INTRODUCTION
Body composition measurements are useful to estimate adiposity, muscle mass and fluid retention in different clinical conditions 1) (2. BIA has been widely used for this purpose after being validated by DEXA, CT and hydrodensitometry 3) (4. The accuracy and precision of the technique can be affected by several variables, one of which is the electrode system 5. It has been found that factors such as electrode size, electrode type, electrode positioning, contact impedance, and polarization voltage can influence the stability of the measurement 6. Failing to adjust for differences in electrodes may result in systematic biases in resistance of up to 5.2% 7. The search for new electrode materials and designs attempting to overcome the artifacts produced by these factors is now an area of considerable research 8) (9) (10. At the beginning, bioimpedance methods used uncomfortable needle electrodes; then, adhesive gel electrodes were used to optimize electrical contact, and more recently, electrodes evolved to modern plate, textile and simple touch-pad electrodes without the need for invasive techniques 11. However, despite extensive research, ability to determine the electrode system properties is still very limited as noticed by Geddes 6. While some bioimpedance analysis manufacturers claim for specifically suited BIA electrodes to obtain precise and reproducible results in bioimpedance testing, some users recommend standard ECG electrodes for BIA performance 12) (13. However, using suitable BIA electrodes could increase the tight budget for health, and sometimes imply difficulties in the importing process 14. For these reasons, many researchers and users have chosen to use ECG electrodes, but certainly, all ECG electrodes do not perform the same, as it was previously shown 14). While the optimal electrode system for BIA body composition continues improving, the validation of ECG electrodes for BIA is an important issue for the technique. Therefore, the aim of this study was to compare suitable previously evaluated BIA electrodes with non-evaluated ECG electrodes.
MATERIALS AND METHODS
SUBJECTS
The methods were approved by the Bioethics Committee of the Universidad de Caldas. A sample of 40 young adult females of the Universidad de Caldas (Colombia) was evaluated. The purpose and procedures of the study were explained to the volunteers and the inclusion/exclusion criteria were verified after completing a questionnaire. Then, the volunteers signed an informed written consent.
Inclusion criteria were being female aged between 18 and 24 years with BMI between 18.6 and 27.6 kg/m2 and without co-morbidities. Exclusion criteria were smoking, having a metallic or a cardiac pacemaker, being pregnant or using diuretics, and having undergone surgery for weight reduction or silicone implants in the breasts.
DATA ACQUISITION
Measurements were performed in one session early in the morning to minimize environmental and biological variations. Relative humidity and environment temperature were controlled with an electric heater (BFH416, Bionaire(r)) and a dehumidifier (BMD100, Bionaire(r)). Relative humidity (RH) and environmental temperature were measured with a thermo-hygrometer (13307, DeltaTrak(r), ± 1% RH/± 0.1 °C) and atmospheric pressure was measured with a barometer (K4, Konustar(r)). Volunteers were asked to comply with the following requirements before the test: not drinking alcohol in the previous 48 hours, 12 hours of no vigorous exercise and 12 hours of fasting but keeping normal water hydration. All were asked to evacuate their bladder and colon 30 minutes before the test and wear a hospital gown during the test. All participants were required to be in the proliferative-follicular phase or in the first seven days of the luteal phase of menstrual cycle 7.
ANTHROPOMETRIC MEASUREMENTS
Height (Heightronic-235(r), Seca, ± 0.01 cm) and weight (PP2000, Icob-Detecto(r), ± 0.1 kg) were measured twice, and a third measurement was taken if a difference greater than 0.5 cm or 0.1 kg respectively was found 15.
BIA MEASUREMENTS
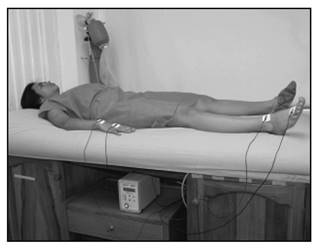
Volunteers were measured on the dominant side of the body for three times at the end of an exhalation on a nonconductive surface 16 (Hydra 4200, Xitron Technologies). Raw resistance (R), capacitive reactance (Xc) and impedance (Z) data at 5, 10, 50, 100, 200 and 500 kHz were measured according to a standardized protocol described earlier 7. Briefly, legs were separated about 45° and arms were separated from trunk about 30° 7) (16 (Fig. 1). Dorsal hand and anterior foot surfaces were cleaned with alcohol and dried with a paper towel (7). Four landmarks were made for the placement of the electrodes: the mid-line between the prominent ends of the radius and ulna of the wrist, the midline of the third metacarpal-phalangeal joint on the dorsal hand surface, the midline between the medial and lateral malleolus of the ankle and the midpoint of the third metatarsal-phalangeal joint on the anterior surface of the foot 5) (7) (14. Current was applied at the distal electrodes and the voltage was measured at the proximal electrodes (Fig. 1). BIA measurement protocol for each type of electrodes (in random order) was: five minutes standing up, measurements between minutes 6 to 10 minutes after lying down, and then five minutes standing up again before the measurement with another type of electrodes 14.
