Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.34 no.6 Madrid nov./dic. 2017
https://dx.doi.org/10.20960/nh.1065
Does the presence of pressure ulcers entail "high risk of negative outcomes" in geriatric rehabilitation? Results from a retrospective cohort study
¿Son las úlceras por presión al ingreso, un factor predictor negativo de los resultados en unidades de rehabilitación geriátrica? Resultados de un estudio de cohortes retrospectivo
Sebastià J. Santaeugènia1, Miquel Àngel Mas1, Francisco J. Tarazona-Santabalbina2, Ana María Alventosa1, Manoli García1, Albert Monterde1, Alicia Gutiérrez1 and Joan Cunill1
1Department of Geriatric Medicine and Palliative Care. Badalona Serveis Assistencials. Badalona, Barcelona. Spain.
2Department of Geriatric Medicine. Hospital Universitario de la Ribera. Alzira, Valencia. Spain. Faculty of Medicine. Universidad Católica de Valencia San Vicente Mártir. Valencia
ABSTRACT
Aim: A retrospective cohort study was performed in order to evaluate the prevalence of pressure ulcers (PrUs) in older patients admitted to a geriatric rehabilitation unit of a postacute care hospital and to investigate the impact of the presence of PrUs on clinical outcomes of the rehabilitation process.
Methods: We studied 668 post-acute patients consecutively attended, from January 2010 to December 2011. The effect of having PrUs at admission was evaluated based on its impact on outcomes: final destination, functional status, mortality and length of stay in the rehabilitation unit.
Results: PrUs prevalence at admission was 16%. Patients with PrUs were older, more disabled and had more complex conditions, including malnutrition and cognitive impairment. In the bivariate analysis, we found patients with PrUs at admission had worst final outcome (%): discharge home (69.2 vs. 82.5), discharge long term care setting (14 vs. 6.4), discharge acute care (8.4 vs. 6.2) and death (8.4 vs. 4.8); p < 0.001, and worst Barthel Index score at discharge 57 (SD 34.1) vs. 83 (SD 33.6); p < 0.001, with longer length of stay in the unit 61 (SD 42.3) vs. 53 (SD 37.1); p 0.004. In the multivariate analysis, PrUs presence was found as one of the variables with significant association to no return to home. Finally, a negative association between PrUs at admission and functional gain at discharge of the postacute unit was identified.
Conclusions: PrUs were prevalent and had negative impact on clinical outcomes of our geriatric unit, as discharge destination, functional gain and Length of Stay, in vulnerable patients.
Key words: Rehabilitation. Intermediate care. Subacute care. Malnutrition. Pressure ulcer.
RESUMEN
Objetivo: se realizó un estudio de cohorte retrospectivo para evaluar la prevalencia de úlceras por presión (PRU) en pacientes mayores ingresados en una unidad de rehabilitación geriátrica de postagudos (atención intermedia) e investigar el impacto de la presencia de PrU en los resultados clínicos del proceso de rehabilitación.
Métodos: se estudiaron 668 pacientes ingresados de forma consecutiva, de enero de 2010 a diciembre de 2011. Se evaluó el impacto de la presencia de PrU en el momento del ingreso en relación a los siguientes resultados de salud: destino final, estado funcional, mortalidad y duración de la estancia en la unidad de rehabilitación.
Resultados: la prevalencia de PrU en el momento del ingreso fue del 16%. Los pacientes con PrU tenían mayor edad, más presencia de discapacidad y tenían una mayor prevalencia de condiciones complejas, incluyendo desnutrición y deterioro cognitivo. En el análisis bivariado se encontró que los pacientes con PrU al ingreso presentaron un peor resultado final (%): alta a domicilio (69,2 vs. 82,5), ingreso en unidades de larga estancia (14 vs. 6,4), reingreso hospitalario (8,4 vs. 6,2) y fallecimiento (8,4 vs. 4,8); p < 0,001, y un peor índice de Barthel al momento del alta (57 frente a 83); p < 0,001, con mayor duración de la estancia en la unidad (61 frente a 53 días); p 0,004. En el análisis multivariante, la presencia de PrU en el momento del ingreso, se asoció como variable predictora negativa de retorno a domicilio, así como predictora negativa respecto a la ganancia funcional al alta de la unidad postagudos.
Conclusiones: las PrUs fueron prevalentes y tuvieron un impacto negativo en los resultados clínicos de nuestra unidad geriátrica, como destino de alta, ganancia funcional y duración de la estancia, en pacientes vulnerables.
