Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.34 no.6 Madrid nov./dic. 2017
https://dx.doi.org/10.20960/nh.1102
Food intake, plate waste and its association with malnutrition in hospitalized patients
Ingesta y desperdicio de alimentos y su asociación con la desnutrición hospitalaria
Kobra Simzari1, Davoud Vahabzadeh2, Sakineh Nouri Saeidlou3, Susan Khoshbin4 and Yener Bektas5
1Department of Nutrition and Dietetics. Faculty of Health Sciences. Hacettepe University. Ankara, Turkey.
2Maternal and Child Obesity Research Center (MCORC). Urmia University of Medical Sciences. Urmia, Iran.
3Food and Beverages Safety Research Center. Urmia University of Medical Sciences. Urmia, Iran.
4BSc in Nutrition. Nutrition Unit. Alavi Hospital. Ardabil University of Medical Sciences. Ardabil, Iran.
5Department of Anthropology. Faculty of Science and Literature. Ahi Evran University. K?rsehir, Turkey
ABSTRACT
Background: Hospital malnutrition is a worldwide dilemma and challenge. High levels of plate waste contribute to malnutrition-related complications in hospital. We investigated the association between the levels of plate waste, food intake and patient satisfaction with nutritional risk and malnutrition prevalence in three hospital settings.
Methods: The sample population of 120 patients, aged 18-65 year, admitted consecutively over a 12 month period to 3 different educational university hospitals was included. For all the patients, diet history, anthropometric measurements, body mass index and patient satisfaction with the hospital food service was evaluated. Weight plate waste for all daily meals was done and actual intakes computed individually for each day. Nutrition risk screening (NRS)-2002 (≥ 3) tool was used for estimating the nutritionally at-risk population.
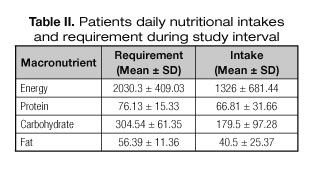
Results: From one hundred twenty non-critically ill patients with a mean 8.9 ± 3.5 day length of hospital stay, 40.8% (49) were men and 59.2% (71) were female. Mean energy and protein requirements were 2,030.3 ± 409.03 kcal/day and 76.13 ± 15.33 g/day respectively. Mean intakes were 1,326 ± 681.44 kcal/day and 66.81 ± 31.66 g/day respectively. The mean percent of plate waste for lunch and dinner were 37.7 ± 29.88 and 30.4 ± 23.61 respectively. In the total population, 25% of patients were satisfied and 75% patients were unsatisfied with hospital foods. Based on BMI (< 20), unintentional weight loss (> 10%), malnutrition prevalence was 12.5% and 14.2% respectively during hospitalization. The prevalence of nutritionally at-risk population was 30% at admission time and reached 33.3% at discharge.
Conclusion: Plate waste and hospital malnutrition were highly prevalent in accompanying with increasing nutritionally risk progression. So it should be addressed as an important health issue and appropriate strategies for stimulating governmental policies should be adopted.
Key words: Food intake. Plate waste. Hospitalized patients. Iran.
RESUMEN
Introducción: la desnutrición hospitalaria constituye a la vez un problema y un reto. Una cantidad grande de desperdicio en el menú hospitalario se correlaciona con mayor incidencia de complicaciones asociadas a la desnutrición. Se evalúa en este trabajo la asociación entre la cantidad de comida desechada, el consumo real y la satisfacción de los pacientes con la prevalencia de desnutrición y de riesgo nutricional en tres hospitales iraníes.
Métodos: se evaluó una muestra de 120 pacientes, de 18 a 65 años, ingresados a lo largo de 12 meses en tres hospitales universitarios de distinto nivel. Se recogieron datos de la historia dietética, las medidas antropométricas, el índice de masa corporal y el grado de satisfacción de los pacientes con el menú servido. Se pesó el desperdicio de las bandejas de alimentación y la ingesta diaria de cada paciente. El riesgo nutricional se evaluó mediante la herramienta NRS-2000, estimando el riesgo cuando la puntuación era ≥ 3.