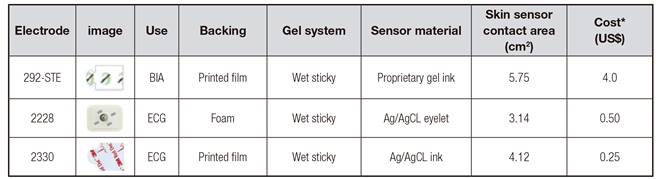
Results obtained with two types of ECG electrodes commercially available (2230 and 2228, 3M) which had not been evaluated previously were compared to the results obtained with the electrodes recommended by the bioimpedance meter manufacturer (292-STE, Impedimed(r)) because this type of electrodes is specifically designed to fit the device. For this reason, in this study, the results obtained with 292-STE electrodes were used as the reference measurements. Table I shows some characteristics of the three different types of electrodes tested in this study.
STATISTICAL METHODS
The Hydra_S_Acquisition Utility (version 1.0 2003) was used to capture the raw data and the Hydra_Data_Model_Vol Utility (version 2.2 1997) was used to obtain the model data and volumes. Mean and standard deviation (SD) were used to evaluate the characteristics of subjects and laboratory conditions. Low and high frequencies were represented from 5 to 500 kHz respectively. Raw data (R, Xc and Z) from 5 to 500 kHz were analyzed to determine the effect of exchanging the order of using the reference electrodes. Raw data, model data (extra-cellular-fluid resistance RECF, intra-cellular-fluid resistance RICF), and volume data (extra-cellular-fluid volume ECF and intra-cellular-fluid volume ICF) were analyzed to determine significant differences between electrodes. Bland Altman plots and paired Student's t-test, using p < 0.01 as significant, were used for statistical comparisons of the various parameters obtained from the bioimpedance machine (Bland and Altman 1986). The standard error of estimate (SEE) was used to evaluate if body composition data was acceptable. The SEE for ECW and ICW was acceptable if it was between 1.0 l and 1.5 l 17. All analyses were performed using XLSTAT software (version 2013.1.01, Addinsoft).
RESULTS
Environmental conditions during measurements were stable: temperature was 18.8 ± 0.7 °C, relative humidity was 73.5 ± 1.9% and atmospheric pressure was 787.4 ± 0.6 mmHg. Subjects' characteristics are shown in Table II.
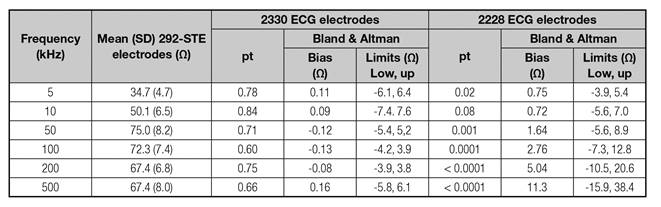
Comparison of raw data (R, Xc and Z from 5 to 500 kHz) obtained in 40 subjects using ECG electrodes (2330 and 2228) versus the reference electrodes (292-STE) are shown in Table III, Table IV, Table V.
Table III Resistance comparison between ECG and BIA electrodes (n = 40)
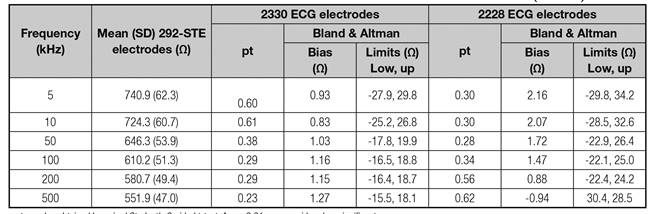
pt: p-value obtained by paired Student's 2-sided t-test. A p < 0.01 was considered as significant.
Table IV Reactance comparison between ECG and BIA electrodes (n = 40)
pt: p-value obtained by paired Student's 2-sided t-test. A p < 0.01 was considered as significant.
Table V Impedance comparison between ECG and BIA electrodes (n = 40)

pt: p-value obtained by paired Student's 2-sided t-test. A p < 0.01 was considered as significant.
Comparison of data volume (ECF, ICF) in 40 subjects using ECG electrodes (2330 and 2228) versus reference electrodes (292-STE) showed that the differences for ECF results between the two types of electrodes tested (3M-2330 and 3M-2228) were small and non-significant (-0.01 and -0.05 liters respectively when compared to the 292-STE electrodes). Similar results occurred with ICF estimations; however, in this case the differences were higher than for ECF: -0.06 and 0.20 liters respectively.
