INTRODUCTION
Vitamin D deficiency leads to alterations in calcium and phosphorus homeostasis, resulting in secondary hyperparathyroidism with increased bone turnover, progressive bone loss, and increased risk of fractures 1,2. Numerous studies have demonstrated lower serum total 25-hydroxyvitamin D (25[OH]D) concentrations in obese subjects compared with their non-obese counterparts 3 4 5 6 7 8 9-10. Although the precise mechanism of decreased 25(OH)D levels in obesity has not been fully elucidated, research findings suggest that increased metabolic clearance and enhanced uptake of vitamin D by adipose tissue or decreased bioavailability of vitamin D once it is deposited in fat tissue may account for this finding 3,4. Moreover, Drincic et al. recently described that simple volumetric dilution may be the most parsimonious explanation for the low vitamin D status in obesity 5.
Aging is characterized by a reduction of muscle, bone mass, and strength levels with a concomitant increase of body fat mass, especially visceral fat mass 11. Moreover, older adults are particularly at higher risk of 25(OH)D deficiency because sunlight exposure is usually limited as a result of lifestyle changes. Likewise, the total production of previtamin D3 after exposure to solar ultraviolet B radiation also decreases considerably with aging 12,13. In Ecuador, despite abundant sunlight throughout the year, a recent study among older adults reported a high prevalence of 25(OH)D insufficiency predominantly in women, indigenous, and residents in the Andes Mountains region of the country. In addition, subjects defined as having obesity had lower 25(OH)D concentrations compared with their non-obese counterparts 14. Because obesity is potentially a modifiable risk factor of 25(OH)D insufficiency, the present study aimed to extend previous research findings by examining the association between obesity and 25(OH)D status in a nationally representative sample of older adults in Ecuador.
METHODS
The present study was based on data from the National Survey of Health, Wellbeing, and Aging (Encuesta National de Salud, Bienestar, y Envejecimiento; SABE II). Briefly, this survey is a probability sample of households with a least one person aged 60 years or older residing in the Andes Mountains and coastal regions of Ecuador. The SABE survey complex sampling design has been described elsewhere 15. Between April and August 2010, participants had biochemical evaluation to determine their nutritional status, including 25(OH)D concentrations. The survey data, including operation manuals, are publicly available and can be downloaded from the SABE survey website 16.
CHARACTERISTICS OF SUBJECTS
Age, sex, and race (white, black, mestizo, mulatto, or indigenous) were self-reported. Subjects were asked about their region (coastal vs mountains) and area of residence (urban vs rural). Literacy was defined by answering affirmatively to the question "Can you write and read a message". Smoking status was classified as current, former and never, and physical activity was evaluated by the question "Do you exercise regularly such as jogging and dancing, or have you performed rigorous work at least three times weekly for the past year?" Participants who responded affirmatively were considered to engage in vigorous physical activity. Self-reported general health was grouped as excellent to good or fair to poor.
Body height in centimeters and weight in kilograms were measured and the body mass index (BMI) was calculated (kg/cm2). BMI was classified into three categories: under/normal (< 25 kg/m2), overweight (25-29.9 kg/m2), and obese (≥ 30 kg/m2)17.
Subjects were defined as having diabetes according to the American Diabetes Association 2017 criteria if they reported a physician diagnosis of diabetes or had a fasting plasma glucose ≥ 126 mg/dl 18. Serum 25(OH)D was measured by liquid chromatography at NetLab laboratory (Quito, Ecuador). The lowest limit of detection for the serum 25(OH)D assay was 4 ng/ml. A serum 25(OH)D < 20 ng/ml was the cut-off level to define subjects with 25(OH)D insufficiency as recommended by the Institute of Medicine 19.