Resultados: se incluyeron 120 pacientes no críticos, con una duración media de hospitalización de 8,9 ± 3,5 días. El 40,8% (49) eran varones. Los requerimientos energéticos medios eran 2.030,3 ± 409,03 kcal/día y los proteicos de 76,13 ± 15,33 g/día. La ingesta media fue de 1.326 ± 681,44 kcal/día y la proteica de 66,81 ± 31,66 g/día. Se desperdició en la comida y en la cena una media del 37,7 ± 29,88 y 30,4 ± 23,61 respectivamente. Solo un 25% de los pacientes estaban satisfechos con la dieta. Un 12,5% de los pacientes tenían un IMC < 20 y un 14,2% una pérdida no intencionada de peso > 10%. La prevalencia de riesgo nutricional era del 30% al ingreso y del 33,3% al alta.
Conclusión: el desperdicio de la comida en el hospital y la desnutrición hospitalaria tienen una alta prevalencia en la muestra estudiada, que se acompañaban de un mayor riesgo nutricional. Las administraciones públicas deberían abordar este problema y desarrollar estrategias de prevención adecuadas.
Palabras clave: Ingesta. Desperdicio. Hospitalización. Irán.
BACKGROUND
Hospital malnutrition is a worldwide dilemma and challenge (1). Malnutrition in the hospital has been identified as a problem for about 40 years (2). It has been reported that there is a wide difference in prevalence rates of malnutrition. Some are primarily due to the fact that the studies included different populations and used different methods (3,4). But an international consensus has been reached that at least 30% to 50% of hospitalized patients suffer from malnutrition (1,5). This can be worsened if remained untreated during the hospital stay. The association between malnutrition, increased morbidity, prolonged hospital stay, and poor survival is well established (6-8).
Hospital food must contribute to preventing undernutrition or limit its development during hospital stay (7,9,10). Reduction of dietary intake during a hospital stay, alongside with the increase of energy requirements, is the main cause of hospital undernutrition and can contribute to its worsening. Several studies have shown that decreased food intake is associated with increased complications and mortality during hospital stay (8,11), so an upward trend between reduced intake and mortality has been proposed by some studies (12,13).
Satisfaction of patients with an acceptable quality of meals within a hospital care system constitutes one of the main attempts to reducing malnutrition appearance (6). Recently proposed methods such as measuring meal wastage can better quantify the acceptability of a given menu (14,15). High levels of plate waste contribute to malnutrition-related complications in the hospital (2). Plate waste in hospitals can be defined as the amount of uneaten served food by inpatients (6). Generally, when daily menus cannot offer all food choices and automatically serve vegetables or other standardized portions, meal wastage increases (2,16).
Plate waste can be done by weighing food or by visual estimation of the amount of food remaining on the plate (2,12), that can be used to evaluate the adequacy of food intake and the efficiency of meal provision (2,6). Quantification of the weight lost in served trays is equal to the amount of food that consumed by the patient (12,14,17). One of the methods for evaluating patient nutritional status is NRS (Nutrition Risk Screening). NRS-2002 is a tool for nutrition risk evaluation in adults in the hospital setting, that if the score be ≥ 3; the patient will be nutritionally at-risk and a nutritional care plan should be initiated (3,4,18).
The current study was done with the aim of investigating the association between the levels of plate waste, food intake and patient satisfaction with nutritional risk and malnutrition prevalence in hospital settings.
MATERIAL AND METHODS
Subjects
Data on 120 patients, aged 18-65 years, admitted consecutively over a 12 month period to 3 different educational university hospitals in Ardabil from Iran were collected. Patients with the length of stays equal to 7 or more days were included. The inclusion criteria were: being 18-65 years old, feeding initiation within first 36 h after hospital admission, lack of enteral or parenteral nutritional support, not to being NPO, being able to give written consent form, hospital staying for longer than 2 days. Informed consent was obtained individually from all included participants in the study.
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki Declaration and its later amendments or with comparable ethical standards.
