Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.34 no.4 Madrid jul./ago. 2017
https://dx.doi.org/10.20960/nh.911
Organization and management of clinical nutrition in Spain. How do we assess the quality of our activities?
Organización y gestión de la nutrición clínica en España. ¿Cuánto evaluamos la calidad de nuestra actividad?
Tomás Martín Folgueras, María Dolores Ballesteros Pomar, Rosa Burgos Peláez, María Victoria Calvo Hernández, Luis Miguel Luengo Pérez, José Antonio Irles Rocamora, Gabriel Olveira, Alfonso Vidal Casariego and Julia Álvarez Hernández; on behalf of the Management Working Group of SENPE
ABSTRACT
Introduction: Among the objectives of the SENPE Management Working Group is the development of knowledge and tools related to the evaluation of health outcomes.
Objectives: To obtain an approximate profile of clinical nutrition in hospitals in Spain, specifically concerning its organization, endowment, activities and quality indicators.
Methods: A cross-sectional study conducted in 2013 through a structured survey sent to a random sample of 20% of hospitals from the network of the National Health System of Spain, stratified by the number of hospital beds.
Results: The overall response rate was 67% (83% in hospitals with over 200 beds). In 65% of hospitals, clinical nutrition is run by a coordinated team or unit, with a doctor working full time in only 50% of centers. Other professionals are often not recognized as part of the team or unit. There is a specialized monographic nutrition clinic in 62% of centers and 72% have more than 40 new inpatient consultations per month (27% with more than 80 per month). Among the centers with a clinical nutrition team or unit, there is a greater tendency to monitor quality indicators related to clinical practice.
Conclusions: There is widespread addition of clinical nutrition teams and units in hospitals in Spain. However, truly multidisciplinary organization is not often found. High workloads are assumed in relation to staffing levels. The existence of well-organized structures may be associated with benefits that directly affect attendance.
Key words: Quality of health care. Quality indicators of health care. Malnutrition. Organization and administration.
RESUMEN
Introducción: el Grupo de Trabajo de Gestión de SENPE tiene entre sus objetivos el conocimiento y desarrollo de herramientas para la evaluación de resultados en salud.
Objetivos: obtener un perfil aproximado de los equipos de Nutrición Clínica en los hospitales de España, específicamente sobre su organización, dotación, actividad e indicadores de calidad.
Métodos: estudio transversal realizado en 2013 mediante una encuesta estructurada remitida a una muestra aleatoria del 20% de hospitales de la red del Sistema Nacional de Salud, estratificada por número de camas de hospitalización.
Resultados: la tasa de respuesta global fue del 67% (83% en centros con más de doscientas camas). En el 65% de los centros, la Nutrición Clínica está a cargo de un equipo coordinado o una unidad, con médico a tiempo completo en solo un 50% de centros. Con frecuencia no se reconocen otros profesionales como parte del equipo o unidad. Existen consultas monográficas especializadas en nutrición clínica en un 62% y se atienden más de 40 nuevas consultas mensuales de hospitalización en el 72% de los centros (más de 80 en el 27%). Entre los centros con equipo de Nutrición se observa una mayor tendencia al seguimiento de indicadores de calidad relacionados con la práctica clínica.
Conclusiones: la incorporación de equipos y unidades de Nutrición Clínica es amplia en los hospitales de España. No es frecuente una verdadera organización multidisciplinar y se asumen cargas de trabajo elevadas en relación a las dotaciones de personal. La existencia de estructuras bien organizadas puede acompañarse de beneficios que repercuten directamente en la calidad de la asistencia.
Palabras clave: Calidad asistencial. Indicadores de calidad sanitaria. Malnutrición. Organización y administración.
Introduction
Management can be defined as taking on activities to achieve a concrete goal. One of the activities included in this definition is being held accountable for achieving appropriate results in order to evaluate situations and take any corrective measures that may be necessary. Quality indicators are tools that allow managers to evaluate these situations. There are quantitative and qualitative instruments that measure the degree of adherence to the specifications established for the key components of a given activity.
