INTRODUCTION
Vitamin D is classically known for its role in regulating body levels of calcium and phosphorus 1,2. In recent years there has been a high level of vitamin status for a substition with hormone characteristics, making it clear that the exercise is biological effects that regulate osseous metabolism 3,4. Despite its physiological multifunctionality, it is believed that the active form of vitamin D exerts its main effects interacting with the high affinity receptor of this vitamin, called a vitamin D receptor (VDR), a factor of transcription-dependent transcription regulator and cell function in various tissues, which may justify its role in various physiological functions of the organism including glucose metabolism, immune system, cancer and cardiovascular diseases 2.
Evidence shows a high prevalence of insufficient vitamin D levels worldwide, which is considered as a public health problem 2,3,4,5. The deficiency of 25-hydrovitamin D (25 [OH] D) is often found in adults and the elderly 5,6. However, recent studies have shown that adolescents and young adults also present insufficient levels of this vitamin in several parts of the world 2,3,4,5,6,7. In countries with greater sun exposure such as Brazil, some studies have found an insufficiency of 70% and 60% in the cities of Juiz de Fora and São Paulo, respectively 8,9.
In the adult population, findings suggest an association between serum levels of 25 (OH) D and the risk of developing diabetes mellitus, cardiovascular disease, cancer 2,3,4,5,6,7,8,9,10, increased blood pressure 11, increased oxidative stress, chronic inflammation 12,13 and obesity 7,8,9,10,11,12,13,14. Another role of vitamin D that has been studied is its action on immunity with possible action in T cells, acting as a significant protector against oxidative stress and antioxidant and anti-inflammatory action 15,16. However, studies evaluating the associations between 25 (OH) D serum levels and biomarkers of inflammation and oxidative stress at school age are rare.
Current data demonstrate that even without outcomes such as the development of type II diabetes and cardiovascular disease, adolescents with insufficient levels of vitamin D are associated with increased risk factors for these complications, including higher BMI, increased blood pressure, insulin resistance and increased oxidative stress 17,18. However, the relationship between 25 (OH) D insufficiency and the increase in cardiometabolic risk factors in childhood and adolescence is still little explored in the literature.
In this sense, this study was designed to verify the presence of vitamin D insufficiency/deficiency results in cardiometabolic disorders in a population of adolescents.
MATERIALS AND METHODS
STUDY DESIGN, POPULATION AND SAMPLE
A cross-sectional epidemiological study was carried out between June and August 2015 involving adolescents between 15 and 19 years of age enrolled in public schools in João Pessoa-PB, a metropolitan city in the northeastern region of Brazil.
To define the sample size, the OpenEpi program (www.openepi.com) was used, considering the prevalence of 60% of hypovitaminosis D found by Peters et al., with a 10% margin of error and a significance level of 5%. The design effect was corrected by multiplying by a factor of 2.1, making a minimum total of 194 adolescents and a margin around 10% for eventual losses. Thus, 229 adolescents were recruited in total. However, nine participants did not meet the inclusion criteria or did not complete all stages of the study, therefore totaling a final sample of 220 individuals.
Stratified sampling was performed with a minimum of 10% of the 32 public schools in the city of João Pessoa, totaling four institutions distributed in distinct regions to ensure greater randomness of the sample. After the classes were surveyed, three rooms were drawn from each school, in which all the adolescents in the age group of interest were invited to participate. Thus, 12 rooms were part of the study.
Adolescents of both genders aged 15 to 19 years were included in the sample and adolescents who already had experienced menarche or presented hair by the axillary and facial region (according to gender). Exclusion criteria were adolescents who were pregnant, breastfed, used supplements or medications that contained or interfered with vitamin D metabolism, carriers of chronic diseases (diabetes, hypertension, chronic kidney disease) or chronic alcoholics or smokers. In addition, renal and hepatic functions were evaluated by means of specific laboratory tests (urea, creatinine, uric acid, alanine amino transferase and aspartate amino transferase) to identify possible abnormalities.
The study protocol was previously approved by the Ethics and Research Committee of the Health Sciences Center of the Federal University of Paraíba (CCS/UFPB) in compliance with Resolution 466/12 of the National Health Council (CAE 43097115.2.0000.5188).
DATA COLLECTION
Data on gender, age and date of birth, marital status, sociodemographic issues and anthropometric data were collected. Data from dietary intake and sun exposure were collected and demonstrated in the previous study 19.
Sociodemographic information, history and clinical and dietetic evaluation
Sociodemographic data were collected through a semi-structured questionnaire. Data collected included gender and age. Clinical history was analyzed through family and personal pathological antecedents, medication use and vitamin supplements. Boys were considered to be sexually mature with presence
of hair by the axillaries, as well as girls who had already experienced menarche 20.