Demographic and anthropometric data gathering
For all the patients, demographic data and anthropometric measurements including weight, height, body mass index (BMI), usual weight and patients' weight change history in the last six months were recorded. In addition, other data regarding diagnosis, hospitalization, past medical or surgery history, and drug prescriptions were collected. All patients' body weight was measured in light clothes with a portable electronic scale (Seca 910, Hamburg, Germany) to the nearest 0.1 kg and height was measured with a portable stadiometer to the nearest 0.1 cm.
Nutritional assessment
A simple previously prepared checklist was used to record the amount of food eaten by patients. For consistency and lack of variation in data collection, all data about meals were gathered by one undergraduate nutritionist. Weight plate waste for all daily meals was measured and actual intakes computed individually for each day. Patients based on level of food consumption were classified into four categories: a) patients with all amount of consumed food; b) those with equal and more than 50% consumed food; c) those with less than 50% consumed food; and d) those who did not consumed any amount of delivered foods during meal. Moreover, the percent of satisfied energy and macronutrients during meals was determined.
Malnutrition prevalence was estimated based on BMI (< 20) and unintentional weight loss (> 10%). Nutritional risk evaluation was done in two separate times; 1) within 48 hours after admission; and 2) at discharge time. The patients with a final NRS
≥ 3 on admission were considered suffering from malnutrition. In patients with the lack of malnutrition at first evaluation, a re-evaluation was done during last one week or earlier. Score; 1 was used for a patient with chronic disease, admitted to hospital due to complications. Score; 2 was used for a patient confined to bed due to illness, e.g. following major abdominal surgery. Score; 3 was used for a patient in intensive care with assisted ventilation. Patients with score; 3 were considered severely undernourished or severely ill. Patients with scores equal to 2 and more were moderately undernourished and patients with scores equal to 1 and more than 1considered mild undernourishment.
Statistical analysis
The variables tested for normality distribution by the Kolmogorove-Smirnov test. T-test was recruited for variables with normal distribution, Mann-Whitney test was taken for comparison between non-parametric variables. Chi-square test was applied for qualitative variables. Frequency and other descriptive tests such as mean, standard deviation, etc. were done for any of the necessary items. p value as much as 0.05 was considered for significances. All data analysis was carried out by SPSS v.18 for windows.
RESULTS
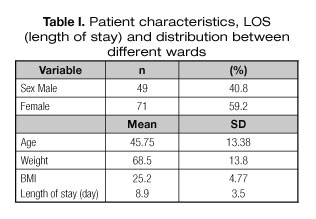
Results showed that 40.8% (49) were men and 59.2% (71) were female. Mean age for total population was 45.75 ± 13.38 and 46.3 ± 12.17 years old respectively. Mean weight and BMI at admission time was 68.5 ± 13.8 20 kg and 25.2 ± 4.77. Based on BMI, unintentional weight loss (> 10%), malnutrition prevalence at admission time was 12.5 and 14.2 respectively. Table I shows the patient numbers, distribution, and LOS in different wards and table II shows their daily nutritional intakes and requirement.
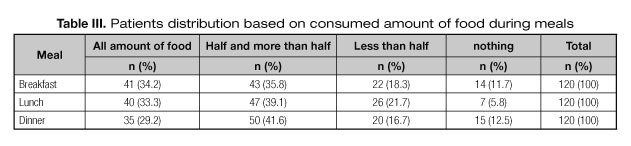
Results showed that greatest number of patients with all amount of food intake were in the breakfast meal (34.2%), based on the monitoring of leftovers. In this population, 11.7%, 5.8% and 12.5% of patients were those with the lack of intake during breakfast, lunch, and dinner respectively (Table III).