The Management Working Group (Grupo de Trabajo de Gestión or GTG), which is part of the Spanish Society of Parenteral and Enteral Nutrition (SENPE), was created in 2009 and its main objectives were established in the 6th Debate Forum of SENPE:
- To develop a model for a Clinical Nutrition and Dietetics Unit to serve as a complete model of management that can be reproduced throughout Spain.
- To establish standards and select minimum quality indicators.
- To develop an evaluation process.
- To facilitate the accreditation process.
- To create a dialogue with health administrations in order to carry out a strategic plan against malnutrition.
- To establish flow dependence and a range of actions, i.e., through an integrated dashboard.
Due to its natural interest in the evaluation of results, the GTG decided in its early stages to carry out a survey in which it asked about a number of indicators to determine opinions concerning the relevance and viability of applying these indicators in the workplace (1). This study allowed us to make a selection of the most important quality indicators in clinical nutrition.
Next, with the collaboration of the Spanish Society of Hospital Pharmacy, we developed a Guideline for the Evaluation of the Clinical Nutrition Process to facilitate the work of clinical nutrition and dietetics micromanagers in hospitals. In these guidelines the process of nutritional support is divided into several subprocesses, starting with nutritional screening. For every subprocess, several aspects are detailed, including key objectives and quality indicators, together with the methods for their measurement (2).
In parallel with the aforementioned project, the GTG established the need for another survey to study the status of clinical nutrition in Spain with regard to measuring quality indicators. We were not as much interested in the results themselves as in the measurement of these indicators. Also, we wanted to seize the opportunity to bring knowledge concerning the current state of nutrition teams up to date as many years had gone by since the last study on the subject (3). Through this study, it was possible to obtain a general view of clinical nutrition management in Spain.
The general objective of this study was to obtain an approximate profile of clinical nutrition in Spain. The specific objectives were to determine the types of organization available to clinical nutrition resources, the human resource endowment, and the activities that the teams carry out within their field and the quality indicators that they use to control and improve their activities.
Materials and methods
This was a cross-sectional study undertaken throughout Spain in 2013. Using the National Catalogue of Hospitals within the National Health System (available at https://www.msssi.gob.es) as a reference, centers were selected according to the following criteria:
- General care, surgical or medical-surgical centers. We excluded geriatric, psychiatric, maternal, pediatric, orthopedic and/or rehabilitation centers, as well as some monographic, high resolution and penitentiary centers.
- Functional dependence on a public entity (regardless of the number of hospital beds) or private hospitals in association with the National Health System (charitable hospitals, hospitals belonging to insurance companies or associated with the Ministry of Defense) with 150 hospital beds or more. Two private centers not associated with the National Health System but with teaching accreditation were also included.
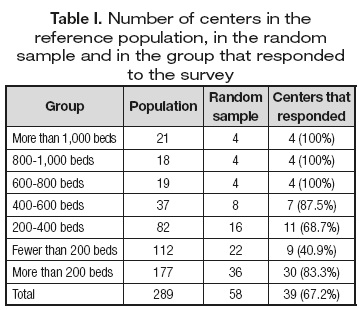
The final population for this study included 289 centers with 110,314 hospital beds. To avoid bias due to the tendency of centers with better results to respond, a random sample of 20% of these centers was taken and the sample was stratified according to the number of beds (Table I).
The GTG members reached a consensus and decided on a model for the survey to be sent out that included three different sections. The first section focused on general aspects: contact data, number of beds, population covered by the hospital and teaching hospital accreditation.
The second section aimed to gather information concerning the organization and patient care activities with regard to clinical nutrition. To study the organizational model of the center, we asked participants to place their center in one of the models proposed in a list (Table II). We asked about staff endowment, focusing on the number of people assigned to clinical nutrition in each center and specifying if the assignment was full time or part time (more or less than 50% of time). To study inpatient consultation activities, we asked about the number of new patients seen in one week and the time it took to respond to these consultations. We also wanted to know if hospital food was prepared on the premises of the hospital or in another center, and if parenteral nutrition formulas were prepared in the hospital pharmacy or if alternative presentations were used (ready-to-use formulas or those prepared by a catering service). With regard to outpatient activities, we asked about the existence of a nutrition outpatient clinic, the mean number of outpatients seen in such clinics and the percentage of patients who were malnourished or obese (with or without fulfilling criteria for bariatric surgery) and had eating disorders or dyslipidemia. Finally, we wanted to know where the formulas and consumables used in the administration of home enteral nutrition were obtained.
