role in pathophysiology of the systemic inflammatory response and multiple organ dysfunction syndromes in the critical illness 4.
The definition of acute gastrointestinal injury in the critically ill patients remains challenging 5,6. Nevertheless, small-bowel dysfunction is considered to exert a relevant adverse impact on the prognosis and to be frequently unrecognized in this context 6,7. As previously reported, 60.2% of critically ill patients evidenced one or more gastrointestinal symptoms during the first week of intensive care unit (ICU) admittance, including high gastric residual volumes, absent bowel sounds, vomiting or regurgitation, diarrhea, bowel distention and gastrointestinal bleeding 8; and 58.3% developed enteral nutrition intolerance 9. Reintam A et al. 8 verified that the gastrointestinal failure, defined by the association of three or more gastrointestinal symptoms on the first day in ICU, was present in 4.8% of the patients and was independently associated with a threefold increased risk of mortality. In their study, during the first week in ICU, gastrointestinal failure occurred in 6.4% of patients and was associated with higher 28-day mortality (62.5 versus 28.9%, p = 0.001) (8). According Reintam A et al. 9, the development of gastrointestinal failure, described by a five-grade scoring system based on food intolerance and intra-abdominal hypertension, in the first three days of the ICU stay, was an independent risk factor for ICU and 90-day mortality.
Citrulline is a non-protein amino acid that results from the enterocyte mitochondrial metabolism of glutamine, particularly in the proximal small bowel, at the upper and medium part of the villi 10,11. Citrulline participates in the adaptation to the variations of the protein ingestion and in the nitric oxide production 10,12. After its synthesis, regulated by pyrroline 5-carboxylate synthase, an enzyme almost exclusive of the enterocytes, citrulline is released in the portal circulation and converted to arginine in the kidneys. Therefore, the intestine represents the main source of circulating citrulline 10,11.
Citrullinemia has been recognized an objective, quantitative, reproducible and simple parameter of the functional enterocyte mass 10,12,13 and proposed as a biomarker of acute intestinal failure in the critically ill patients 6,12,13.
The present study intends to determine the prevalence of intestinal dysfunction and the kinetic profile of citrullinemia in severe trauma patients and to evaluate its correlation with the severity indicators and clinical outcome.
METHODS
A prospective observational cohort study of adult critical trauma patients admitted in the Intensive Care Unit (ICU) of a tertiary university hospital was accomplished between October 2013 and April 2014. Recruitment of trauma patients was based on the Intensive Care Society definition of critically illness 14 and the prediction of an ICU length of stay not inferior to three days. Rejection factors were pregnancy, lactation, acquired immunodeficiency syndrome, renal insufficiency (creatininemia ≥ 2 mg/dL), acute liver failure (conforming to previous definitions) 15,16, amino acid metabolism diseases, chronic gut disorders and previous enterectomy.
Study was ratified by the institution's ethics committee and adhered to the principles of the Helsinki's declaration 17.
Patients' age, gender and type of admission (primary or after initial treatment on other hospital) were registered. Severity scores were recorded at the admittance, including Acute Physiology and Chronic Health Evaluation II (APACHE II) score 18, Simplified Acute Physiology Score II (SAPS II) 19, Sequential Organ Failure Assessment (SOFA) score 20, Injury Severity Score 21, Revised Trauma Score 22 and Shock Index 23. Mechanical ventilation, erythrocytes transfusions, catecholamines support, renal substitution therapy, surgical interventions and artificial feeding were listed, as well as, glutamine exogenous supplementation. Regular regimens were used in enteral nutrition; glutamine (0.2-0.4 mg/kg/day) was provided intravenously in patients on parenteral nutrition.
Assessment was undertaken at the time of admittance in the ICU, at the first and the third days, with measurement of amino acid plasma levels (citrulline, ornithine, proline, arginine, glutamine, alanine, glutamic acid, leucine and isoleucine) and routine laboratory tests (including blood gases analysis and arterial lactate level).