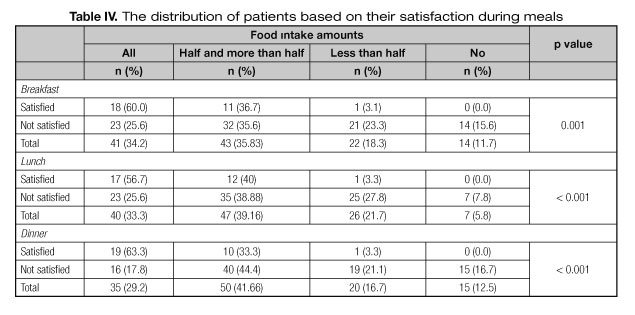
There was a significant difference between food intake in breakfast, lunch, and dinner (Table IV). In the total population, 25% of patients were satisfied and 75% patients were unsatisfied with hospital foods. Sixty per cent of satisfied and 25.6% of unsatisfied patients consumed total amount of delivered breakfast; 56.7% of satisfied and 25.6% of unsatisfied patients consumed total amount of delivered lunch; 63.3% of satisfied and 17.8% of unsatisfied patients consumed total amount of delivered dinner.
The mean percent of plate waste for lunch and dinner were 37.7 ± 29.88 and 30.4 ± 23.61 respectively. The minimum leftover amount was for breakfast; 26.7 ± 29.01. Mean total daily percent of plate waste was 31.3 ± 23.36.
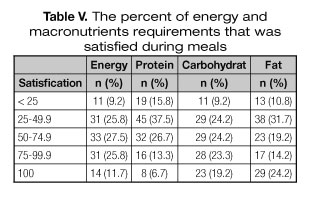
The percent of satisfied energy and macronutrients can be seen in table V. These results showed that 9.2% of patients had intakes less than 25% of their daily energy requirements; only 11.7% of patients have intakes according to their daily energy requirement. Data about other macronutrient has been presented in table V. In regard protein, carbohydrate, and fat 15.8%, 9.2% and 10.8% recieved less than 25% of their daily requirement, respectively.
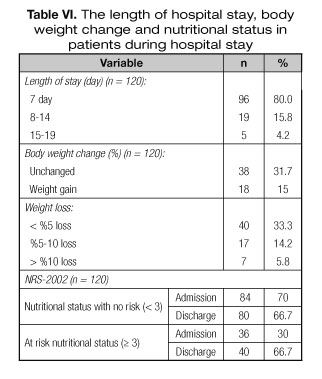
Mean length of stay (LOS) for this studied population was 8.05 days. During hospitalization time in 31.7% of patients, body weight was unchanged, 15% of patients experienced weight gain. Weight reduction took place in 53.3% of subjects. Average weight loss and weight gain were 2.8 ± 2.31 kg and 1.8 ± 8.3 kg respectively. Based on NRS screening tool for determining patient at nutritional risk, 33.3% of participants were at risk at discharge time (Table VI).
Mean BMI at admission time was 25.2 ± 4.77 and in discharge time was 24.8 ± 4. Comparing patient nutritional status based on BMI between admission and discharge time, showed a significant difference (< 0.001).
DISCUSSION
Malnutrition is common in hospital patients and has a negative effect on disease outcome and increasing the duration of the hospital stay. This study was aimed to report the nutritional risk and the prevalence of malnutrition in patients admitted to three different hospitals in Ardabil. The used tool in this study for the nutritional evaluation was NRS-2002. In the current study, the percent of nutritionally at-risk population based on NRS assessment were 30% at admission time and 33.7% in discharge time, indicating an increase about 3.7% in nutrition risk during hospital staying period. Such increasing amount has been presented in other studies (12,19); for example in the study of Kandiah et al., it has been postulated that the percent of malnutrition showed an increase in different amounts based on diagnosed diseases type during hospital stay (12,19). In the Hernández study a decrease in the percent of malnutrition based on weight change trends and BMI during hospitalization has been indicated (3). Furthermore in our study based on BMI (< 20), unintentional weight loss (> 10%) malnutrition prevalence estimated 12.5, 14.2 and 15.8 respectively. There are various studies involving the NRS 2002 for the detection of nutritionally at-risk population in hospitals. Some of them have reported greater prevalence than 30% among hospitalized patients (10,20,21), while some others carried out in other areas (15,19) reported lower percentages of malnutrition than ours. The different results are probably due to the fact that various methods for diagnosing malnutrition have been used.