The third section was devoted to gathering information concerning activities aimed at improving the quality of healthcare. In this section, we asked about their level of conformity with a list of statements (Tables IV-X) using a 5-point Likert scale: 1 = strongly disagree, 2 = slightly disagree, 3 = somewhat agree, 4 = agree, 5 = strongly agree. To rule out a lack of improvement initiatives due to them not being considered as a priority, for every statement the subject was asked to respond twice: in part A with regard to the reality of their center and in part B according to the possibility of carrying out these activities.
STATISTICAL ANALYSIS
For the statistical analysis, hospitals were grouped according to the number of beds: more or fewer than 600. According to the organizational structure, the hospitals were subdivided into those with a nutrition unit or a nutrition team (as described in table II) to compare them with those in which the center's nutritional support depended on certain people without the support of an organized group or in which each doctor was responsible for their patients' nutritional support (rest of the options in table II).
To analyze each statement in the third section, we only included those hospitals that were confirmed as carrying out initiatives to improve the quality of healthcare (grades 4 or 5 in part B). These hospitals were grouped according to their responses regarding their own reality into "adherers" (grades 3 to 5 in part A) and "non-adherers" (grades 1 or 2 in part A). In this part of the study, we only considered the hospitals with more than 200 beds, with a higher potential to serve patients with nutritional disorders and to activate measures to improve quality.
The results were compared using the Chi2 test (considering p < 0.05 as significant) with regard to the number of beds (hospitals with 200-600 beds vs those with more than 600 beds) and the existence or not of a nutrition unit or team.
Results
GENERAL DATA
Surveys were sent out to 58 hospitals and responses were received from 39 (67%). Of these hospitals, 40% were county hospitals, 51% were reference hospitals and 9% were private hospitals associated with the National Health System. The median number of hospital beds was 442 (interquartile range 349.5) and the median population covered by these hospitals was
270,287 (interquartile range 212,500). In all, 70.6% of the hospitals were associated with undergraduate education and 85.3%, with graduate education. Of the hospitals with more than 200 beds, 30 out of 36 centers responded (83%), while of those with fewer than 200 beds, nine out of 22 centers responded (40%).
ORGANIZATIONAL STRUCTURE AND PERFORMANCE
The organizational structure of clinical nutrition in each center is described in table II. Clinical nutrition units are more common in hospitals with more than 400 beds (83.3% vs 14.3%, p < 0.001) and in reference hospitals (75% of reference hospitals, compared with 36% of county hospitals and 33% of private hospitals, p = 0.175). The endowment of staff devoted to clinical nutrition is shown in table III.
Inpatient assistance constituted between 40 and 80 new consultations monthly in 45% of centers and more than 80 monthly consultations in 27.5% of centers; 27.5% of centers had fewer than 40 monthly consultations. Hospitals without a nutrition team or unit had a significantly lower (p = 0.024) number of new consultations (fewer than 40 per month in all cases) compared to centers with a nutrition team or unit (between 40 and 60 consultations in 35% of cases, between 60 and 80 in 22%, and more than 80 in 30%). The delay in tending to these consultations was less than 24 hours in 97% of cases.
Hospital food was prepared in the hospital kitchen in 86% of centers and we found no differences with regard to the existence or not of a nutrition unit or team. Parenteral nutrition was usually prepared in the hospital pharmacy; ready-to-use formulas were sometimes used in 74% of hospitals and solely used in 20% of centers.
In outpatient care, there was a specialized monographic nutrition clinic in 62% of cases, while in 35% of cases nutritional disorders were addressed with no monographic clinic devoted to nutrition. Of those centers with a nutrition unit or team, 83% have a monographic nutrition clinic as opposed to 11% in hospitals without a nutrition unit or team (p = 0.005). The mean number of outpatients seen per week in specialized clinics was 57.5 (standard deviation [SD] 44.0). Of the outpatients seen in these clinics, 47% were malnourished and received nutritional assessment and support (SD 21.0), 23% were obese and had indications for bariatric surgery (SD 18.5), 20% were obese without indications for bariatric surgery (SD 11.8), 4% had dyslipidemia (SD 6.3) and 4% (SD 5.5) had eating disorders.