STATISTICAL ANALYSIS
The descriptive characteristics of participants were stratified by BMI categories and examined using the ANOVA and Chi-square test for continuous and categorical variables, respectively. Data for men and women were analyzed separately since the prevalence of 25(OH)D insufficiency and obesity differed by gender among older adults in Ecuador 14,20. Subsequently, sex-specific multivariate logistic regression models were assembled in stages to evaluate the independent associations between BMI categories and the prevalence of 25(OH)D insufficiency. The first model was adjusted for age, race, and area of residency. A second model was further adjusted for literacy, smoking status, physical activity, self-reported health, and diagnosis of diabetes. Of 2,375 participants who completed the biochemical evaluation, 105 subjects were excluded from this analysis because of missing data on 25(OH)D concentrations (n = 5) and BMI (n = 100) measurements. All analyses used sample weights to account for nonresponse and the unequal probability of selection of the SABE survey and thus provide estimates representative of the older adult population in Ecuador. Statistical analyses were performed using SPSS, version 17 software (SPSS Inc., Chicago, IL).
RESULTS
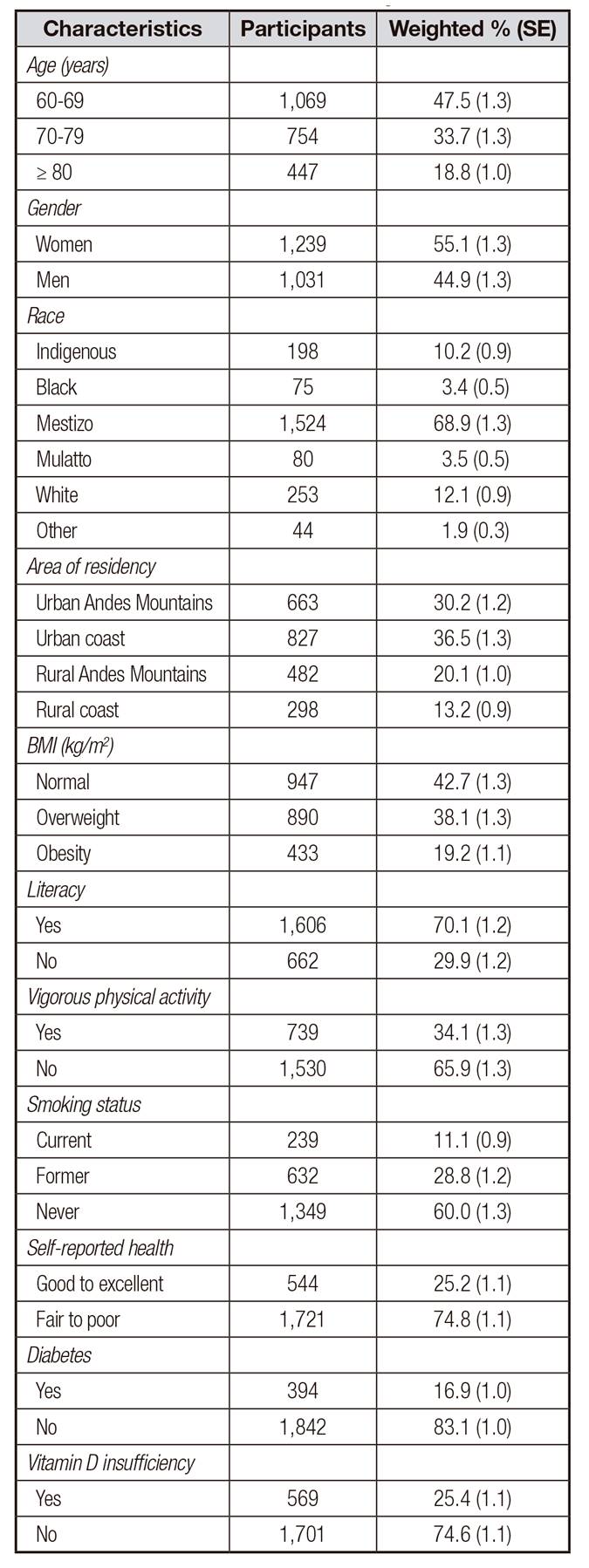
A total of 2,270 participants with a mean age of 71.5 (SD 8.1) years comprised the sample size, representing an estimated 1.1 million older adults in Ecuador. Table 1 shows the demographic, behavioral, and health characteristics of participants. In general, women and self-reported race as mestizo accounted for 55.1% and 68.9% of the participants, respectively. In addition, the crude prevalence of obesity was 19.2% and 25.4% of subjects were defined as having 25(OH)D insufficiency.