Plate waste has an important effect on malnutrition-related complications and weight loss during hospital stay (16,22,23). It has been showed that there will be a two-fold increase in the risk of patient's mortality during hospital admission if they eat only one-quarter of their provided food (2,11). Unfortunately, there is still a lack of evidence to support interventions to improve this problem. In present study mean plate waste was 31.3% by weight. In one Meta-analysis of 32 studies (2), carried out in 29 countries, the median reported plate waste have been 30% of the plated food weight. In this study the minimum leftover amount was for breakfast in agreement with most previous published studies (2,14). In above mentioned studies they have indicated less plate waste in breakfast compared to other main meals. In our study, 9.2% of patients had intakes less than 25% of their daily energy requirements; 25.8% received 50-75% of their calculated needs; 27.5% received 75-100% of their calculated needs. Only 11.7% of patients had intakes according to their daily energy requirement. For protein, daily calculated satisfied needs for above-mentioned categories were 15.8, 37.5, 26.7, 13.3 and 6.7% respectively. In the study of Fernandez et al. (24) it has been indicated that 25% of the diets have been able to cover the energy needs and only one diet have been able for covering the protein needs. In other studies such as Roosemalen et al. (22), sixty-one percent of patients achieved < 90% of their energy requirements, and in regard the protein 75% achieved < 90% of their protein requirements. Nineteen percent of patients consumed > 110% of their calculated needs for energy, and 14% of patients consumed > 110% of their calculated needs for protein.
In that study they categorized patients based on below ranges: patient with every eaten foods were patients with eating 86%-100% their provided meals, patient with more than half eaten were patients with eating 51%-85% provided amount of their meals, patients with less than half eaten were patients with eating 16%-50% of provided meals, and finally "nothing ate" patients were whom with eating 0%-15% of provided meals. In our study, categorization was different. In our study parallel ranges were 75%-100%, 50%-75%, 25%-50%, and 0%-25%, respectively. In this study like above-mentioned study, mean plate waste has reported as a percent of daily provided food, but in others the amount of daily plate waste as a percent of daily provided energy and protein have been reported (7,14).
Patient satisfaction can be affected by the amount of wasted meal since patients report can be upset by the amount of wasted food. Previously published studies performed in other hospital care settings have concluded that there is some evidence to suggest that a more personalized meal service system in hospitals has the ability to improve energy intakes and patient satisfaction (12). In the present study, 25% of patients were satisfied and 75% patients were unsatisfied with hospital foods. Sixty percent of satisfied patients and 25.6% of unsatisfied patients consumed all of the delivered food in the breakfast. These amounts were 60%, 25.6% for lunch and 63.3, 17.8% for dinner meal, respectively. In the study of Roosemalen et al. (22), it has been showed that 83% of the patients were satisfied or fairly satisfied with the choices offered at mealtimes. Eighty-three per cent were satisfied or fairly satisfied with the taste of the meals, 88% were satisfied with the presentation of the meals and with the tools provided. Sixty-three percent of patients reported that they consumed all ordered amount of foods. In other studies such as Dupertuis et al. (7), it has been indicated that less than 10% of the patients considered hospital meals unacceptable.
In our study, main causes for reducing intake and elevation of wasted food amounts was nausea, dry mouth, and unwillingness, while in other studies (22) in parallel with us a fair or poor appetite have been reported as a cause for the lack of eating a complete meal, irrespective of ordered meal size. In other studies (2,7,11) other factors such as more staying in hospital, prepared special diet, lack of oral nutritional supplements (ONS) intakes, low quality delivered meals, type of diagnosed disease, poor food quality, inappropriate portion sizes, limited menu choices, inappropriate meal times, interruptions, and unpleasant surroundings have been mentioned. In others, inadequate taste and absence of choice have been introduced as factors related to reduced intake amount (7).