Patients with home enteral nutrition obtain oral supplements and formulas to be administered by feeding tubes, mainly from pharmacies outside the hospital (73%). Fungible goods (syringes, feeding tubes, etc.) are obtained in 50% of cases from centers that depend on hospitals (25% of cases obtain them from nutrition outpatient clinics) and in 46% of cases they are obtained from Primary Care centers.
INITIATIVES THAT AIM TO IMPROVE QUALITY
In tables IV to X, we show the results obtained with regard to each of the initiatives proposed to improve quality. For each statement, the percentage of centers that conformed and the percentage of "adherers" and "non-adherers" are shown.
We differentiate between centers with more or fewer than 600 beds and between those with and without a nutrition team or unit. The statistically significant differences mentioned above are shown.
Discussion
In this study information concerning the organization and structure of clinical nutrition in a variety of hospitals in Spain is presented. As the study was performed using a randomly selected sample, we have avoided obtaining results only from hospitals with a greater degree of awareness in the field of clinical nutrition, thus enhancing the reliability of our data.
On the other hand, the global response rate to the survey (67%) could be considered as a limitation. Nevertheless, among the hospitals with more than 200 beds, comprising the majority (86%) of the sites in the country, the response was higher (83%). These are more complex centers which are more likely to have patients with malnutrition. Thus, we believe that the data presented here approximately describe the reality of clinical nutrition in Spain. Difficulty in finding contacts was the main obstacle in the group of centers with fewer than 200 beds, in which we presume that activity related to clinical nutrition is considerably lower.
Similar initiatives were carried out in Germany (4), Portugal (5), Austria and Switzerland (6) in the early 2000s. However, the methodology varied and the results were very diverse, especially regarding the structure of the units. Moreover, they did not employ quality measures, as we did. For example, a study carried out in twelve European countries with the support of ESPEN (7) considered only university hospitals and obtained 199 responses to the survey (36% of potential responses). In the Portuguese survey, the participation rate was 44%.
At the time of our survey, clinical nutrition assistance was organized through a nutrition unit or team that was adequately structured in more than half of hospitals. As was to be expected, this was more common in larger centers. In the aforementioned European survey, 86% of the 21 Spanish hospitals asked had nutrition units. Although this value is higher than ours, we believe that the results are not comparable. First, the sample was not randomly obtained and was limited only to university centers. Second, in the European survey, what constituted a nutrition unit was not defined.
With regard to the endowment of staff devoted to clinical nutrition, there was considerable heterogeneity between hospitals both in terms of the number and types of degrees held by the staff. It is remarkable that only 50% of centers with a nutrition unit or team had a doctor working with them full time and the percentage decreased to 40% when we considered the presence of a pharmacist in the team or unit. The results were even worse for the rest of the professional categories, with the exception of nurses.
The activities performed were very variable in quantitative and organizational terms. In centers with a nutrition unit or team, hospital activity was significantly greater and the presence of a specialized outpatient clinic was higher.
Regarding the section of the study measuring the quality of nutritional assistance, we believe that this is the first initiative related to these characteristics and no such work has previously been published in any country. In this study, the degree of conformity with the indicators proposed was very high (more than 85%). The indicators with lower levels of agreement shared the common feature that they were not related to healthcare (existence of a welcome plan for staff, carrying out satisfaction surveys among patients who were discharged, and control of outpatient clinics in a single sphere).
Among the indicators with higher levels of agreement, there were some with a high degree of adherence. These were indicators related to the preparation, dispensation and administration of artificial nutrition (except the labelling of enteral nutrition packages). This result is probably related to the systematic nature of this activity.
The indicators with high agreement rates but mid or low levels of adherence comprise areas in which improvements could be made. Within this group, it is worth noting the low adherence for activities related to nutritional screening, which in our previous study (1) were shown to be considered as the most relevant but least feasible. The result obtained for the indicator of nutritional assessment among patients with pressure ulcers was also low. The existence of a nutrition team or unit may possibly help overcome obstacles in this regard as the centers that had these units or teams had significantly better results. However, although the five hospitals that performed nutritional screening had a nutrition unit or team, the result of the comparison was not significant.