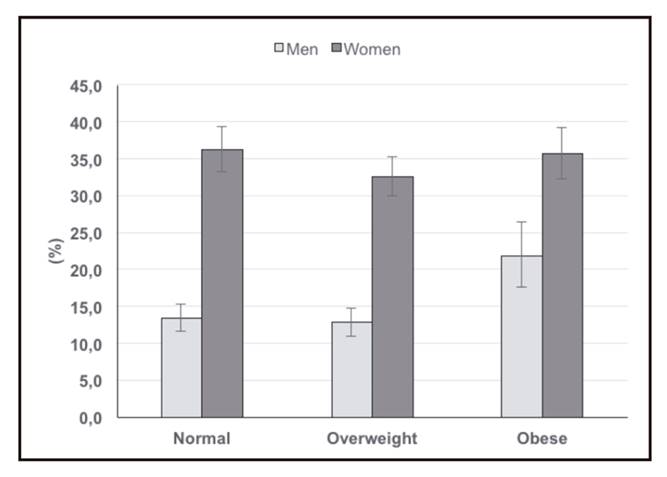
Table 2 shows the characteristics of participants stratified according to BMI categories. Overall, women, residents in the urban Andes Mountains, and subjects defined as having diabetes had higher obesity prevalence rates than those without. Moreover, obese subjects had significantly lower 25(OH)D concentrations compared with their non-obese counterparts. Likewise, obesity prevalence rates were higher among older adults with 25(OH)D insufficiency than in those without. As shown in Figure 1, the prevalence of 25(OH)D insufficiency was considerably higher in women and remained steady across BMI categories. In contrast, 25(OH)D insufficiency prevalence rates in men increased progressively as BMI categories also increase.
As shown in Table 3, obese older men were two times more likely to have 25(OH)D insufficiency compared with those defined as having an ideal weight. Moreover, this strong association persisted even after adjusting for sociodemographic, behavioral, and health characteristics of the participants. In women, obesity was weakly associated with an inadequate 25(OH)D status. However, the prevalence of 25(OH)D insufficiency remained 12% higher in obese women compared with their normal weight counterparts.
DISCUSSION
The present findings indicate that obese older Ecuadorians had higher 25(OH)D insufficiency prevalence rates than their normal weight counterparts. This relationship was particularly evident in men. Indeed, older men with obesity had two-fold higher odds of having 25(OH)D insufficiency compared with those classified having a normal weight even after adjusting for sociodemographic characteristics previously associated with a high prevalence of 25(OH)D insufficiency nationwide 14. In contrast, obese women were not significantly associated with inadequate 25(OH)D status, which may have been be partly explained by a high prevalence of 25(OH)D insufficiency across BMI categories, but particularly among those defined as having a normal weight. Indeed, up to 36.3% of women with normal weight had evidence of 25(OH)D insufficiency in Ecuador. Similarly, overweight men and women had 11% and 13% lower risk of having 25(OH)D insufficiency than those with an ideal weight, respectively. Of relevance, a recent study described significantly higher obesity prevalence rates nationwide in women than in men 20. Thus, it is possible that the increased prevalence of 25(OH)D insufficiency in older women may be related to gender differences in body fatness, which has been documented by other investigators 21,22.