During the study interval, sixty-four patients (53.33%) lost their weight. Forty (33.3%) have < 5% weight loss, seventeen (14.2%) have 5-10% weight loss and seven (5.8% 7) with > 10% weight loss. In this subgroup (64 patients), in 7 patients (10.9%), more than 75% of provided food was wasted at the breakfast meal. In other words, they consumed only about less than 25% of their offered food. Also, we observed that about 57.1% of these subjects lost more than 10% of their weight during the hospitalization period. Therefore statistical analysis showed that amount of wasted food in breakfast meal was significantly associated with weight loss during a hospital stay, but it was not significant for other meals. In the study of Barton et al., 112 patients lost an average weight about 7.2% of their initial weight, with the greatest weight loss in those who were the most undernourished on admission. In another study, weight loss has been reported in 52.7% of all participants (20), also it has been stated by Ross that 81% of all participants in their study were at a significant risk of future weight loss owing to their poor appetite (25). In Pirlich´s study (21), results in regard the percent of weight loss in relation to the amount of dietary intake and malnutrition prevalence during hospitalization has been discussed. In another study, weight loss during the previous 6 months has reported in 28.9% of patients. In that study, weight loss has been higher in the group with cancer compared with patients with other diseases (19).
In this study, plate waste and malnutrition were high concurrently. High wastage rates were associated with inadequate energy and protein intakes, which this may help to explain patients' weight loss during a hospital stay. This high malnutrition prevalence should be addressed as an important issue in hospital clinical care. Some attempts have been made to develop targets for acceptable plate waste levels, but yet more attempts need to be done for providing adequate patient food intakes and improve nutritional care efficiency. Ultimately it is important for each hospital to monitor their own performance and strive to find effective ways for improving the nutritional intakes of vulnerable patients. One way to achieving this target will be minimizing plate waste as much as possible.
The small number of the study population was one of the limitations in the current study. This limitation was inevitable because all university educational hospitals in this province were included and there were no more hospital and patients for inclusion. So we think that it could be better to do such study in a multicenter design. In this time it was impossible, because of the study design entity that was for a specific curriculum course. Another limitation was fast patients turnover and reduced subject's involvement in the study. Some were because of a limited existent number of beds for patient hospitalization. In turn, some advantages from this study can be counted as calculation of weighted plate waste in compare with some other previous studies that they have calculated or estimated just visual plate waste in their investigation. Another advantage can be population homogeneity since all included patients were Azari and just from one native territory.
Finally, as the main conclusion from this study, it can be derived that hospital malnutrition is highly prevalent in concurrent with a high rate of plate waste and nutritional risk. So it should be addressed as an important health issue and appropriate strategies for stimulating governmental policies should be adopted.
ACKNOWLEDGMENT
The authors are grateful to all physicians and nurses from the Ardabil hospitals for their assistance with data collection.
REFERENCES
1. Correia MIT, Campos ACL, Study EC. Prevalence of hospital malnutrition in Latin America: The multicenter ELAN study. Nutrition 2003;19(10):823-5.
2. Williams P, Walton K. Plate waste in hospitals and strategies for change. e-SPEN, the European e-Journal of Clinical Nutrition and Metabolism 2011;6(6):e235-e41.
3. Álvarez Hernández J, Planas Vilá M, León Sanz M, Garcia de Lorenzo y Mateos A, Celaya S, García Lorda P, et al. Prevalence and costs of multinutrution in hospitalized patients; the PREDyCES study. Nutr Hosp 2012;27(4):1049-59.
4. Mercadal-Orfila G, Lluch-Taltavull J, Campillo-Artero C, Torrent-Quetglas M. Association between nutritional risk based on the NRS-2002 test and hospital morbidity and mortality. Nutr Hosp 2012;27(4):1248-54.
5. Waitzberg DL, Caiaffa WT, Correia MIT. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition 2001; 17(7):573-80.
6. Valero Díaz A, Caracuel García A. Evaluation of factors affecting plate waste of inpatients in different healthcare settings. Nutr Hosp 2013; 28(2):419-27.
7. Dupertuis Y, Kossovsky M, Kyle U, Raguso C, Genton L, Pichard C. Food intake in 1707 hospitalised patients: a prospective comprehensive hospital survey. Clin Nutr 2003;22(2):115-23.