Palabras clave: Rehabilitación. Atención intermedia. Subagudos. Malnutrición. Úlceras por presión.
INTRODUCTION
Pressure ulcers (PrUs) remain a major health problem that especially older patients from various health and social settings and from all around the world, including the US and European countries, are confronted with (1-3). Multimorbidity, a phenomenon associated with higher life expectancy, could lead to mobility problems and disabilities for elderly people, which is involving a high risk of incidence of PrUs (4-6). A relationship has been found between the presence of PrUs and negative consequences for patients in acute hospitals, especially in geriatric units, in long term care settings and in the community (7-10). In particular, a relationship between PrUs and mortality, costs, length of stay and readmission rates has been identified (11-13). Old age, functional and cognitive impairment, faecal and urinary incontinence, malnutrition, being bedridden and being institutionalized are considered as main risk factors associated with pressure sores (14,15). Meanwhile, preventive and comprehensive care strategies have been associated positive impacts on health outcomes and cost savings (16-18) especially in acute care units. However, more research is needed in sub-acute and post-acute care settings due to high prevalence of main pressure sores risk factors in patients admitted to these units (19,20). In this context, the aim of this study was to evaluate the prevalence and the clinical impact of pressure ulcers in older patients admitted to a geriatric rehabilitation unit of an Intermediate Care hospital, in order to develop individualized care strategies for future research.
METHODS
Study population, setting and data collection
Data collection was conducted by a specialized research staff (geriatricians and expert nurses) from a Comprehensive Geriatric Assessment database used in the post-acute care setting of the Department of Geriatric Medicine and Palliative Care of Badalona Serveis Assistencials, at El Carme Intermediate Care Hospital in Badalona, located north of Barcelona's urban area. Patients consecutively admitted from 1st January 2010 to 31th December 2011 for treatment of post-acute conditions and rehabilitation after acute illness were considered to be included. The suffering from a terminal illness or a medical/cognitive status not considered adequate for tolerate rehabilitation therapies were exclusion criteria. An individualized rehabilitation plan was provided by a multidisciplinary care team (medical, nursing, physiotherapy, occupational therapy and social work staff) and was based on Comprehensive Geriatric Assessment, which refers to a multidimensional assessment followed by an individualized care plan (21). Assessment included the following dimensions: functional -measured by therapists using the Barthel Index Granger version (22); co-morbidity - measured by the Charlson Comorbidity Index (23); social situation (clinical evaluation by social worker); and geriatric syndromes (24)- based on an structured clinical evaluation done by nurse staff, using North American Nursing Diagnosis Association (NANDA, 2012) (25). The main geriatric syndromes evaluated comprised: polipharmacy (5 o more drugs prescribed on admission), incontinence, falls, constipation, immobility, cognitive impairment/dementia, mood disorder and malnutrition. Health staff evaluated the skin status in the first 24 hours of admission, who also registered if the patient had a prevalent pressure ulcer as a condition to be included in the multidisciplinary care plan.
As main outcomes at discharge of the unit were considered: positive functional gain (measured by Barthel Index at discharge - Barthel Index at admission > 0), length of stay in the unit (days), acute hospitalization, death and home destination at discharge. These outcomes were analysed based on the presence or absence of pressure ulcers at admission.
Data analysis
A descriptive analysis was conducted to examine the data distribution and to describe the study sample, including mean, median, standard deviation and interquartile range for continuous data and percentage for categorical data.
A bivariate analysis was used to explore unadjusted associations between pressure ulcer status and clinical outcomes. Comparison of baseline and end point data between study groups involved chi-square tests for categorical variables and Mann-Whitney tests for non-normally distributed continuous variables.
A multiple logistic regression analysis was performed using discharge home as dependent variable. Finally, we developed two separated multiple linear regression models using the Barthel index at discharge and functional gain as dependent variables, and baseline characteristics considered as independent variable. For the construction of these models, we first considered the full model with all variable identified as significantly associated with dependent variables in the bivariate analysis. In a second step, any variable not causing an important change (defined as the absence of and adjusted effect of more than 10%) or not improving the standard error of the estimation upon adjusting the model without this variable was removed from the model. Agreement between the investigators was reached in cases where two or more subsets of variables were obtained with a similar degree of adjustment. Results were expressed as odds ratio and confidence interval.
All data were analysed with SPSS software (version 21;SPSS, Chicago, IL). A two-sided p value < 0.05 was considered statistically significant for all analysis.