Diastolic and systolic blood pressures were measured using the right arm at the same level of the heart using an adequate armband. The measurement was performed in duplicate for each adolescent within an interval of five minutes. We used the auscultatory technique with an adequately calibrated aneroid sphygmomanometer. The classification took into account gender, age and height based on the parameters of the Brazilian Society of Hypertension 21.
ANTHROPOMETRIC ASSESSMENT
Weight was evaluated with a digital scale (model BAL-20 PM) with capacity for 150 kg and interval of 100 g. Height was determined with a precision of 1 mm and accuracy of 0.5 cm using a stadiometer (Sanny(r), Caprice ES2060). Nutritional status was determined by BMI according to the World Health Organization (WHO) 22). Overweight (being overweight or obese) was defined as BMI above 1 standard deviation.
Waist circumference (WC) measurements were performed with the individual standing, with the aid of a non-elastic tape measure at the midpoint between the last rib and the iliac crest. For risk classification by WC, a percentile > 80 was used as risk for metabolic diseases according to Taylor et al. 23. Waist-to-height ratio (WHtR) was obtained by the quotient between waist circumference (cm) and height (cm). The single cut-off point adopted was 0.5 24.
DIETARY INTAKE
Vitamin D intake was evaluated by applying a 24-hour recall with all participants, and a new application was performed in 40% of the sample on a non-consecutive day, respecting a minimum period of 30 days and a maximum of 45 days between the application of one reminder and another. Vitamin D intake was calculated using Avanutri Revolution software version 3.0.
The multiple source method (MSM) available at the site (https://msm.dife.de/tps/msm/) was used to estimate the distribution of habitual intake. The mean intake was compared according to age group with that proposed by the dietary reference intake (DRI) according to estimated mean need (EAR). Thus, the daily vitamin D recommendation of 10 μg/day was used 25.
BIOCHEMICAL ANALYSIS
The adolescents were informed about the need to fast for 12 hours and the blood samples were collected at school on pre-scheduled dates, with approximately 15 ml being withdrawn by venipuncture. Blood samples were collected by a suitably trained team for analysis of 25 (OH) D, parathyroid hormone (PTH), hs-CRP, AGP-A, MDA, CAT, calcium, urea, creatinine, ALT and AST. The samples were centrifuged at 3,000 rpm for 15 minutes
and the supernatant was then transferred to microtubes and frozen at -20 °C until analysis.
Serum dosage of 25 (OH) D and PTH was determined by means of a chemiluminescent immunoassay (UniCel(r) DxI 800 - Beckman Coulter), considering the reference values < 20 ng/ml as deficiency, 21-29 ng/ml as failure, and ≥ 30 ng/ml as sufficient according to the Endocrine Society 14. The calcium dosage was performed by automated colorimetric technique using commercial kits from Calcio Arzenazo (Bioclin).
The dosages of glucose, total cholesterol, HDL and triglycerides were carried out in serum samples using commercial kits (Labtest, Minas Gerais, Brazil) following the manufacturer's recommendations in a Labmax 240 Premium(r) automatic analyzer (Lagoa Santa - MG, Brazil). Low-density lipoproteins (LDL-c) were obtained by the Friedwald equation (LDL-c = [CT-HDL-c] - [TG/5]) 26.
Ultrasensitive C-reactive protein (hs-CRP) and alpha 1 acid glycoprotein (AGP-A) serum levels were assessed by the immunonephelometric method. Oxidative activity was determined by an analysis of malondialdehyde (MDA) in the plasma through a thiobarbituric acid (TBARS) reaction with the decomposition products of hydroperoxides, as described by Ohkawa, Ohishi and Yagi 27. Total antioxidant capacity (TAC) was analyzed by the DPPH method in plasma, as described by Brand-Williams, Cuvelier and Berset 28.
STATISTICAL ANALYSIS
The results are presented as percentage, mean and standard deviation of the mean. The analyses were carried out in the program Statistical Package for the Social Sciences (SPSS Inc., Chicago, Ill., USA), version 21.0. The data were previously tested for normality and homogeneity by the Kolmogorov-Smirnov test and for homogeneity by Levene, respectively. The Chi-square test was used to evaluate the proportion between the nominal data groups. Pearson or Spearman correlation tests were also used for the variables studied with the serum vitamin D concentration. Multiple linear regression was also performed in order to evaluate the independent associations in multivariate form and possible confounding factors. The inclusion criterion for inputting the variables of the regression model was to present a p value of ≤ 0.20 in the correlation using the backward method, and considering the model that resulted in the smallest residue and F value. The significant threshold was set at p < 0.05 in all cases.