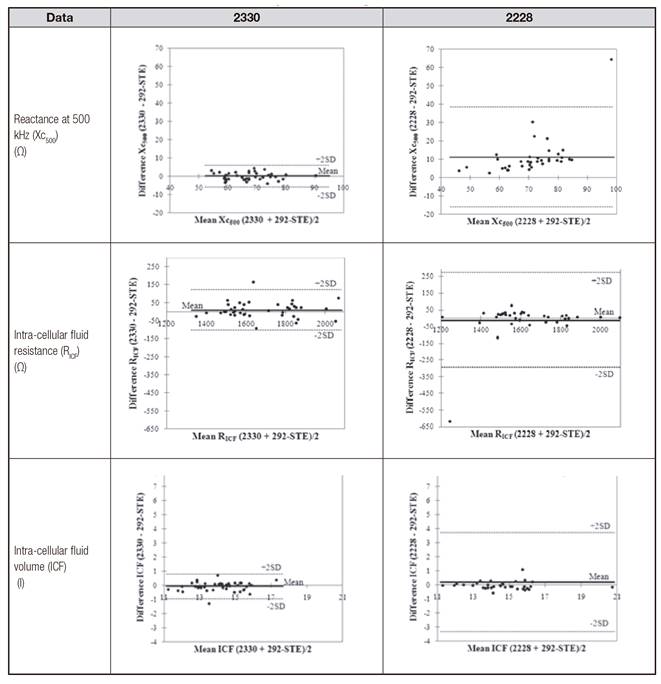
Bland and Altman plots for some raw, model and volume data from 40 subjects using ECG electrodes (2330 and 2228) versus the reference electrodes are presented in Table VI to show the biggest discrepancies at high frequency measurements. Simple linear regressions of data volume by 292-STE versus ECG electrodes are shown in Table VII.
DISCUSSION
There is a constant commitment to improve the quality of BIA measurements and try to minimize the most of all the variables that affect the results and remove the BIA merits. It has been recognized that the type of electrodes for electrical measurements influence the signals that are measured and it is important to find the suitable electrode system for each application, otherwise, the obtained data might produce wrong estimation of BIA parameters and inaccurate diagnosis of body composition 19. Although the bioimpedance analysis manufacturers have strongly recommended using the electrodes designed for a specific BIA machine, this is not always possible and many researchers use the ECG electrodes. However, some electrodes do not have the minimum recommended area or gel cannot meet the requirements for long-term use in hemodialysis and renal applications 20. Since in many cases studies report using ECG electrodes in bioimpedance measurements, we wanted to compare previously evaluated and not evaluated ECG electrodes from the same brand trying to find those producing the fewest artifacts.
In this study, 40 healthy women normally-hydrated and without clinical skin affections were measured in the frequency range 5 to 500 kHz. Although the device generates data at 1,000 kHz, these measurements were omitted since it is known that at higher frequencies, the stray capacitance can produce errors 21. Three types of electrodes were tested: those for reference which are produced for the specific BIA device (Impedimed(r) 292-STE) used for this study, evaluated ECG electrodes (3M-2228) and non-evaluated ECG electrodes (3M- 2330).
The 3M-2228 and 3M-2330 did not show statistically significant differences with the reference standard electrodes in resistance. However, the 3M-2228 reactance differed significantly from the 50 kHz measurements. When impedance was examined, the differences were not significant for the two types of electrodes (probably because the resistive component is greater than the reactive) but the different reactive component was reflected in the modeling and estimating of the intra-cellular fluid volume. The results showed that albeit the already evaluated ECG electrodes (3M-2228) performed well and within the previously established parameters, the non-evaluated 3M-2330 performed better. Thus, by using the correct ECG electrodes some limitations produced by these electrodes must be previously predicted and prevented to undertake BIA measurements.
Possible explanations for the results may be related to the greater area of the 3M-2330 compared to 3M-2228 electrodes (Table I) since the minimum recommended area is 4 cm2 (5 and because a smaller area affects the reactive component, increases the impedance 22 and deteriorates the coupling of the gel-electrode and skin interface. Another source of variation could be the backing electrodes (printed vs foam) and material sensor (eyelet vs ink). In addition, although a formal study for cost-effectiveness was not the intention in this study, we found that 2330 was cheaper than the other two types of electrodes.
Regarding the clinical significance of the findings in ECF and ICF estimations, in adults, perhaps the differences are not of clinical importance but using this ECG of the assessment of children may be more important and further studies might be done 23.
Several controversies remain on using different type of electrodes: dry or wet electrodes (and type of gel for the latter), metal touch or textile electrodes 8) (11) (24. Although dried gel electrodes would have more advantages over wet gel electrodes, dried gel electrodes are less conductive than wet gel electrodes. The gel is able to get into the skin ensuring better interface gel-electrode-skin. For this reason, wet electrodes are the most commercial ones 25. Previously, it was found that 3M-2228 wet-gel electrodes are more convenient for BIA measurements than the 2290 dried-gel electrodes.
Recently, conductive textile materials have been used for electrodes. However, to date, the results obtained with these materials have low reproducibility and cause errors in the estimation of the body composition, and more research must be done to provide a textile-based electrode system to allow reliable BIA measurements 8) (9. In addition, these types of electrodes are not easily available in developing countries. While both situations changed, we tried to find which ECG electrodes would be more suitable for BIA measurements.
CONCLUSION
The findings in this report suggest the possibility of measuring BIA parameters with ECG electrode system in young adult females when the recommended manufacturers of BIA devices are not available. Since not all ECG electrodes are suitable for these measurements, ECG electrodes should be evaluated for BIA measurements in order to avoid adding errors to the registered signals and making mistakes in assessing body composition in humans.