RESULTS
A total of 668 patients were included in the analysis. Main characteristics of the sample were a mean age of 82 years (SD 9.9); 68% of female patients; Charlson Comorbidity Index 2 (SD 2); mean number of geriatric syndromes at admission 4.4 (SD 1.8). Main geriatric syndromes at admission comprised polipharmacy (64%), incontinence (49%), falls (39%), constipation (36%), immobility (32%), cognitive impairment/dementia (24%), mood disorder (22%) and malnutrition (17%). Patients were referred from acute care units in 87% of cases. Main diagnostic groups included: Orthopaedic 46%, Medical 30%, Stroke 18% and Surgical 6%.
Sixteen per cent of patients (n = 107) had PrUs at admission to the rehabilitation unit. PrUs prevalence exhibited variations between diagnostic groups: Surgical 37%, Medical 16%, Orthopaedic 15%, Stroke 11% (p < 0.01).
Table I shows the main clinical characteristics at admission related to PrUs presence. Patients with PrUs at admission had higher ages, were more disabled and suffered from more complex conditions, including malnutrition and cognitive impairment.
Table II shows the negative impact of PrUs presence on functional outcomes, mortality and discharge destination. In the bivariate analysis, patients with PrUs at admission were found to suffer at discharge from worst final outcome destination home and worst functional status (with longer length of stay in the unit). In this sense, a negative correlation was found between the variable pressure ulcers at admission and low functional gain of activities of daily living during the stay in the post-acute care unit. The PrUs presence was associated with a probability of not having a positive functional gain at discharge OR 1.637 (95% IC 1.032-2.597).
A multiple logistic regression analysis found PrUs at admission OR 0.466 (95% IC 0.263-0.824; p 0.009) and Charlson Comorbidity Index OR 0.865 (95% IC 0.758-0.988; p 0.032) as independent negative predictive variables to return home. In the same analysis change in score of Barthel Index between discharge and hospital admission OR 1.060 (95% IC 1.048-1.072; p < 0.001) was identified as independent positive predictive variable of home destination.
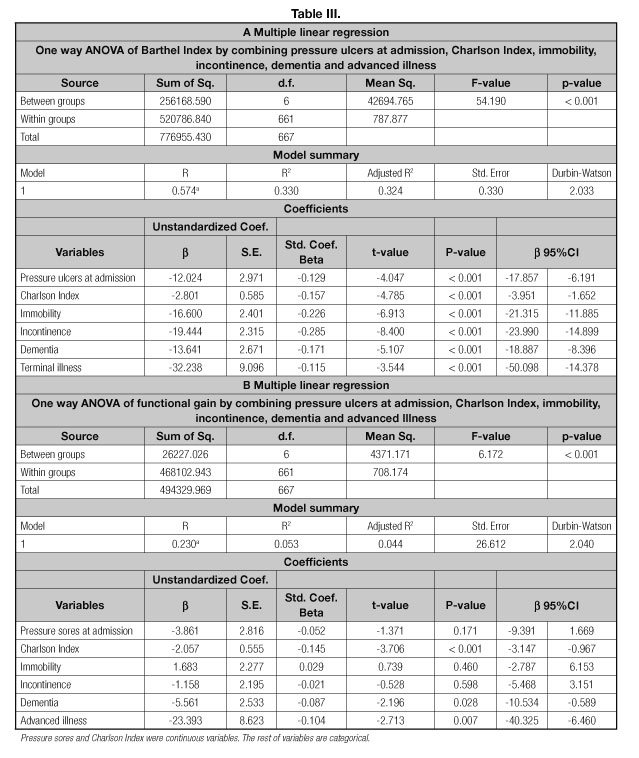
Table IIIA shows the results of an initial multiple linear regression model conducted to evaluate how well the variable pressure ulcers at admission and the other baseline characteristics predicted the Barthel Index at discharge. PrUs at admission, Charlson Comorbidity Index, immobility, incontinence, dementia and advanced illness were introduced in a model that can explain around one third of the variability (adjusted R2 = 0.324; p < 0.000).
Finally, table IIIB shows a multiple linear regression model using functional gain at discharge as a dependent variable. A negative but not significant association was found for PrUs at admission and functional gain as an indicator of clinical outcome. Nevertheless, Charlson Comorbidity Index, dementia and advanced illness were found significantly associated (adjusted R2 = 0.044; p 0.000).
