INTRODUCTION
Hospitalized patients and critically ill patients in intensive care units may often present malnutrition, hypermetabolism, increased risk of infections, complications, increased length of stay in the hospital and in the intensive care units, and develop high mortality rates 1,2,3,4,5. They also have, for the most part, an intake of energy and proteins below their needs when fed with nutritional therapy; this issue of energetic and protein goals are much discussed in the pertinent literature 6,7,8,9.
Calorie and protein inadequacy in severely ill patients 6 was investigated in intensive care units of a university hospital and it was found that in more than half of the patients assessed, this inadequacy occurred.
A recently developed study with critically ill patients admitted in intensive care units 10 receiving enteral and parenteral nutrition therapy in several Latin American countries showed a high prevalence of malnutrition, with 74.1% patients exhibiting severe or moderate malnutrition. The study also showed that many critically ill patients receiving nutritional therapy did not reach the goals of energy consumption established 10.
In a recent study Siqueira-Paese et al. 11 evaluated the influence of caloric and protein deficit, length of hospital stay and mortality in critically ill patients, and found a high incidence of caloric and protein deficit. The authors also showed that both deficits contributed to the increase in length of hospital stay 11. Lee et al. 12 demonstrated that the energy and protein adequacy, greater than or equal to 2/3 of the prescribed values, was associated with a tendency of increased mortality in 60 days in those critically ill patients with mechanical ventilation.
In view of such considerations, the objective of this study was to investigate whether the calorie and protein deficits, the diagnosis and the NUTRIC score, behaved as risk factors associated to the survival time, in critically ill patients hospitalized in an intensive care unit.
CASES AND METHODS
STUDY DESIGN AND ETHICAL APPROVAL
A prospective longitudinal study was conducted with adult patients hospitalized in an intensive care unit (ICU) of a university hospital. Demographic, clinical, nutritional and other variables in connection with enteral nutritional therapy (ENT) were evaluated by the investigators involved in the study.
The study protocol was approved by the research Ethics Committee of the Institution and the Free and Informed Consent Form was signed by the research participant or by his/her relatives. This study did not receive external funding.
STUDY PARTICIPANTS
For the eligibility of the population to be studied, critically ill patients in the ICU of the hospital, aged over 18 years and under exclusive enteral nutritional therapy (EENT) were considered criteria for inclusion. Study exclusion criteria included patients who were receiving other routes of nutritional therapy (oral or parenteral), even if receiving concomitantly EENT and those patients with an EENT period of less than 3 days. Thus, eighty-two patients (n = 82) were recruited from the ICU of the hospital; they were evaluated in the first 24 hours after ICU admission, at the beginning and at the end of the EENT, as well as every 5 days, during the hospitalization period.
DEMOGRAPHIC, CLINICAL AND NUTRITIONAL VARIABLES
Data such as sex, age, diagnosis, ICU length of stay and length of ENT were collected directly from the medical records. In addition, ICU daily medical and nutritional records were used to collect all the information inherent to the administration of ENT (calorie and protein goals, caloric and protein deficit); complications during the procedure; nutrition risk in the critically ill score (NUTRIC score); body mass index (BMI); C-reactive protein (CRP), albumin, and whether the patient eventually died.
For the calculation of BMI, the criteria established by the WHO, 1995 13), for adults up to 60 years of age and by Lipschitz (1994) 14) for the elderly (> 60 years) were used. When it was not possible to weight bedridden patients, a defined equation was used to estimate body weight 15).
The present study adopted the NUTRIC score tool that represents the first nutritional risk assessment tool developed and validated specifically for ICU patients, as described by Heyland et al. 16. The nutritional risk state for critically ill patients in intensive care unit (ICU) was defined by the NUTRIC score16, which addresses variables such as acute physiology and chronic health evaluation II (APACHE II), the sepsis-related organ failure assessment (SOFA), age, number of comorbidities, and total days of hospital stay prior to admission to the ICU. Values ≥ 5 were considered to be of higher nutritional risk by NUTRIC score 16.
In the analysis of the laboratory tests, the serum albumin dosage was considered, and the following classification cutoff points were used: > 3.5 mg/dl (reference values); between 2.8-3.5 mg/dl (mild depletion); between 2.1-2.7 mg/dl (moderate depletion) and < 2.1 mg/dl (severe depletion) 17.
