INTRODUCTION
The prevalence of sedentary life in adults and children continues to rise globally. At least 60% of the world population does not perform the necessary physical activity to prevent obesity and related noncommunicable diseases (NCDs) 1. And Chile is not an exception. According to a 2012 report of physical fitness in schools, 70% of Chilean students in 8th grade had unsatisfactory aerobic fitness levels and lived predominantly sedentary lives 2, spending > 10 hours in activities of low energy expenditure and excessive time in front of a screen (television or computer) 3) (4. Obesity and a sedentary lifestyle during childhood leads to poor physical fitness, increasing the risk for obesity, metabolic syndrome and cardiovascular disease in adulthood. These consequences have not been sufficiently studied in children. Thus we considered of interest to assess the association between physical fitness and cardiometabolic risk (CMR) to strengthen the call for more physical activity in children and adolescents. We further hypothesized that the evidence of prolonged heart rate recovery time in young children might motivate parents to act at an early stage, thus preventing further deterioration 5.
Heart rate recovery (ΔHRR) reflects the functional capacity of autonomic nervous system 6 and perhaps could be considered a measure autonomic dysfunction 7. Additionally, adults with high cardiorespiratory fitness recover faster than adults with lower level physical fitness 8. Metabolic risk factors are inversely associated with ΔHRR in healthy children and adolescents 9. The physiological mechanism underlying heart rate recovery after exercise in children operates faster than in adults; smaller heart size, relative muscle mass, perfusion distance and faster cardiorespiratory circulation time kinetics explain most of the difference 10. Simhaee et al. showed that children with high body mass index (BMI) have a longer heart rate recovery time and that those with faster recovery have more moderate to vigorous physical activity. Other studies show that there is a direct correlation between sedentary behavior and increased heart rate recovery 9. A cross-sectional study of 993 healthy adolescents of 12-19 years of age shows that heart rate recovery time was inversely related to metabolic risk factors (waist circumference, systolic blood pressure, plasma triglycerides, levels of C-reactive protein) and positively related to circulating HDL levels 11. Prolonged heart rate recovery time, which reflects a deteriorating physical condition, might be useful to detect children with elevated CMR. Thus, it is important to further investigate the link between heart rate recovery time and cardiovascular/metabolic risk in children 9. The aim of this cross-sectional study was to explore the association between physical fitness (6-minute walk test and muscle strength) and CMR, with heart rate recovery, in a group of Chilean schoolchildren aged 6-9 years.
MATERIALS AND METHODS
POPULATION
The study sample comprised 478 6-9 years-old children (n = 216 girls) participating in the Growth and Obesity Cohort Study (GOCS) conducted in Santiago, Chile. GOCS is a study of low-middle income Chilean children born in 2002-2003 (n = 1,196, ~ 50% girls), of normal gestation 37-42 weeks with birth weight ≥ 2,500 g 12. The study was approved by the Ethics Committee of the Institute of Nutrition and Food Technology, University of Chile. All parents/legal guardians agreed to the participation of their children by signing the free informed consent form.
ASSESSMENT OF PHYSICAL FITNESS (PF)
Muscle strength was evaluated testing upper body strength (arms, handgrip strength) using a (Baseline 12-0286(r)) digital force gauge 13 and lower body strength (legs) was assessed by the standing long jump 14. Aerobic fitness was evaluated with the submaximal six minute walk test (6MWT) 15. Heart rate (HR) was measured and recorded with a heart rate monitor (Polar model FS1C): at rest before the test, then every three minutes, and finally one minute after test completion. Test results were expressed in meters traveled divided by the height of each child. The results of grip strength and jump were expressed in relative values, as the fat-free mass and length of stride of participants significantly modify the absolute values. We created an overall z-score of physical fitness (6MWTz/height + grip strength Z/weight + jump Z/height/3), and categorized "low" physical fitness as < -1 SD; "intermediate", between 1 and -1 SD; and "high", as > 1 SD.