DISCUSSION
In our sample, pressure ulcers were prevalent at admission to our rehabilitation hospital and had a negative impact on outcomes of post-acute patients. In the PrUs group, a significant lower percentage of destination home, worst functional outcome at discharge and longer length of stay in the rehabilitation unit was found.
These findings are in line with the outcomes of a similar study (20) conducted in an inpatient rehabilitation facility in the US, where the presence of a pressure ulcer was found to be associated with a minor lower motor gain, a longer length of stay in the facility and lower odds of being discharged to the community. Focussing on another aspect of the process of rehabilitation, a study conducted in other geriatric rehabilitation unit in Catalonia (26) found that patients with incontinence or pressure sores on admission were found to be at greater risk of interruption of the rehabilitation therapy and of carrying a poor prognosis, with less than one in four patients able to be discharged home from the unit. Hence, it was concluded that these patients might benefit from extra monitoring in order to improve the efficiency of rehabilitation programmes and discharge planning.
Nevertheless, we suggest the findings from the present study to be considered with sufficient care, as similar negative consequences of the hospitalization process could be evidenced in older patients, which are not directly related to the presence of PrUs, but rather to their "high risk of negative outcomes" profile, clinical complexity and low functional reserve. A previous study (9) found that, after adjusting for nutritional and functional status, global measures of disease severity and co-morbidity, and non-infectious hospital complications, pressure ulcers developed during acute hospitalization were not associated with reduced 1-year survival among high-risk older persons.
Furthermore, pressure ulcers were found frequent at admission in rehabilitation units, especially for surgical patients. Several papers found evidence on incidence and risk of PrUs in the continuum of care of older vulnerable patients. As an example, in a prospective cohort of hip fracture patients (27), specific relative risks in rehabilitation settings were identified. Based on our own experience, we deem it necessary to improve the prevention of pressure ulcers in older vulnerable patients at acute units, especially in surgical departments.
Finally, we identified several factors at admission that are related with the presence of PrUs, such as age, functional status or number of geriatric syndromes. Recent research (15,28) has come to similar conclusions. It could support the fact that, in geriatric hospital care, presence of PrUs can be regarded as "the tip of the iceberg" of vulnerable older patients due to their advanced age, disability and an accumulation of high-risk geriatric conditions.
More research is needed to find strategies both in acute care wards and in post-acute care settings in order to individualize management of patients with high risk of negative outcomes. Research efforts should not only focus on the prevention and management of pressure ulcers, but also on the care of other high risk geriatric conditions, such as immobility, malnutrition or cognitive impairment. In these cases, as mentioned before, the presence of a pressure ulcer could be considered as a signal of high risk profile of worse final result of the rehabilitation process.
Study limitations
The main limitation of the study is the design using a retrospective approach. It seems adequate to confirm these results with new prospective studies. A second limitation is the pragmatic approach of the PrUs group as a homogeneous category, without a sub-analysis of PrUs risk or PrUs grades. A differentiated approach may prove relevant for future analyses.
Pressure ulcers are a geriatric condition of major interest not only for the comorbidity related to acute hospitalization, but also for the consequences on health outcomes and resource consume of the post-acute phase.
It is necessary to develop preventive strategies for older vulnerable patients at acute units, especially in high-risk processes with functional acute impairment such as surgery.
Once PrUs are detected, it is therefore essential to integrate specific individualized intervention in order to minimize negative risks in health outcomes and resources use.
ACKNOWLEDGEMENTS
We would like to thank Mrs. Sonia García for the support in data revision and to Dr. Javier Soldevilla, director of GNEAUPP (Grupo Nacional para el Estudio de Úlceras por Presión) Spain, for his revision of the manuscript.
REFERENCES
1. Yarkony GM. Pressure ulcers: a review. Arch Phys Med Rehabil 1994; 75(8):908-17.
2. Garcia AD, Thomas DR. Assessment and management of chronic pressure ulcers in the elderly. Med Clin N Am 2006;90:925-44.
3. Soldevilla Agreda JJ, Torra I, et al. The Burden of Pressure Ulcers in Spain. Wounds 2007;19(7):201-6.
4. Smits J, Monden C. Length of life inequality around the globe. Soc Sci Med 2009;68:1114-23.
5. Stineman MG, Xie D, Pan Q, Kurichi JE, Saliba D, Streim J. Activity of daily living staging, chronic health conditions, and perceived lack of home accessibility features for elderly people living in the community. J Am Geriatr Soc 2011;59(3):454-62.