RESULTS
The sample consisted of 220 adolescents with a mean age of 16.9 (± 1.07) years. Vitamin D deficiency/deficiency was found in 57.3% (126) of the adolescents, with a higher prevalence in females (79.3% versus 20.6%) and also a high prevalence of overweight/obese adolescents (78%) (Table 1). With regard to dietary vitamin D intake, the usual dietary intake was 1.50 μg/day (± 0.45), representing only 15% of the recommendation of the DRIS. In addition, no individual reached the minimum recommended intake (EAR) for this age group (data not shown).
Table I General characteristics and prevalence of risk factors according to status of 25 (OH) D in adolescents
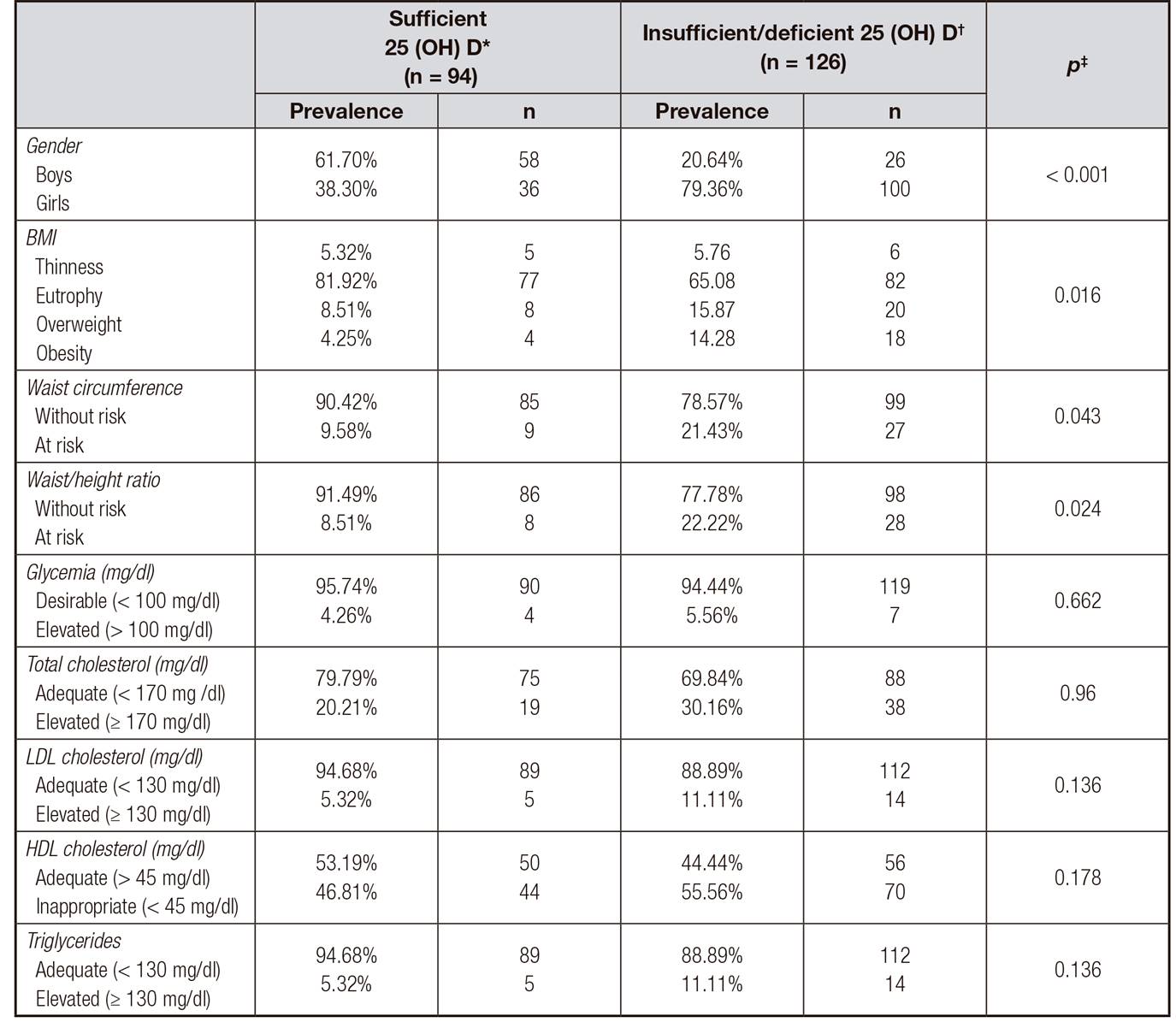
Data are expressed as mean and standard deviation of the mean (SD). 25 (OH) D: 25 hydroxyvitamin D; TG: triglycerides; COL: total cholesterol; HDL: high density lipoprotein; LDL: low density lipoprotein; CRP-us: C-reactive protein; AGPA: alpha 1 acid glycoprotein; MDA: malondialdehyde; CAT: total antioxidant capacity; SBP: systolic blood pressure; DBP: diastolic blood pressure. *25 (OH) D ≥ 75 nmol/l (30 ng/ml). †25 (OH) D < 75 nmol/l (30 ng/ml). ‡Pearson's Chi-square test or the nonparametric correspondent.