NUTRITIONAL ASSESSMENT
All children were measured in duplicate for weight (light clothing), standing at the center of a Tanita Body Composition Analyser BC-418, with 100 g precision and 220 kg capacity; height (Frankfurt methodology using a portable SECA, 222 stadiometer with upper range 200 cm and divisions of 1 mm) 16; and waist circumference, with an automatic locking tape (SECA) measured above the rim of the iliac crest, through the navel 17. Average height and weight measurements were used to determine BMI.
BODY COMPOSITION
In a sub-sample of 122 boys and 92 girls, fat-free mass was estimated by total body water with bioelectrical impedance using Tanita BC-418MA, eight-electrode, hand-to-foot system, manufactured by Tanita Corporation (Tokyo, Japan) 18. We observed a high correlation between body weight and fat free mass (r = 0.95, p < 0.001).
CMR-z
We evaluated CMR based on glucose, fasting insulin levels and lipid profile. CMR defined z ≥ 1.29 (90th percentile), from the score of the variables included in the equation (waist circumference-Z + glucose-Z + insulin-Z + triglycerides-Z - HDL-Z/5) 19. We used USA cut-offs for waist circumference 17 and plasma lipids 20, and blood glucose and insulin based on Chilean data 21. Insulin and HOMA were classified based on the centile distribution of Chilean children 6-15 years 22. The 75th centile for Tanner 1 (HOMA: 2.1) was used as a cut-off to diagnose insulin resistance.
HEART RATE RECOVERY
We calculated a change in heart rate recovery (ΔHRR) as the difference between heart rate at the end of the 6MWT and after the one minute rest. Later, differences were classified in quartiles. The lowest quartile represented better recovery.
STATISTICAL ANALYSIS
After analyzing the distribution of variables, data were expressed with means ± SD. Continuous variables were compared by sex and age range. To study the association between heart rate recovery and overall physical fitness (PF-z), insulin and HOMA, either Pearson or Spearman correlation coefficients were used. The associations between physical condition (lower, middle, top) and heart rate recovery (in quartiles) were evaluated with Chi-squared tests. Finally, the Student's t-test was used to compare the ΔHRR, according to presence or absence of insulin resistance, and ANOVA was used to assess whether heart rate recovery varied by nutritional status and CMR. A p value < 0.05 was considered to be statistically significant.
RESULTS
The characteristics of the sample are summarized in Table I. A total of 478 students (54.8% boys) of 8.3 ± 0.7 years were included in this study. When analyzing the results by sex, girls had lower resting HR, HR maximum and z-PF (p < 0.001), and the like ΔHRR (beats/minute) than boys. The prevalence of obesity was significantly higher in boys than in girls (15% and 7%, respectively; p < 0.01).
Table I Basic characteristics of the sample

p < 0.01. BMI: body mass index; ΔHRR: change in heart rate recovery; a: differences by sex; b: differences by age range in boys; c: differences by age range in girls.
After calculating cut-offs for ΔHRR quartiles (< 41, 41-58, 58-80 and > 80), no differences were found by sex or age range, although we found a higher % of girls in the top two quartiles ΔHRR (60% girls vs 45% children). The ΔHRR was lower in schoolchildren with normal nutritional status compared with those who were obese (p = 0.03) (Fig. 1); no differences were found in analyzing the results by sex and age range.
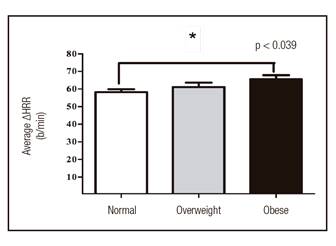
Figure 1 Mean ΔHRR by nutritional status in schoolchildren aged 6-9 years. Anova, Bonferroni. p value represents trend between groups. Average ∆RHR: normal (58.2 ± 25.8 l/min), overweight (61.2 ± 26.8 l/min), obesity (66.0 ± 23.4).
