INTRODUCTION
The incidence of obesity has increased among children and adolescents, and obesity has been considered one of the most serious public health problems in recent years (1). Childhood obesity, similar to that in adults, also carries risk factors for atherosclerosis and cardiovascular diseases, such as hypertension, dyslipidemia, low HDL cholesterol, and impaired glucose metabolism (2). The effect of obesity on metabolic disease has been previously demonstrated (2). Obesity has been considered an independent risk factor for chronic kidney disease (CKD). Therefore, concurrent with a dramatic increase in the frequency of end-stage renal disease (ESRD), many studies have been conducted on obesity as a risk factor for CKD. Moreover, body mass index has been reported as an independent predictor of CKD progression (3,4).
The significant increase in childhood obesity has in turn increased the number of kidney disease patients (5). Early detection of impairment in kidney function before a significant decline in glomerular filtration rate (GFR) is crucial. Blood urea nitrogen (BUN) and serum creatinine levels do not help in the recognition of early renal damage because detectable increases in these levels can be seen only after substantial kidney injury (6). Hence, early biomarkers of renal dysfunction such as cystatin C, neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1), and N acetyl-beta-D-glucosaminidase (NAG) were evaluated in several studies. These biomarkers were suggested to determine early renal damage and its location (7,8).
Urinary NGAL levels increase particularly in patients with acute kidney injury. NGAL is readily excreted and detected in the urine. Kidney tubular epithelial cells release NGAL in response to inflammation and other tissue insults (9). Furthermore, NGAL is a sensitive biomarker of tubular damage (10).
Kidney injury molecule 1 (KIM-1) is a type-1 transmembrane glycoprotein expressed in the glomerular and tubular epithelial cells of a damaged kidney. KIM-1 is untraceable in the normal kidney, but its level increases significantly in damaged kidneys (9). KIM-1 can be used to detect early renal damage in obese children (8).
Considering that the onset of obesity-associated renal disease is insidious and asymptomatic, we proposed early biomarkers to detect impaired renal function in obese adolescents. We aimed to determine the degree of impairment of kidney function by evaluating urine NGAL and KIM-1 levels in obese adolescents with normal serum creatinine (sCre) and BUN levels.
MATERIALS AND METHODS
PARTICIPANTS AND STUDY AREA
In total, 59 obese, 37 overweight, and 28 control adolescents were enrolled from the outpatient department at the Tokat Gaziosmanpasa University School of Medicine Hospital, Tokat, Turkey. Subjects were classified based on the body mass index (BMI) reference curve adjusted for Turkish children according to age and sex. Adolescents with a BMI above the 95th percentile were accepted as obese, those with a BMI between the 85th and 94th percentile were accepted as overweight, and those with a BMI within the 5-84th percentile were accepted as normal (11). Waist circumference was measured midway between the lowest rib and the iliac crest with a flexible anthropometric tape (12).
We excluded nine obese (three with familial Mediterranean fever, two with Hashimoto thyroiditis, and four aged < 10 years), 11 overweight (two with urinary tract infection; two with < 75 % of estimated GFR (eGFR), which was calculated according to the Schwartz formula, and seven aged < 10 years), and two control (one with urinary tract infection and one with familial Mediterranean fever) subjects. Finally, 50 obese, 26 overweight, and 26 control adolescents aged 10-16 years were enrolled. Figure 1 displays the flowchart depicting the study population.

Figure 1. Flowchart diagram of the study population (FMF: familial Mediterranean fever; eGFR: estimated glomerular filtration rate).
Subjects’ demographic and clinical data, basic demographic information (age and sex), and physical data (height, weight, BMI, and systolic and diastolic blood pressure) were recorded. Weights were measured using a digital scale (Seca Corp., Chino, California, USA) with the patients being barefoot and wearing light clothing. Height was measured using a portable stadiometer (Seca) together with weight. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). The demographic data and characteristics of the study group are shown in table I.