For evaluation of the C-reactive protein (CRP), the dosages taken every 5 days, the same day or the closest day (maximum 2 days before or after) with regard to the albumin dosage were considered. Thus, the value of the CRP found was only used for the calculation of the inflammatory-nutritional index CRP/albumin, and was not used alone for the evaluation of the patient. This exam collection was performed with the patient fasted for 8 hours and the cut-off point for inflammatory assay was < 0.5mg/dl (18). In the evaluation of the risk of severely ill patients, we used the inflammatory-nutritional index CRP/albumin. The recommendation proposed by AHA, 2003 18, was considered in the classification of risk for complications. Such recommendations establish the following: CRP/albumin ratio < 0.4 (without risk); 0.4-1.2 (low risk); 1.2-2.0 (medium risk); and > 2.0 (high risk) 18,19.
ENERGY AND PROTEIN GOALS
The energetic and protein goals for the administration of ENT in critical ICU patients were established according to the guidelines of the American Society for Parenteral and Enteral Nutrition (ASPEN) 20 (25-30 kcal/kg current body weight/day and 1, 2-2 grams of protein/kg current body weight/day).
DEFINITION OF CALORICAND PROTEIN DEFICITS
Caloric and protein deficits were calculated daily by subtracting the infused amount from the prescribed amount. The total deficit was calculated by the sum of all the deficits during the ICU stay. The average deficit per patient was calculated by dividing the total deficit by the number of days as ICU inpatient. Critical deficits were defined by the 75th percentile of the mean deficit. Thus, critical caloric level was defined as a value equal to or above 426 kcal/day (≥ 426 kcal/day) and as critical protein level, values equal to or above 18.4 g/day (≥ 18.4 g/day). This method was also used in another study 11.
COMPLICATIONS
Gastrointestinal complications were considered when patients presented with abdominal distension, diarrhea or constipation as mechanical complications, patients who had displacement, loss or obstruction of the catheter and as unavoidable complications, procedures such as tracheostomy, extubation, exams and surgeries.
STATISTICAL ANALYSIS
Initially a descriptive data analysis was carried out, with frequency tables for the categorical variables and position and dispersion measurements for the numerical variables. The chi-square or Fisher's exact test was then used when necessary to compare proportions between demographic and clinical variables (gender, categorized BMI, diagnosis, classified NUTRIC score, presence of intercurrences, risk assessed by CRP/albumin ratio and death) and the caloric and/or protein deficit variables. In the comparison of numerical measures (age, BMI, ICU time, enteral nutrition time and number of days with intercurrences) between 2 groups, the Mann-Whitney test and between 3 groups the Kruskal-Wallis test were used. In order to identify risk factors associated with time to death, the univariate and multiple Cox regression analysis were used. The stepwise variable selection process was used. The Kaplan-Meyer method was used to estimate survival distributions. The level of significance adopted for the statistical tests was 5% 21,22,23,24.
RESULTIS
It was observed that the patients who presented with caloric deficit, had also an average number of days with major intercurrences (p < 0.001). The protein target in patients who presented with critical caloric deficit was lower, on average, than in those patients who did not exhibit caloric deficit (p = 0.0087). The presence of ENT mechanical complications was greater in percentage among those patients who presented caloric deficit (61.9% versus 36.1%), with a statistically significant difference (p = 0.0389). There was also a higher risk of CRP/higher albumin level among patients presenting a critical caloric deficit when compared to those patients who did not present with a caloric deficit (100.0% versus 80.3%), with a statistically significant difference (0.0308). It was also observed that 37.8% (n = 31) of the patients eventually died (Table I).
Table I. Comparison of the studied variables with the caloric deficit of critically ill patients

BMI: body mass index; ICU: intensive care unit; ENT: enteral nutrition therapy; ICU and ENT time are in days; CRP/albumin: CRP/albumin risk.
1Mann-Whitney test
2Chi-square test; 3Fisher's exact test.
3Fisher's exact test.
Among patients with protein deficiency, a mean number of days with major intercurrences (64.2 days versus 40.9 days) was observed as compared to those patients who did not exhibit protein deficiency, with a statistically significant difference (p < 0.0001). The protein target also showed a statistically significant difference (p = 0.0219), between the two groups, that is; patients who exhibited a protein deficit had a lower protein target (Table II).
Table II. Comparison of the studied variables with protein deficiency of critically ill patients

BMI: body mass index; ICU: intensive care unit; ENT: enteral nutrition therapy; ICU and ENT time are in days; CRP/albumin: CRP/albumin risk.