8. Gheorghe C, Pascu O, Iacob R, Vadan R, Iacob S, Goldis A, et al. Nutritional risk screening and prevalence of malnutrition on admission to gastroenterology departments: a multicentric study. Chirurgia (Bucur) 2013;108(4): 535-41.
9. Beck AM, Balkn U, Fürst P, Hasunen K, Jones L, Keller U, et al. Food and nutritional care in hospitals: how to prevent undernutrition?report and guidelines from the Council of Europe. Clin Nutr 2001;20(5):455-60.
10. Ofei K, Dobroczynski M, Holst M, Rasmussen H, Mikkelsen B, editors. The Dietary Intake Monitoring System (DIMS)-an Innovative Device for Capturing Patient's Food Choice, Food Intake and Plate Waste in a Hospital Setting. Proceedings of Measuring Behavior; 2014.
11. Thibault R, Chikhi M, Clerc A, Darmon P, Chopard P, Genton L, et al. Assessment of food intake in hospitalised patients: a 10-year comparative study of a prospective hospital survey. Clin Nutr 2011;30(3):289-96.
12. Kandiah J, Stinnett L, Lutton D. Visual plate waste in hospitalized patients: length of stay and diet order. J Am Diet Assoc 2006;106(10):1663-6.
13. Calleja Fernandez A, Vidal Casariego A, Cano Rodriguez I, Ballesteros Pomar MD. Adequacy of hospital diets to inpatients' nutritional requirements. Nutr Hosp 2016;33(1):80-5.
14. Grieger J, Nowson C. Nutrient intake and plate waste from an Australian residential care facility. Eur J Clin Nutr 2007;61(5):655-63.
15. Saccares S, Scognamiglio U, Moroni C, Marani A, Calcaterra V, Amendola M, et al. Evaluation model of plate waste to monitor food consumption in two different catering settings. Italian Journal of Food Safety 2014;3(2).
16. Barton A, Beigg C, Macdonald I, Allison S. High food wastage and low nutritional intakes in hospital patients. Clin Nutr 2000;19(6):445-9.
17. Almdal T, Viggers L, Beck AM, Jensen K. Food production and wastage in relation to nutritional intake in a general district hospital-wastage is not reduced by training the staff. Clin Nutr 2003;22(1):47-51.
18. Lisboa da Silva D1, Alves Santos P, Coelho Cabral P, Pessoa de Araujo Burgos MG. Nutritional screening in clinical patients at a University Hospital in Northeastern Brazil. Nutr Hosp 2012;27(6):2015-9.
19. Pablo AR, Izaga MA, Alday LA. Assessment of nutritional status on hospital admission: nutritional scores. Eur J Clin Nutr 2003;57(7):824-31.
20. Wyszynski DF, Perman M, Crivelli A. Prevalence of hospital malnutrition in Argentina: preliminary results of a population-based study. Nutrition 2003;19(2):115-9.
21. Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr 2006;25(4):563-72.
22. Roosemalen MM, Weijs PJ, Langius JA. High waste contributes to low food intake in hospitalized patients. Nutr Clin Pract 2012;27(2):274-80.
23. Barendregt K, Soeters PB, Allison SP, Kondrup J. Basic concepts in nutrition: Diagnosis of malnutrition-Screening and assessment. e-SPEN, the European e-Journal of Clinical Nutrition and Metabolism 2008;3(3):e121-e5.
24. Fernández AC, de la Maza BP, Casariego AV, Taibo RV, Gómez JL, Rodríguez IC, et al. Food intake and nutritional status influence outcomes in hospitalized hematology-oncology patients. Nutr Hosp 2015;31(6):2598-605.
25. Ross LJ, Wilson M, Banks M, Rezannah F, Daglish M. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition 2012;28(7):738-43.
 Correspondence:
Correspondence:
Sakineh Nouri Saeidlou.
Food and Beverages Safety Research Center.
Urmia University of Medical Sciences.
Urmia, Iran
e-mail: saeedlou2003@yahoo.com
Received: 09/03/2017
Accepted: 15/03/2017