Table I. Demographic data and subject characteristics according to groups
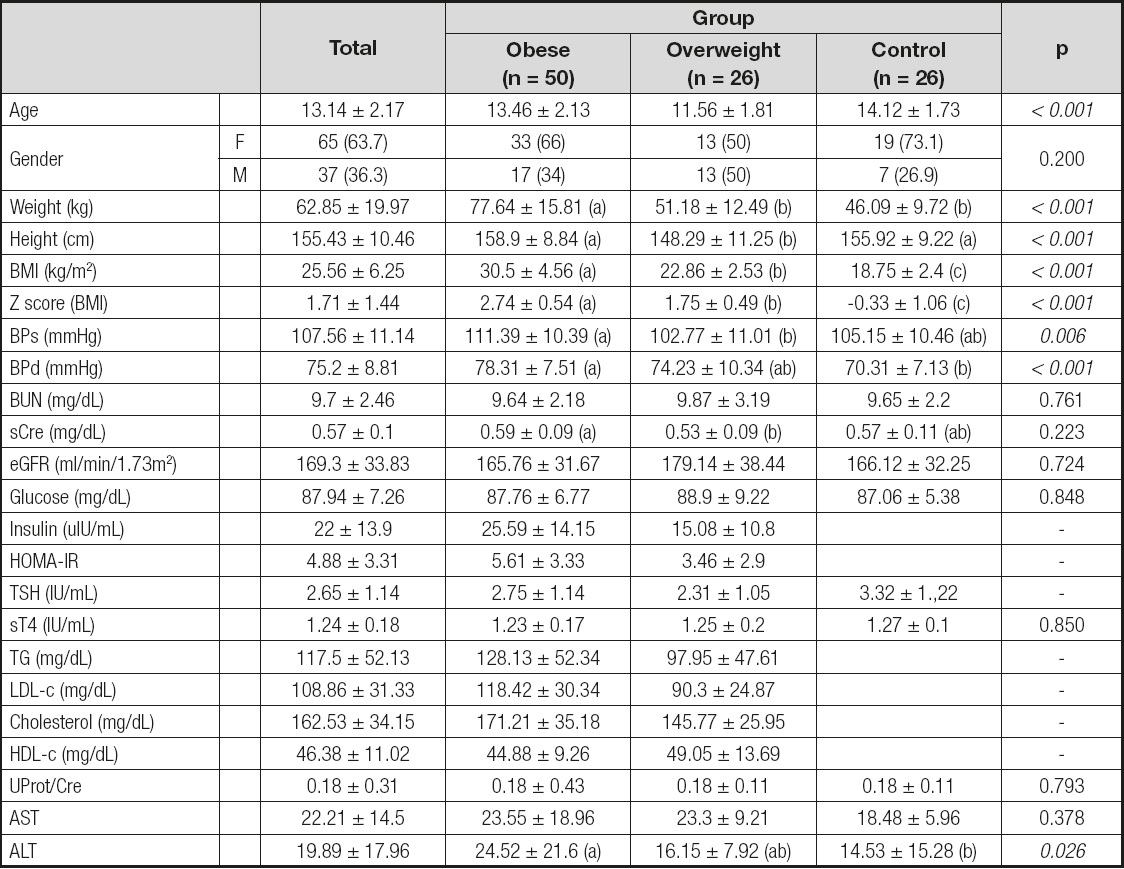
F: female; M: male; BPs: systolic blood pressure; BPd: diastolic blood pressure; BUN: blood urea nitrogen; sCre: serum creatinine; eGFR: estimated glomerular filtration rate; HOMA-IR: Homeostasis Assessment Model-Insulin Resistance; TSH: thyroid stimulating hormone; fT4: free T4; TG: triglycerides; LDL-c: low-density lipoprotein cholesterol; HDL-c: high-density lipoprotein cholesterol. Data are presented as number-percentage, mean ± standard deviation, using [Q1-Q3] for median. Chi-square and one-way ANOVA tests were used to compare groups. (ab): the common letter in a line means statistical insignificance. Statistically significant differences are shown in italics type. Age correction was applied for quantitative variables.
LABORATORY TESTS
Laboratory tests, including complete blood count, glucose, BUN, sCre, aspartate transaminase (AST), and alanine transaminase (ALT), were derived from fasting blood samples drawn from all participants, whereas insulin levels, lipid profiles, and thyroid function tests were only conducted on obese and overweight participants. Urinary creatinine and protein were determined from urine samples.