Hospitals with a nutrition unit or team more frequently reported having basic clinical protocols compared to the rest of the centers. However, the degree of adherence to these protocols can still be improved. Although it did not reach statistical significance, the result tended to be better in centers with a nutrition unit or team with reference to the follow-up of nutritional requirements, use of feeding ostomies in patients with prolonged enteral nutrition, and short-term parenteral nutrition.
Although again not reaching statistical significance, we believe that it is important to point out that the results are consistently better in centers with a nutrition unit or team for the majority of indicators directly related to clinical practice and improvements in efficiency, supporting their potential to be valuable in clinical nutrition assistance.
Finally, we found a low frequency for the proportion of critically ill patients among whom enteral nutrition was initiated early and follow-up of the percentage of patients who received artificial nutrition among whom nutritional requirements were met. This could be due to the difficulty perceived in measuring these indicators, but such assessment requires greater attention due to the relevance of the aspects pointed out.
In conclusion, we can state that, although the establishment of clinical nutrition units and teams is widespread, especially in hospitals with a greater number of beds, their characteristics with regard to organization and performance are highly variable. Clinical nutrition teams and units frequently do not have a multidisciplinary endowment of staff and in many instances there are insufficient numbers of staff devoted solely to clinical nutrition. The existence of nutrition units or teams in hospitals is associated with improved performance and an increase in the existence of specialized outpatient nutrition clinics, as well as a greater tendency to carry out improvement measures that directly affect assistance.
Members of the management working group of SENPE
Julia Álvarez Hernández, Maria Dolores Ballesteros Pomar, Néstor Benítez Brito, Rosa Burgos Peláez, Maria Victoria Calvo Hernández, Verónica Chazín, Abelardo García de Lorenzo y Mateos, Pedro Pablo García Luna, José Antonio Irles Rocamora, Teresa Lajo Morales, Luis Miguel Luengo Pérez, Tomás Martín Folgueras (coordinator), Gabriel Olveira Fuster, Cleofé Pérez Portabella, Hegoi Segurola Gurrutxaga, Alfonso Vidal Casariego and Cristina Velasco.
References
1. Martín Folgueras T, Álvarez Hernández J, Burgos Peláez R, Celaya Pérez S, Calvo Hernández MV, García de Lorenzo A, et al.; Grupo de Trabajo de Gestión de SENPE. Análisis de la relevancia y factibilidad de indicadores de calidad en las unidades de nutrición. Nutr Hosp 2012;27(1):198-204. DOI: 10.1590/S0212-16112012000100024. [ Links ]
2. SENPE. Proceso de nutrición clínica. Guía de evaluación. Disponible en: http://www.senpe.com. Consultado 21/07/2017. [ Links ]
3. Soto A, Tofé S, León M, García-Luna PP. Estudio sobre la situación organizativa y asistencial de la nutrición clínica hospitalaria en España: de 1995 a 2001. Endocrinol Nutr 2003;50(1):8-13. [ Links ]
4. Senkal M, Dormann A, Stehle P, Shang E, Suchner U. Survey on structure and performance of nutrition-support teams in Germany. Clin Nutr 2002;21(4):329-35. [ Links ]
5. Ravasco P, Martins P, Ruivo A, Camilo ME. Survey on the current practice of nutritional therapy in Portugal. Clin Nutr 2004;23(1):113-9. [ Links ]
6. Shang E, Hasenberg T, Schlegel B, Sterchi AB, Schindler K, Druml W, et al. An European survey of structure and organisation of nutrition support teams in Germany, Austria and Switzerland. Clin Nutr 2005;24(6):1005-13. E-pub Sep 6 2005. [ Links ]
7. Jonkers C, Lochs H, Lerebours E, Meier R, Messing B, Soeters PB. Survey to establish the current status of artificial nutritional support in Europe. Clin Nutr 1999;18(3):179-88. [ Links ]
![]() Correspondence:
Correspondence:
Tomás Martín Folgueras.
e-mail: Tmf7312@hotmail.com
Received: 12/01/2017
Accepted: 02/05/2017