Plasma levels of amino acids were quantified by ion exchange chromatography in a high-pressure system (Biochrom 30 analyzer). Plasma was obtained from blood drawn in ethilenediaminotetraacetic acid, by centrifugation at 4,000 g, during 10 minutes, and refrigerated at 4 °C; samples were prepared with 12% ditiotreitol, five to 10 minutes, deproteinized with sulfosalicilic acid, 60 minutes at room temperature and, after separation of the sediment by centrifugation, were filtered and stored at -20 °C for posterior processing.
Primary targets included in-hospital mortality rate and actuarial survival. Secondary goals were health care-associated infections rate 24, extent of invasive ventilation support, hospital and ICU lengths of stay and performance status at the last examination (as stated by the Karnofsky index) 25. The criteria of the health care-associated infections in the acute care setting of the National Healthcare Safety Network (NSHN), Centers for Disease Control and Prevention (CDC), Atlanta, GA, USA were considered 24.
Statistical analysis was completed with SPSS Software version 18.0 for Windows (SPSS Inc., Chicago, IL, USA) applying Qui-square, Student's t, Kaplan Meier and log rank tests, Pearson's correlations and Receiver Operating Characteristic
(ROC) curves. Significant differences were regarded for p value < 0.05. Data were expressed as n (%) or mean ± standard deviation (SD).
RESULTS
Twenty-three critical trauma patients were included, 78.3% of male gender, with a mean age of 48.8 ± 17.8 (21-82) years-old and 78.3% primarily admitted. Mean values of APACHE II, SAPS II and SOFA scores were 19.4 ± 5.5 (10-32), 41.3 ± 12.2 (20-78) and 6.9 ± 3.2 (2-10), respectively; Shock Index, Injury Severity Score and Revised Trauma Score were 0.82 ± 0.25 (0.31-1.4), 47.9 ± 18.5 (27-75) and 5.9 ± 1.3 (3.6-7.6). All the patients were submitted to invasive ventilation and enteral nutrition, 16 to cathecolamines support, 14 to erythrocytes transfusion, 14 to surgical interventions and one to parenteral nutrition. ICU, hospital and global mortality rates were 17.4%, 26.1% and 43.5%, respectively. Health care-associated infections rate was 87%. Mean duration of ventilation support was 12.7 ± 7.8 (2-27) days; ICU and hospital extent of stay were 13.9 ± 9.1 (3-52) and 29.4 ± 21.9 (5-95) days. After a mean follow-up of 7.4 ± 3.1 (2.3-12.2) months, actuarial survival was 229.2 ± 32.9 (95%CI 164.7-293.8) days. Karnofsky's index at the moment of the last examination was 69 ± 17.3 (40-90).
Analysis of plasma amino acid profile was completed in all patients at the ICU admission; in 18 both at the admission and the first day; 12 patients fulfilled the three points of assessment.
In critical trauma patients, mean value of citrullinemia at the moment of admission was low [19.5±11.1 (4-60.3) μmol/L] and increased, although not significantly, during the first three days in the ICU [20.2 ± 10.6 (5.6-49.2) μmol/L in the first day and 24.8 ± 15.2 (13.8-56.6) μmol/L in the third day] (Fig. 1). Severe hypocitrullinemia (< 20 μmol/L) prevalence was high (n = 16; 69.6%). At admittance, citrullinemia was not significantly correlated with the plasma concentrations of other amino acids, including glutamine, arginine, ornithine and proline. Baseline citrullinemia was inversely and significantly correlated with shock index [Pearson's correlation coefficient (r) = -55.1%, p = 0.008] and length of invasive ventilation support (r = -42.7%, p = 0.042) (Fig. 2). No significant connection was observed between citrullinemia and severity indexes. Citrullinemia < 13.7 μmol/L at admission, documented in 17.4% of patients, was associated with higher shock index (1.27 ± 0.10 versus 0.75 ± 0.18, p = 0.0001) and longer duration of invasive ventilation support (20.3 ± 7 versus 11.2 ± 7.1 days, p = 0.029) and of intensive care unit stay (22 ± 5.9 versus 12.2 ± 8.8 days, p = 0.048) (Table I). In univariate analysis, a citrullinemia reduction at the first day after admission (∆Citrullinemia1) superior to 12.7%, verified in 17.4% of patients, constituted a significant predictive factor of in-hospital mortality [75 versus 14.3%, p = 0.044; odds ratio = 7.8 (95%CI 1.04-58.8); accuracy = 65.2%; sensitivity = 60%; specificity = 92.3%; positive predictive value = 75%; negative predictive value = 85.7%] and lower actuarial survival (69.8 ± 41.6 versus 278.1 ± 37.4 days, p = 0.034) (Fig. 3 and Fig. 4).