Serum fasting glucose, insulin, triglycerides (TGs), and high-density lipoprotein cholesterol (HDL-C) were detected using reagent kits from Roche Diagnostics adapted to the COBAS 6000 Autoanalyzer (Roche Diagnostics, Indianapolis, IN, USA). GFR was calculated using the Schwartz formula ([k × height]/sCre) in units of GFR mL/min/1.73 m2 (k constant, child or female adolescent: 0.55, male adolescent: 0.70).
Urine specimens were taken of 10 mL as spot urine, and centrifuged at 1,500 rpm for 5 min. The supernatant was removed and stored at -80 ºC. Urinary NGAL (Affymetrix eBioscience Human NGAL Platinum ELISA, Austria) and KIM-1 levels (Elabscience Biotechnology Co., Ltd, China) were measured using an enzyme-linked immunosorbent assay kit. Urinary NGAL and KIM-1 levels were expressed related to urine creatinine as pg/mL/creatinine for NGAL and ng/mL/creatinine for KIM-1.
DEFINITION OF HYPERTENSION, INSULIN RESISTANCE, DYSLIPIDEMIA, AND METABOLIC SYNDROME
Blood pressure was measured using a digital sphygmomanometer (OMRON 705IT, Omron Healthcare Co., Kyoto, Japan). Hypertension was defined as blood pressure ≥ 95th percentile according to age, sex, and height (13).
The homeostasis model assessment of insulin resistance (HOMA-IR) level was calculated using the following equation: HOMA-IR = fasting insulin (μU/mL) × fasting glucose (mg/dL)/405. The HOMA cutoff for insulin resistance diagnosis was 5.22 for male and 3.82 for female adolescents (14). Dyslipidemia was defined as the existence of any of these criteria: TGs > 136 mg/dL in children ≥ 10 years of age, and HDL-C < 35 mg/dL (15). We determined proteinuria with the urine protein/creatinine ratio in spot urine samples as ≥ 0.20 mg/mg (16).
Current definitions of metabolic syndrome (MetS) include the following key characteristics: hyperinsulinemia or insulin resistance, dyslipidemia, hypertension, and obesity, with a particular emphasis on central adiposity height (17,18).
STATISTICAL ANALYSES
Quantitative data are expressed as arithmetic mean and standard deviation. Categorical variables are demonstrated as number and percentage. An independent sample t-test or one-way analysis of variance was used to compare continuous normal data between groups. For multiple comparisons, Tukey’s HSD test was used. Chi-square tests or Kruskal–Wallis tests were used for categorical data analysis or non-normal data comparisons between groups. For examining the relationships between variables a simple correlation analysis and Pearson’s correlation coefficient were used. A value of p < 0.05 was considered statistically significant. The statistical analysis of the data was performed using the SPSS 19 (IBM SPSS Statistics 19, SPSS Inc., Somers, NY, USA).
RESULTS
NGAL and KIM-1 levels were studied in urine samples from 102 subjects. NGAL and KIM-1 levels were expressed as a ratio to urine creatinine levels. The results obtained according to each study group are summarized in table II. The nonparametric results of urinary NGAL and KIM-1 levels were shown using median values because their distribution was not homogeneous.
Table II. Urinary NGAL and KIM-1 levels according to groups

NGAL: ng/mL in urine; KIM-1: pg/mL in urine; NGAL/Cre: ng/mg; KIM-1/Cre: pg/mg. Data are presented using [Q1-Q3] for median. Chi-square, one-way ANOVA, and Kruskal-Wallis tests were used to compare groups. Age correction was applied for quantitative variables.
In addition, obese and overweight adolescents were grouped according to sex, proteinuria, MetS, hypertension, dyslipidemia, and insulin resistance, and statistical analyses were performed for NGAL and KIM-1 levels. In the obese and overweight group, urinary NGAL levels were higher in females than in males (p = 0.013) (Table III). Additionally, urinary NGAL levels were increased in obese and overweight adolescents with LDL dyslipidemia as compared with those without LDL dyslipidemia (p = 0.024) (Table III). Table III summarizes the obtained NGAL and KIM-1 levels according to these variables in the obese and overweight group. In the group with high triglyceridemia, urinary NGAL and NGAL/Cre levels were higher than in those outside this group (p = 0.032 and 0.020, respectively; Table III).