1Mann-Whitney test
2Chi-square test; 3Fisher's exact test.
3Fisher's exact test.
The mean number of days with intercurrences (p < 0.0001) and protein target (p = 0.0184) were statistically significant. In other words; the mean number of days with intercurrences was greater among patients who exhibited calorie or protein deficit. And the protein target was lower in the same group (Table III). It was also found that there was no statistically significant difference in the average caloric prescription/infusion and the average protein prescription/infusion between the two patient groups, with and without caloric and/or protein deficit, as observed in Table I, Table II, Table III.
Table III. Comparison of the studied variables with the caloric and/or protein deficit of critically ill patients

BMI: body mass index; ICU: intensive care unit; ENT: enteral nutrition therapy; ICU and ENT time are in days; CRP/albumin: CRP/Albumin risk.
1Mann-Whitney test
2Chi-square test; 3Fisher's exact test.
3Fisher's exact test.
In this comparative review, it was possible to verify that there was a major occurrence of deaths among older patients (67.5 years versus 56.0 years), with a significant difference (p = 0.0068). There was also a greater occurrence of death in those patients with nutritional risk based on NUTRIC score ≥ 5 (p < 0.0001) and in those who experienced fewer complications (p = 0.0041) (Table IV).
Table IV. Comparison of the occurrence of death among all the variables studied
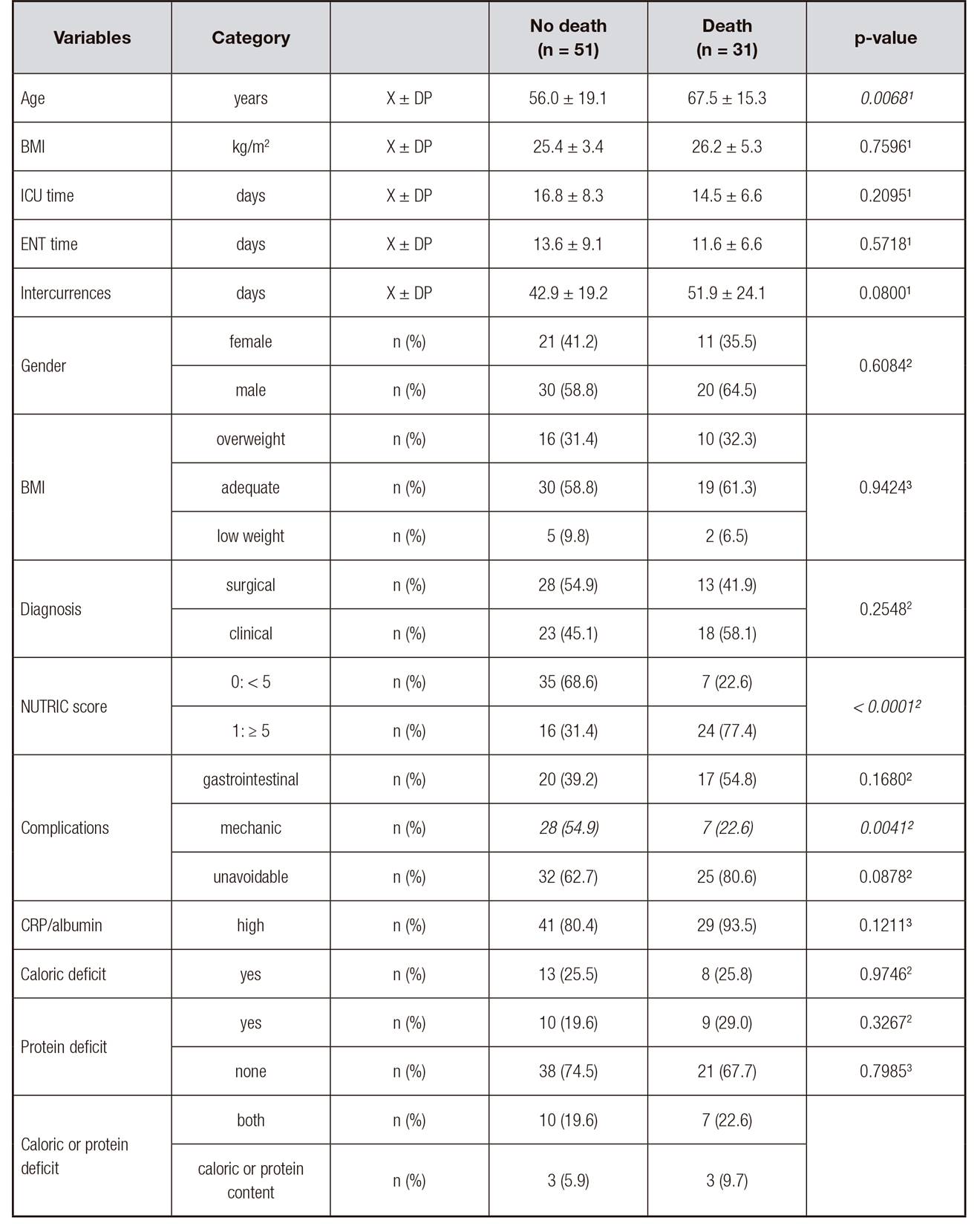
BMI: body mass index; ICU: intensive care unit; ENT: enteral nutrition therapy; ICU and ENT time are in days; CRP/albumin: CRP/albumin risk.