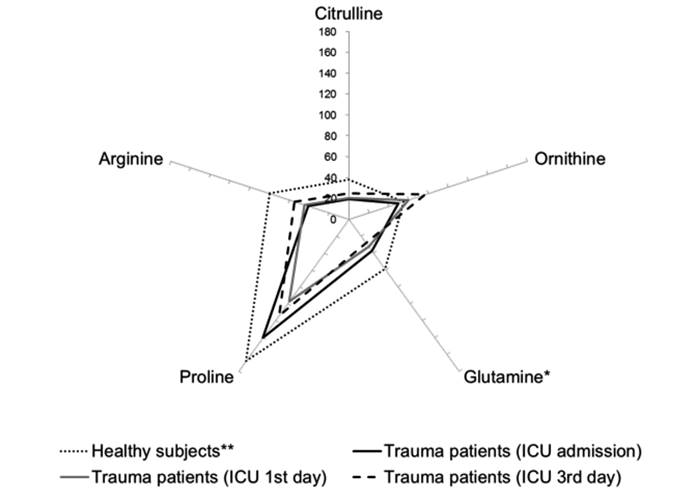
Figure 1 Mean plasma concentrations of citrulline, glutamine, ornithine, proline and arginine in critical trauma patients (n = 23) at the moment of admission in the intensive care unit (ICU), at the first and the third days. *Plasma levels × 10-1; **Mean values of a cohort of fasting healthy individuals (n = 100) were used for comparison (26).

Figure 2 Correlations between citrullinemia at the admission and Shock Index (r = -55.1%, p = 0.008) and invasive ventilation support duration (r = -42.7%, p = 0.042) in severe trauma patients (n = 23). Pearson’s correlation test and coefficient (r) were used. Shock index was calculated as the ratio between the first recorded heart rate and systolic blood pressure and its normal value is considered 0.7 or less (23). °Citrullinemia ≥ 13.7 μmol/L, • Glutaminemia < 13.7 μmol/L.
Table I Relation between citrullinemia at the admission and critical trauma patients' characteristics, severity scores and outcome parameters (n = 23)
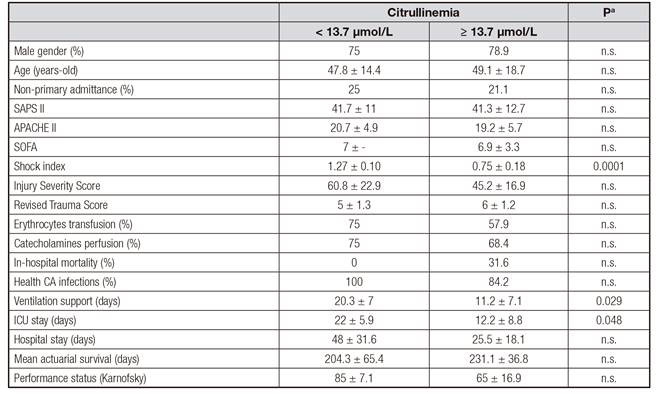
Data expressed as number (%) or mean ± standard deviation. APACHE II: Acute Physiology and Chronic Health Evaluation II; Health CA infections: health care-associated infections; SAPS II: Simplified Acute Physiology Score II; SD: standard deviation; SOFA: Sequential Organ Failure Assessment; vs.: versus; statistically n.s.: statistically not significant. at-Student and Qui-square tests.