6. Lyder CH. Pressure ulcer prevention and management. JAMA 2003;289:223-6.
7. Kottner J, Tannen A, Dassen T. Hospital pressure ulcer prevalence rates and number of raters. J Clin Nurs 2009;18:1550-6.
8. Landi F, Onder G, Russo A, Bernabei R. Pressure ulcer and mortality in frail elderly people living in community. Arch Gerontol Geriatr 2007;44(Suppl 1):217-23.
9. Thomas DR, Goode PS, Tarquine PH, Allman RM. Hospital-acquired pressure ulcers and risk of death. J Am Geriatr Soc 1996;44:1435-40.
10. Kuwahara M, Tada H, Mashiba K, Yurugi S, Iioka H, Niitsuma K, et al. Mortality and recurrence rate after pressure ulcer operation for elderly long-term bedridden patients. Ann Plast Surg 2005;54:629-32.
11. Graves N, Birrell FA, Whitby M. Modeling the economic losses from pressure ulcers among hospitalized patients in Australia. Wound Repair Regen 2005;13:462-7.
12. Lyder CH, Wang Y, Metersky M, Curry M, Kliman R, Verzier NR, et al. Hospital-acquired pressure ulcers: results from the national medicare patient safety monitoring system study. J Am Geriatr Soc 2012;60:1603-8.
13. Brem H, Maggi J, Nierman D, Rolnitzky L, Bell D, Rennert R, et al. High cost of stage IV pressure ulcers. Am J Surg 2010;200(4):473-7.
14. Smith S. Incidence of hospital-acquired pressure ulcers in acute care using two different risk assessment scales: Results of a retrospective study. Ostomy Wound Manage 2011;57(5):20-7.
15. Baumgarten M, Margolis DJ, Localio AR, Kagan SH, Lowe RA, Kinosian B, et al. Pressure ulcers among elderly patients early in the hospital stay. J Gerontol A Biol Sci Med Sci 2006;61(7):749-54.
16. Pham B, Teague L, Mahoney J, Goodman L, Paulden M, Poss J, et al. Early prevention of pressure ulcers among elderly patients admitted through emergency departments: a cost-effectiveness analysis. Ann Emerg Med 2011;58(5):468-78.
17. Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers. A systematic review. JAMA 2008;300(22):2647-62.
18. Jaul E. Assessment and management of pressure ulcers in the elderly: current strategies. Drugs Aging 2010;27:311-25.
19. Thomas DR, Kamel HK. Wound management in postacute care. Clin Geriatr Med 2000;16(4):783-804.
20. Wang H, Niewczyk P, Divita M, Camicia M, Appelman J, Mix J, et al. Impact of pressure ulcers on outcomes in inpatient rehabilitation facilities. Am J Phys Med Rehabil 2014;93(3):207-16.
21. Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive Geriatric Assessment: A meta-analysis of controlled trials. Lancet 1993;342:1032-6.
22. Granger CV, Albrecht GL, Hamilton BB. Outcome of comprehensive medical rehabilitation: measurement by PULSES Profile and the Barthel Index. Arch Phys Med Rehabil 1979;60:145-54.
23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:145-54.
24. Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research and policy implication of a core geriatric concept. J Am Geriatr Soc 2007;55:780-91.
25. NANDA International. Diagnósticos enfermeros. Definiciones y clasificación 2012-2014. Barcelona: Elsevier, 2012. pp. 568.
26. Mas MA, Renom A, Vazquez O, Miralles R, Bayer AJ, Cervera AM. Interruptions to rehabilitation in a geriatric rehabilitation unit: associated factors and consequences. Age Ageing 2009;38(3):346-9.
27. Baumgarten M, Margolis DJ, Orwig DL, Shardell MD, Hawkes WG, Langenberg P, et al. Pressure ulcers in elderly patients with hip fracture across the continuum of care. J Am Geriatr Soc 2009;57(5):863-70.
28. Jaul E, Calderon-Margarit R. Systemic factors and mortality in elderly patients with pressure ulcers. Int Wound J 2013. DOI:10.1111/iwj.12086.
 Correspondence:
Correspondence:
Sebastià Santaeugènia.
El Carme Intermediate Care Hospital.
Carrer Sant Jeroni de la Murta, 60.
08917 Badalona, Barcelona. Spain
e-mail: ssantaeugenia@bsa.cat
Received: 23/02/2017
Accepted: 02/05/2017