1Mann-Whitney test
2Chi-square test; 3Fisher's exact test.
3Fisher's exact test.
The variables age, number of days with intercurrences and the NUTRIC score; were significant in the univariate Cox regression analysis (Table V). One-year increase in age increased the risk of death in 4.1% (p = 0.0009; HR = 1.041). The increase of one day with intercurrences, increased the risk of death in 1.8% (p = 0.0485; HR = 1.018). Patients with NUTRIC score ≥ 5, presented with 5.4-fold higher risk of death (p < 0.0001; HR = 5.408), than those patients with a NUTRIC score < 5. In conclusion, the critical caloric and protein deficits did not behave as death risk factors in this population. The results of the Cox multiple regression analysis with stepwise variable selection criteria shown in Table V, that diagnostic and nutritional risk were the variables that together were associated to the survival time. The risk ratio was 2-fold greater for the clinical diagnosis (p = 0.0462; HR = 2.091) and 5.7-fold greater for the NUTRIC score ≥ 5 (p < 0.0001; HR = 5.740) (Table V). As it was verified in the regression analysis that the main factors associated to survival time were the diagnosis and the NUTRIC score, Kaplan-Meier curves were then performed for these factors.
Table V. Risk factors associated with death, analyzed by the univariate and multiple Cox regression model
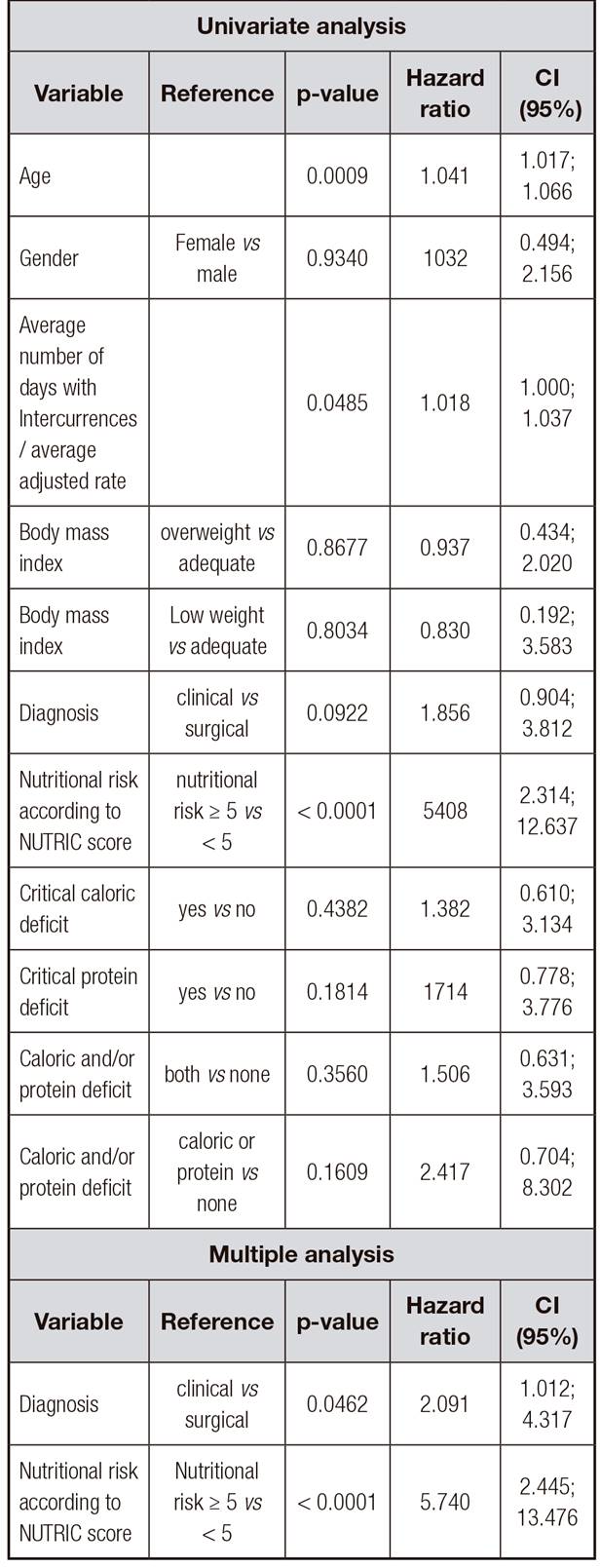
HR: Hazard ratio; CI 95%: 95% HR confidence interval.