The Chi-square test revealed an evident relationship between the three overweight indicators evaluated in this study (BMI), waist circumference (WC) and waist-to-hip ratio (WHR) and vitamin D deficiency/deficiency (p < 0.05). There was no association with adequacy and/or inadequacy of the glycolipid profile and inflammation and oxidative stress when compared with the groups with sufficient or insufficient/deficient concentrations in 25 (OH) D, as can be observed in table 1.
Table II Correlation between 25 (OH) D levels and metabolic parameters

Data are expressed as mean and standard deviation of the mean (SD). 25 (OH) D: 25 hydroxyvitamin D; PTH: parathyroid hormone; TG: triglycerides; COL: total cholesterol; HDL: high density lipoprotein; LDL: low density lipoprotein; PCR-us: C-reactive protein-ultra-sensitive; AGPA: alpha 1 acid glycoprotein; MDA: malondialdehyde; CAT: total antioxidant capacity; SBP: systolic blood pressure; DBP: diastolic blood pressure.
The correlation tests indicated a positive correlation of the 25 (OH) D serum concentration with calcium (r = 0.287; p ≤ 0,01), and an inverse correlation with total cholesterol (r = -0.191, p = 0.004), LDL cholesterol (p < 0.01) and BMI (r = -0.182, p = 0.007), as observed in table 2. The variables PTH, fasting glycemia, triglycerides, AGP-A, TAC, SBP and WHtR resulted in p < 0.20, thus they were also considered for the regression model. Multiple regression analysis (Table 3) resulted in a p value. For this model, the triglyceride (p = 0.03) and calcium (p = 0.01) variables were the only variables that maintained the association with the 25 (OH) D serum concentration. This model contributed 23.6% of the variation in vitamin D serum levels.
DISCUSSION
Our study identified that even in the adolescence stage, vitamin D insufficiency/deficiency was mostly present in females, but the 20% found in boys should not be neglected, since it is already considered to be an important prevalence 14, mainly considering adolescents living in a tropical country and in a region with solar incidence throughout the year. In addition, 25 (OH) D serum concentrations had a positive association with calcium and inverse association with cardiometabolic markers, especially triglycerides, which was independently associated with gender.
Previous studies have already demonstrated the high prevalence of vitamin D insufficiency in the adolescent population. In Europe, insufficient levels of 25 vitamin D may reach 72.9% 29. The prevalence of hypovitaminosis D has been found even in tropical countries such as Brazil, where Oliveira et al. 8 evaluated schoolchildren in the city of Juiz de Fora-MG and found a 70.6% deficiency, and Peters et al. 9, in their study in the city of São Paulo with 136 adolescents, found a 60% vitamin D insufficiency.
The present study showed a higher prevalence of 25 (OH) D insufficiency/deficiency among overweight adolescents and a higher frequency of eutrophic levels with adequate levels of 25 (OH) D, demonstrating the importance of adequate nutritional status for vitamin D blood levels. This finding corroborates the study by Turer et al. 30 performed with 12,292 thousand children and adolescents, where they identified that as the BMI increased, the prevalence of vitamin D insufficiency was also increased, obtaining a deficiency between healthy weight, overweight, obesity and severely obese children of 21%, 29%, 34%, and 49%, respectively, and demonstrating that seriously obese could have twice as much chance of developing vitamin D insufficiency.
Other researchers have found this association of vitamin D with adiposity. Zhang et al. 17 studied 1,488 children aged seven to eleven years in China and identified that the vitamin D deficient group had significantly higher body weight, concluding that 25 (OH) D levels are closely associated with adiposity; and Pacifico et al. 31 identified an inverse correlation of BMI with vitamin D in 452 children and adolescents.