The present study results are consistent with those from the Mexican Health and Aging Study in which obese older adults were 1.7 times more likely to be associated with 25(OH)D concentrations in the lowest tertile (≤ 20.4 ng/ml) compared with their normal weight counterparts 22. Similarly, results of the Health, Aging and Body Composition Study demonstrated that older obese black and white were 1.5 and 1.3 times more likely to be defined as having 25(OH)D insufficiency, respectively 23. A previous study among participants of the Longitudinal Aging Study Amsterdam also reported that higher BMI, waist circumference, and skin folds were statistically significantly associated with lower 25(OH)D concentrations. However, the associations of total body fat with serum 25(OH)D levels were stronger than the associations of anthropometric measures 23. Furthermore, Young et al. demonstrated that among Hispanic and African-American, 25(OH)D levels were inversely associated with baseline BMI, and computed tomography derived measures of subcutaneous and visceral adipose tissue 25.
Notably, a recent study conducted to examine the effect of BMI categories on 25(OH)D concentrations and bone health demonstrated low free 25(OH)D levels in obesity, which were not due to differences in protein binding. Indeed, serum albumin and vitamin D binding proteins and genotype variation did not differ by BMI categories. Moreover, that particular study provided evidence that lower 25(OH)D concentrations in obesity were not due to more rapid metabolic clearance 9. Although 25(OH)D is fat soluble, and distributed into fat, muscle, liver, and serum, all of these compartments are increased in volume in obesity. Consequently, lower 25(OH)D concentrations likely reflect a volumetric dilution effect, and whole body stores of 25(OH)D may be adequate 26. In a recent study, Carelli et al. reported that 25(OH)D concentrations measured by mass spectroscopy in omental and subcutaneous adipose tissue did not significantly differ in obese and normal weigh women. However, total body vitamin D stores were significantly greater in obese women than in their normal weight counterparts. Thus, these findings also support the hypotheses that the enlarged adipose mass in obese individuals serves as a reservoir for vitamin D and that the increased amount of vitamin D required to saturate this depot may predispose obese individuals to inadequate serum 25(OH)D 27. Of relevance, a large study conducted among healthy volunteers in the province of Alberta, Canada, demonstrated that the differences in serum 25(OH)D between normal, overweight, and obese subjects significantly differed by supplementation dose. For instance, supplementation with 600 IU per day would achieve a mean serum 25(OH)D levels of 33.2, 30.4, and 26.4 ng/ml in normal weight, overweight, and obese participants, respectively. Moreover, a mean serum 25(OH)D concentration of 40 ng/ml in normal, overweight, and obese subjects, was estimated to require 2,080 IU, 3,065 IU, and 5,473 IU per day, respectively 28. However, as previously described, overweight and obese subjects were less likely to use any dietary or vitamin supplements compared with their normal weight counterparts 29. Therefore, it is possible that the increased prevalence of 25(OH)D insufficiency among obese Ecuadorians may be partly explained by the low use of vitamin D supplements. However, this hypothesis may not be confirmed because no previous study has reported the prevalence of vitamin D supplement use among older adults in Ecuador. Of interest, results of a recent systematic review of randomized and nonrandomized control weight-loss trials reported that the effect of weight loss on circulating 25(OH)D levels, random assignment to weight loss compared with weight maintenance resulted in a small but significantly greater increase in serum 25(OH)D of 0.44 ng/ml. Similar results were found for nonrandomized trials 30. Thus, based on these findings, older obese subjects should be offered vitamin D supplementation and lifestyle modifications to improve their 25(OH)D status.
Several limitations should be mentioned while interpreting the present study results. First, the temporal relationship between obesity and 25(OH)D status may not be established due to the cross-sectional study design. Second, participants self-reported their demographic and certain behavioral characteristics, which may be a source of recall bias. Third, the dietary intake of and use of vitamin D supplements was not assessed in the survey. Fourth, participant's sunlight exposure was not examined. Fifth, because traditional anthropometric measures of adiposity such as BMI are weaker than direct measures of adiposity, it is possible that the association between obesity and 25(OH)D may be underestimated in the present study 25. Finally, the present study findings may be generalized to older adults residing in the coastal and Andes Mountains regions of the country.
In conclusion, obesity is associated with increased risk of 25(OH)D insufficiency among older adults in Ecuador. Thus, obese older subjects should be offered vitamin D supplementation and counseled regarding lifestyle modifications to improve their 25(OH)D status.