Thus, Figure 1 shows the Kaplan-Meier curves for the major factors associated with survival time. It was possible to verify that the average survival time for patients with clinical diagnosis was 23.1 days (median 20 days), and with surgical diagnosis was 23.6 days (median 27 days). The probability of survival in 40 days was 28.1% for patients with clinical diagnosis and 40.2% for patients with surgical diagnosis. The mean survival time for patients with NUTRIC score < 5 was 34.5 days and 17.4 days (median 18 days) for patients with NUTRIC score ≥ 5. The probability of survival at 40 days was 72.8% for patients with NUTRIC score < 5 and 6.4% for patients with NUTRIC score ≥ 5 (Fig. 1).
DISCUSSION
Our study evaluated 82 critically ill patients in an ICU who received exclusively enteral nutrition because the main focus of the present study was to explore how the various clinical and nutritional variables would behave in patients fed with enteral nutrition only, and especially the differences found in the groups of patients with and without critical caloric and protein deficits.
In the group of patients with critical caloric deficit, there were more intercurrences, mechanical complications, higher risk of increased CRP/ albumin, and their protein target was lower. However, we did not find statistically significant association in ICU length of stay between patients who exhibited or did not exhibit caloric deficit. In an interesting study by Siqueira-Paese et al. 11, the authors showed that only 4% of patients did not present with caloric deficits, and also found a statistically significant correlation between length of hospital stay and both caloric and protein deficits.
In this study, more days of intercurrences and lower protein target were found in those patients who exhibited protein deficit. Another study highlighted that the protein inadequacy was associated with the length of hospitalization time (if shorter than or equal to 14 days), increased residual gastric volume and withdrawal or obstruction of the probe 6; these situations were not associated with the protein deficit in our study.
In this study, when the caloric and protein deficits were reviewed together, more days with intercurrences were observed in patients with caloric and protein deficiency. Both caloric and protein deficiency may affect the evolution of surgical patients in Intensive Care Units, as seen recently in a study conducted by Yeh et al., 2016 25. In a univariate analysis 11, a more critical caloric deficit was observed in patients hospitalized for trauma and when nutritional therapy was initiated after 12 hours of hospitalization. In the same study, a greater number of cases of critical protein deficiency was observed in patients who underwent nutritional therapy after 24 hours hospitalization and in those with the greatest number of organ failure 11.
In the present study, when we investigated the different variables and their relationship with the occurrence of death, a significant association was found between the occurrence of death and older age, with nutritional risk with NUTRIC score ≥ 5 and in those patients with a smaller number of mechanical complications. Different from the data found in the present study; in the study by Lee et al. 12, although increased mortality was observed when the adequacy of energy and protein was reviewed in relation to the prescribed amounts neither the energy nor protein adequacy alone, influenced the mortality in 60 days. The increase in mortality rate was associated with the energy and protein supply of ≥ 2/3 of the prescribed values only in patients with low nutritional risk in the first seven days of ICU admission 12.
Other studies that explored the relationship between energy and protein intake and clinical outcomes in critically ill patients 26 showed no association with mortality; but they pointed out that the caloric and protein deficits were associated with longer hospitalization time and longer mechanical ventilation 26.