Table III. Urinary NGAL, NGAL/Cre, KIM-1, and KIM-1/Cre levels in the obese and overweight group according to gender and clinical disturbances

HT: hypertension; Cre: creatinine; TG: triglycerides; LDL-c: low-density lipoprotein cholesterol; HDL-c: high-density lipoprotein cholesterol. Data are presented using [Q1-Q3] for median. Kruskal-Wallis tests were used to compare groups. Age correction was applied.
The KIM-1/Cre ratio was higher in overweight adolescents with abdominal obesity than in those without abdominal obesity (52.89 [28.55-55.69] and 93.22 [63.48-133.04], respectively, p = 0.007). This significant difference was not determined in the obese group (65.75 [41.73-101.36] and 80.09 [30.23-129.95], respectively, p = 0.978).
We determined a correlation between insulin and HOMA-IR levels with the NGAL/Cre ratio in the overweight group (r = 0.515; p = 0.008, and r = 0.483; p = 0.014, respectively). No correlation was found between insulin and HOMA-IR levels with NGAL/Cre ratio in the obese group (r= -0.151; p = 0.296, and r = −0.149; p = 0.300, respectively). In the obese group, insulin and HOMA-IR levels were correlated with ALT levels (r = 0.388; p = 0.006, and r = 0.398; p = 0.005, respectively).
DISCUSSION
Obesity is suggested to contribute to renal disease (19). Early renal markers (NGAL, cystatin C, NAG, and KIM-1) have been used in studies to evaluate renal function because of the late presentation of obesity-related kidney disorders. NGAL and KIM-1 as tubular damage markers have been used to assess proteinuric, toxic, and ischemic kidney diseases (20,21). If metabolic disturbances are not considered, we determined that renal function is not yet affected in obese adolescents as compared to controls and overweight participants. We observed that the renal function of obese female adolescents may have been impaired when compared with that of male adolescents.
The mechanisms by which obesity may initiate and exacerbate CKD remain unclear. Deterioration in renal hemodynamics is very likely the main factor; however, a contribution of inflammatory and metabolic mechanisms may be considered. The time at which the harmful effects of obesity on the kidney can be determined has not been established yet. Savino et al. suggested that a longer exposure to obesity is probably needed before renal function impairment develops (22). Han et al. showed that KIM-1 can be excreted in the urine within 12 h after an initial ischemic renal insult, before regeneration of the epithelium, and then persists over time (23).
Hypertension, DM, and hyperlipidemia, all of which increase the risk of ESRD, are more prevalent in the obese population. Obesity is linked with glomerular hyperfiltration and hypertension (3). Hypertension and hyperfiltration may contribute to glomerulosclerosis (24). Consistent with Goknar et al. (8), we found that hypertension was not associated with kidney injury in obese adolescents. In the present study, no significant differences in eGFR were found between the obese, overweight, and control groups. However, Duzova et al. found that eGFR was lower in patients with higher BMI; hence, obese children had the lowest eGFR (25). We thought that these different findings would depend on our small sample size. Conversely, Duzova et al. reported that there was no significant difference between the groups in terms of frequency of subjects with eGFR < 75 mL/min/1.73 m2 (25). Also, Salman et al. reported that eGFR as calculated from sCre was higher in obese patients without MetS than in nonobese controls. They interpreted this as a symptom of hyperfiltration, which is the first stage of progression to renal dysfunction (26). Metabolic effects, including inflammation, insulin resistance, and adipokine dysregulation, may directly or indirectly affect renal structure and function (27). Conversely, inflammatory risk factors and lipid byproducts play a key role in the progression of renal dysfunction in obese adult patients (28). As mentioned above, consistent with the concept of a causal relationship between dyslipidemia and renal dysfunction, we found that the high LDL-c group had higher KIM1/Cre levels than the normal group. In the present study a statistically significant difference was found in the urinary excretion of NGAL between those with and without hypertriglyceridemia in the obese and overweight group. Intracellular accumulation of free fatty acids and triglycerides in renal glomerular and tubulo-interstitial cells may lead to renal lipotoxicity (29). Taken together, in agreement with the present study, abdominal obesity was reported to be an important risk factor for CKD (30).