The characteristics of the physical fitness tests are summarized in Table II. In the jumping test, adjusted for height, boys jumped significantly more than girls (94 vs 84 cm, p < 0.01), a difference that was not maintained in tests of grip strength/weight and 6MWT/height. Studying the data by nutritional status, normal weight subjects scored better on tests of muscle strength and aerobic capacity than those who were overweight or obese (p < 0.001). In analyzing the results of physical fitness according to z-FP, 85% of schoolchildren had an intermediate fitness level (+/- 1 SD).
Table II Physical fitness characteristics by sex and age range
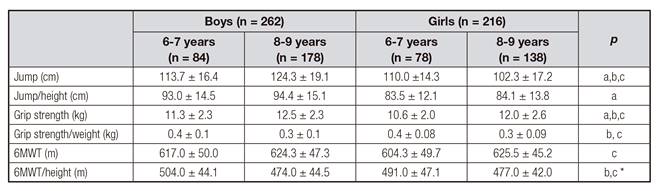
p < 0.01; *p 0.02. 6MWT: 6 minute walking test; a: differences by sex; b: differences by age range in boys; c: differences by age range in girls.
Table III shows the cardiovascular and metabolic profile and CMR score by sex and nutritional status. There were statistically significant differences in blood glucose and HDL-C by sex. Nutritional status, waist circumference, triglycerides, insulin and HOMA were also significantly different.
Table III Cardiometabolic profile, HOMA and CMR-z score by sex and nutritional status
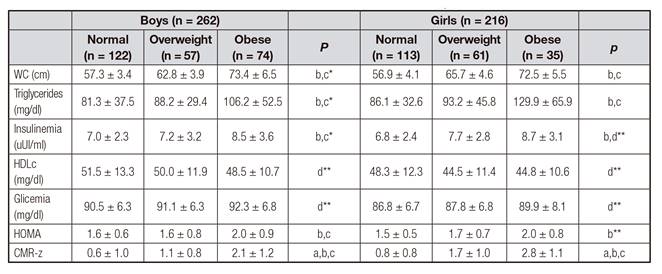
p < 0.01; *p = 0.04; **p < 0.001. WC: waist circumference; CMR-z: cardiometabolic risk score; a: differences between normal weight and overweight; b: differences between normal weight and obese; c: differences between overweight and obesity; d: differences by sex.
Thirteen and seventeen percent of schoolchildren had hyperinsulinemia and altered HOMA, respectively; 44% of them had high CMR scores (≥ z: 1.29); and no differences by sex or age were found. Children with overweight and obesity had higher CMR-z than normal children (Table III). However, no relationship between ΔHRR and CMR-z were observed, except for z value for insulin and HOMA, in this group. (r = 0.4; p < 0.001). When comparing schoolchildren with and without insulin resistance, we noted that this condition was associated with increased ΔHRR (72.4 vs 58.2 l/min; p < 0.001) (Fig. 2).

Figure 2 ∆RHR and insulin resistance in schoolchildren aged 6 to 9 years. Student's t-test. p value represents trend between groups.
No statistical relationship was found between ΔHRR and -PF z (lower, middle or high). Instead, an association was observed if ΔHRR and strength grip/weight (r = -0.3; p < 0.01) were included, especially in 6-7 years old obese children (r = -0.6; p < 0.01). Finally, in the same group, higher ΔHRR was associated with a lower z-PF (r = - 0.6, p = 0.04).
DISCUSSION
Our study showed that overall PF-z, grip strength, HOMA and insulinemia were significantly associated with ΔHRR in overweight and obese children.