In the study of Vallejo et al., 2017 10, with critically ill patients receiving enteral and parenteral nutrition, in different hospitals in Latin America, 74.1% of the patients presented with moderate or severe malnutrition according to the global subjective evaluation. And the NUTRIC score indicated a high need for nutritional therapy in 39.2% of the patients 10 . The study also indicated caloric deficits in more than 40% of the patients receiving enteral nutrition, with lower deficits observed in those patients who were receiving a combination of enteral and parenteral nutrition 10. Another study investigating the amount of calories and proteins in the postoperative period showed that patients with reduced caloric and protein intake had an increased risk of infection and extended hospitalization 27.
In the present study, the univariate Cox regression analysis showed that age, NUTRIC score and days with intercurrences behaved as factors associated with death. Later, in the Cox multiple analysis, only the diagnostic and the nutritional risk according to the NUTRIC score were associated with survival time. In this study, critical caloric and protein deficits did not remain associated with death. Data from another study 26, with critically ill patients, also showed no association between energy and protein intake with mortality.
In the study by Lee et al. 12, which investigated the relationship between energy and protein adequacy with mortality in critically ill patients, a 60-day 44.8% mortality rate was found, with approximately 27.9% of patients dying in the ICU. The study showed that the nutritional risk conditions, and not ICU length of stay, influenced the relationship between nutritional adequacy and mortality in 60 days 12. The authors also concluded that the energetic and protein adequacy ≥ 2/3 of the recommended amounts were associated with a 60-day trend in mortality among critically ill patients under mechanical ventilation. However, neither the energetic or protein adequacy, alone, of ≥ or < 2/3 of adequacy, affected the mortality in 60 days. The increase in mortality was associated with the supply of energy and protein in ≥ 2/3 of the prescribed amounts, which affected only patients with low nutritional risk 12.
In our study, the Kaplan-Meier curves showed that the diagnostic and the nutritional risk according to the NUTRIC score were the main factors associated with survival time. In another very interesting study 28, the authors also indicated the validity of the NUTRIC score in the identification of severely ill patients in intensive care units, who are more likely to benefit from adequate amounts of macronutrients when mortality is considered as an outcome. Another recent study conducted by Hsu et al., 2018 29, which investigated the energy and protein intake in enteral nutrition in elderly patients with severe illness and under mechanical ventilation, used the modified NUTRIC score to identify nutritional status. The authors showed a prevalence of elderly patients with high nutritional risk, and those patients who had caloric intake through enteral nutrition ≥ 80% of the prescription showed lower hospital and ICU mortality rates 29.
It is important to say that the present study adopted the NUTRIC score as a nutritional risk assessment criterion, as established in the study developed by Heyland et al. 16. The study developed by Heyland et al. 16 aimed to develop a scoring method for quantifying nutrition risk in the intensive care unit (ICU). In addition, at the study by Heyland et al. 16 for the development and validation of the method (NUTRIC score) it was also shown that patients with higher score had worse clinical outcomes, such as higher mortality and longer mechanical ventilation. The authors concluded that this tool (NUTRI score) represents the first nutritional risk assessment tool developed and validated specifically for ICU patients 16. For this reason, we have chosen to refer to the NUTRIC score as a risk assessment tool for severe ICU patients. There is also another study 30 showing that there is a strong positive association between nutritional adequacy and 28-day mortality in patients with a high NUTRIC score, but this association diminishes with decreasing NUTRIC score. Although it has been proposed by Heyland et al. 16 as a nutritional risk assessment tool for critical ICU patients, it is important to note that the NUTRI score needs further investigation, according to Arabi et al. 31.
As limiting factors of this study, we can report the challenges to obtain information in patients' charts. Considering it is a prospective study, the daily loss of patients and the difficulties of obtaining some important information from the teams involved in patient care made it difficult to evaluate some of the outcomes. Another limitation to be considered refers to the adoption in the present study of the criterion for the definition of critical deficit by the 75th percentile. It was not taken into consideration the fact that the caloric and protein target could be different in the acute phase of the disease in relation to the stable phase, which could leave to implications for the definition of caloric and protein deficit.
CONCLUSION
The findings of the present study allow us to conclude that caloric and protein deficits are not risk factors for mortality. Only the nutritional risk and diagnosis by the NUTRIC score were considered risk factors associated with survival time, in critically ill in-patients receiving ENT in an ICU.












 Curriculum ScienTI
Curriculum ScienTI