Figure 3 Variation of citrullinemia between the moment of admission and the first day at the intensive care unit (∆Citrullinemia1) in critical trauma patients (n = 23) according in-hospital mortality. • ∆Citrullinemia1 ≥ -12.7%, • ∆Citrullinemia1 < -12.7%
DISCUSSION
In present series, acute intestinal dysfunction, defined as the reduction of enterocyte function and quantified by the citrulline plasma concentration, developed frequently and early after severe trauma. Approximately 69.6% of patients demonstrated citrullinemia levels under 20 μmol/L at the time of ICU admission, in consonance with the observed by other authors (50 to 68%) 6. Mean citrulline plasma levels of critical trauma patients at the admission on the ICU were lower than those of described in the literature for fasting healthy individuals 26.
Baseline citrullinemia demonstrated a significant inverse and moderate correlation with the shock index, in agreement with the pathophysiology of gut failure in critically ill patients; in fact, ischemia is one of the leading mechanisms of loss of enterocyte integrity in this context 6. Intestinal mucosa is extremely sensitive to ischemia-reperfusion injury with induction of epithelial apoptosis, disruption of barrier integrity and increase of permeability 27.
According present data and in agreement with other studies 6, an association between citrullinemia values and outcome parameters was demonstrated. Citrullinemia was inversely related with duration of invasive ventilation and baseline levels of citrulline below 13.7 μmol/L were significantly associated with prolonged mechanical ventilation and ICU stay. Furthermore, a reduction of citrulline levels higher than 12.7% during the first day after admission constituted a risk factor of in-hospital mortality, with high specificity and negative predictive value, and of lower actuarial survival. Citrullinemia threshold observed in present study is in consonance with those referred in the literature 6.
Intestinal mucosal barrier integrity is compromised in the critical illness, with increase of epithelial apoptosis and permeability.
Autodigestion and release of toxic intestine-derived mediators through the mesenteric lymphatics induces inflammatory, cytotoxic and proteolytic injuries in distant organs, including the lung 28 .
Citrullinemia has been related with objective intestinal dysfunction, including histological evidences of damage 29, systemic inflammation parameters 7,30-33, bacterial translocation 30,34 and clinical manifestations of intestinal dysfunction, such as ileus, diarrhea and bleeding 6,35.
Piton G et al. 31 verified that citrullinemia plasma concentrations ≤ 10 μmol/L at the first 24 hours, present in 44% of critically ill patients, were associated with higher nosocomial infection rates and constituted independent risk factors of 28 days-mortality. In another study, citrullinemia levels ≤ 12.2 μmol/L and plasma concentrations of intestinal-fatty acid binding protein (an enterocyte damage marker) ≥ 355 pg/mL at the moment of ICU admission were independently related with higher 28 days-mortality in multivariate analysis 7. Plasma citrulline concentration less than or equal to 10 µmol/L at admission to the ICU was associated with higher intra-abdominal pressure, higher plasma C-reactive protein concentration, and more frequent antibiotic use 7.
Hypocitrullinemia < 15 μmol/L was connected with the development of clinical manifestations of intestinal dysfunction, including higher residual gastric volume, ileus, among others 35.
Although citrullinemia has been proposed for the evaluation of the intestinal function in the critically illness, its prognostic value requires further validation. In fact, in this context, limitations of citrullinemia include the susceptibility to the interferences of renal insufficiency, the reduced glutamine bioavailability and the increase of extra-intestinal synthesis of citrulline from arginine in the systemic inflammatory syndrome 6,12,13.
Limitations of present series included the single-center character, small number of studied patients and high severity scores.
Present findings confirm the precocious development, high prevalence and prognostic relevance of hypocitrullinemia, considered a biomarker of intestinal dysfunction, in severe trauma patients. Evaluation of intestinal function may allow the implementation of prophylactic and therapeutic strategies of intestinal integrity preservation with potential impact on prognosis. Additional studies are necessary to determine the citrullinemia value in this context.