An important point to consider when interpreting the results of this study is the large variability in HR by age. This variability is due to a progressive maturation of the autonomic nervous system between three and six years old children. During this period, there is a tendency to increase sympathicotonia 23) (24) (25. Over-activation of the sympathetic nervous system in obesity, hypertension and hyperinsulinism 26) (27 could be explained by an increase in free radicals, a decrease in nitric oxide, and an increase in both tubular sodium reabsorption and arterial vasoconstriction 28). Our results showed fluctuations in heart rate at rest and after the 6MWT by sex and age range, and an association between insulin levels, HOMA and waist circumference with ΔHRR in children with overweight/obesity. Wilks et al. reported that lifestyle changes for four to six weeks in children and adolescents with overweight/obesity would produce a significant improvement in heart rate recovery, although this recovery would not be associated with an improvement in cardiometabolic risk factors 29.
We find that higher ΔHRR was associated with a lower overall physical fitness (z-PF) in obese children aged six to seven years, a difference that was not observed in other children. This could be possibly explained by the fact that this group is more susceptible to develop sympathicotonia due to the lower age range. Furthermore, the nutritional state of these children is associated with greater cardiovascular and metabolic risk 9. The association is not expressed in the same way when analyzing separately the ratio of heart rate recovery with different fitness tests. In our study, ΔHRR was associated only with better grip strength/weight. This result is consistent with the fact that a better physical fitness in children is usually associated with greater muscle strength. Artero et al. found, in a sample of 709 adolescents, that muscle strength was associated with better physical condition and lower cardiometabolic risk 30. In this regard, this finding and our work complement previous studies in which the results showed that heart rate recovery was a marker of aerobic fitness, not related with muscle strength 31. On the other hand, the lack of association with the 6MWT could be because the latter would have a low correlation with maximum oxygen consumption (VO2max), assessing functional capacity and not fitness aerobic. Morinder et al. found a low correlation between the traveled distance by the 6MWT and VO2max in 8-16 years obese children 32. Other authors obtained similar results in obese children and adolescents by comparing the correlation of 6MWT and Cooper tests with VO2max 33.
In analyzing our results related to ΔHRR, nutritional status and cardiometabolic risk, it is important to consider that 23% of subjects were obese, similar to that reported by the Board of School Aid and Scholarships Chile 34. Nearly half (48%) of our sample had CMR, close to the prevalence of insulin resistance (53%) described in Chilean children and adolescents between four and 16 years 35. In our study, children with insulin resistance had significantly higher ΔHRR, results similar to those of KuoHsu-Ko et al. in a sample of adolescents and adults with insulin resistance 36.
The differences found in ΔHRR by nutritional status were similar to those described in American obese schoolchildren 9. Another study in healthy adolescents and adults between 12 and 49 years showed that those who had slower heart rate recovery had higher BMI 36.
A lack of association was found between ΔHRR and CMR, which is consistent with other studies. In a sample of US adolescents (NHANES III), Liny el al. found, after a test of aerobic submaximal fitness, that heart rate recovery per minute was not associated with overall CMR, even if it was associated with some components of the metabolic syndrome 11. This result could be explained because the low demand of the submaximal test does not generate an increase of maximum heart rate or a change in ΔHRR, so it cannot detect individuals with higher CMR. In a sample of 1,395 children of both sexes, aged 9-12 years old, evaluated with a maximal test of short duration (three minutes), Laguna M. et al. found a significant association between blood pressure and ΔHRR in younger subjects and no association with global CMR 37.
One limitation of this study was the choice of the 6MWT. Future research should consider using the Navette test, an instrument with strong evidence to determine aerobic capacity in children and adolescents 38. Further, the lack of previous data related to the physical fitness of Chilean children could have influenced the overall classification and analysis of PF-z, and thus the absence of an association with heart rate recovery. In addition, not having measured blood pressure could partly explain the lack of association between CMR and ΔHRR, which however was associated with levels of insulin and HOMA. These findings support the need to improve efforts to reduce the high prevalence of overweight and obesity in schoolchildren aged 6-7 years. We can conclude that in overweight and obese children, ΔHRR could be a sensitive method for evaluating physical fitness and metabolic risk.