Evidence from other studies suggests that the possible causes of the relationship between vitamin D levels and adiposity may explain this phenomenon 32, indicating that increased adipocyte sequestration of vitamin D reduces its bioavailability. Alternatively, other authors indicate that vitamin D deficiency leads to increased parathyroid hormone, which may promote the influx of calcium into adipocytes and thus stimulate lipogenesis 33. Regardless of the causative factor, vitamin D deficiency and being overweight appear to be detrimental in this age group, requiring additional research to clarify and direct the relationship between vitamin D and obesity.
Vitamin D is considered to be a pre-hormone and, together with the parathyroid hormone (PTH), they act as important regulators of calcium homeostasis and bone metabolism, with these actions being well-established in the literature 2. Pludowski et al. 10 conducted a review based on randomized meta-analyzes and reported that vitamin D deficiency in children and adults causes a decrease in the efficiency of intestinal calcium absorption, and may result in a significant decrease in bone mass and exacerbate osteopenia and osteoporosis in children. At present, a positive correlation was found between calcium and vitamin D levels; this is extremely important since, given the evidence that vitamin D has a known role in bone health, its deficiency can cause bone health damage in childhood.
On the one hand, if the ratio of calcium to vitamin D is notorious, our study found an inverse correlation with triglycerides. In a study of 452 children and adolescents, an inverse association of 25 (OH) D with blood pressure, triglycerides and obesity was found, but the association with hypertriglyceridemia became non-significant after adjustment with BMI. The explanation for the inverse associations of metabolic disorders with vitamin D deficiency is very complex and the results with the association of vitamin D with the lipid profile are still conflicting and limited. A possible mechanism by which vitamin D may be associated with triglyceride levels is through increased lipoprotein lipase activity, which has been shown to be regulated by vitamin D in adipocytes 34.
Recently, extra-osseous vitamin D functions have been investigated and one of the most evident results demonstrates a relationship with cardiometabolic risks 2. It is concerning that current research demonstrates these risk factors are also present in adolescents with vitamin D insufficiency, particularly with high levels of blood glucose, blood pressure, total cholesterol, inflammatory markers and oxidative stress 8,9,10,11,12,13,14,15,16,17.
Vitamin D insufficiency/deficiency has also been the cause of inflammation and oxidative stress. This malady has already been described in adolescents, but the results are still controversial. A study carried out in Spain with obese children aged seven to 14 years found levels of vitamin D deficiency (< 20 ng/ml) in 5% of the normal children in the control group and in 30% of the obese children, in which there was an increase in oxidative stress and inflammation markers. The oxidative stress, malondialdehyde, myeloperoxidase, and 3-nitrotyrosine markers together with interleukin 6 levels were significantly increased in the 25 (OH) D group, presenting values of < 20 ng/ml (deficiency), but found no significant difference in the inflammation markers for C-reactive protein (CRP) 35.
It is important to note that this association was found in the obese population, which is a factor that causes an increase in inflammatory markers and oxidative stress. Another study by Zhang et al. 17 with children between seven and eleven years old found that the insufficient ones presented higher levels of inflammatory markers (CRP and interleukin-6) in comparison to the sufficient children, but the statistical significance disappeared after adjusting for BMI, which is caused by adiposity.
In the present study no association between 25 (OH) D serum concentrations, inflammatory process parameters (CRP, AGP-A) and oxidative stress (MDA and TAC) was found. This is the first study in adolescents to date to demonstrate this trend with AGP-A, stimulating future studies using this marker in the adolescent age.
The practical implications of the present study lie in the prevalence aspect and the harmful effects found. Regarding prevalence, this study confirms previous data of high prevalence. We verified that there is a deficient consumption of vitamin D sources, so that the main practical implication is that society should be paying greater attention to food intake of vitamin D sources in adolescents and to evaluate introducing vitamin D enriched food policies. From the perspective of the observed cardiometabolic effects, this study confirms some variables, but presented two unpublished variables investigated in adolescents; the first is AGP-A, and the second is TAC. Although the association with 25 (OH) D was for TAC and not for AGP-A, the data stimulate the need for these variables to be replicated in later studies to better determine the influence of vitamin D insufficiency/deficiency in adolescents.
CONCLUSION
The most relevant finding of our study is the association of 25 (OH) D with calcium and triglycerides regardless of gender, even in this population of young people. In addition, female gender, BMI, WC and WHtR were already associated with hypovitaminosis D. These data indicate that nutritional status is as important as hypovitaminosis, so that it should be considered along with the levels of 25 (OH) D in evaluating the health state of adolescents. Thus, it is important to develop strategies for the prevention and control of obesity and inadequate nutritional status of vitamin D.