In chronic hyperglycemia, especially in diabetes, the renin-angiotensin system and the endothelin system may induce hemodynamic effects, which lead to microvascular complications, and non-hemodynamic effects through an autocrine or paracrine action, which may contribute to the proliferation of kidney cells and the expression of growth factors or cytokines, leading to changes in renal function (31,32). Insulin resistance may be one of the real culprits in the development of glomerulosclerosis (33). Despite these mechanisms, consistent with the present study, Goknar et al. found that urinary injury markers did not differ among patients with insulin resistance and impaired glucose tolerance. These values have not correlated with fasting and postprandial glucose values (8). Conversely, urine samples from patients with diabetic nephropathy and SLE nephropathy, who had significant proteinuria (3 g/day) but no evidence of tubule necrosis on urine sediments, had no elevated KIM-1 protein levels (23). Furthermore, we found a positive correlation between insulin and HOMA-IR values with NGAL/Cre values in overweight subjects, but not in obese subjects. A study from the EGIR-RISC cohort reports that improving insulin sensitivity might also reduce or prevent albuminuria, in particular at very early stages (34). Based on these findings, renal function was correlated with insulin and HOMA-IR levels in the early stages of excess weight gain. However, in the later stages of obesity we thought that NGAL excretion could be disproportionate with further deterioration of tubular function. We judged that excretion of NGAL in urine might be unstable when tubular disorder progresses.
The aforementioned mechanisms have been suggested to explain the impact of obesity on renal function. However, a meta-analysis suggested that a high body mass index acts as an independent predictor of new-onset CKD, which remains currently undefined (35). In a cohort study, central adiposity and metabolic disturbances may lie in the causal pathway between obesity and CKD (30). Therefore, renal function is not affected by obesity as compared with the control group according to the results of the present study. Otherwise, based on systematic review findings from cohort studies, Wang et al. suggested that obesity increased the risk for kidney disease, including CKD, ESRD, kidney stones, kidney cancer, and RCC (3). So, in light of these opinions, the finding might suggest that debates on the timing of kidney injury by obesity will continue. After an average follow-up of > 6 years, obesity increased the risk of low eGFR and albuminuria by 28 % and 51 %, respectively (35).
Physiological differences in the kidneys of men and women may be driven by the kidney’s sex hormone receptors (36). Hill et al. reported a higher prevalence of CKD in women compared with men in a meta-analysis (37). Likewise, in our cohort, female obese adolescents excreted higher urinary NGAL levels than male obese adolescents. Hsu et al. suggested a higher risk for CKD in obese women when compared to obese men. This finding is due to a higher percentage of adipose tissue in obese women than in obese men (3). Differences in diet habits may also contribute to differences between genders.
Given that renal injury markers should be investigated in long-term, prospective, observational studies, the present study had a cross-sectional design and small sample size, which is a limitation of our study. By designing a longitudinal study, the effect of obesity on kidney function may be determined more accurately. The unsteady creatinine volume output will influence the data considerably. As such, the normalization of urinary markers as related to urine creatinine concentration poses a limitation. The strength of this study is that we chose to prospectively assess obese and overweight adolescents to evaluate kidney function. In the present study we also investigated the effects of all obesity-related comorbidities, i.e., hypertension, dyslipidemia, insulin resistance, and proteinuria, on kidney function in obese adolescents.
Further, comprehensive studies are needed to prove that obesity disrupts renal function in adolescents. In the present study we observed that obese and overweight adolescents had no notable renal dysfunction when compared with control adolescents. However, dyslipidemia in obesity affects kidney function. In addition, obesity impaired renal function in female adolescents as compared with male adolescents. Excretion of NGAL in urine might be unsteady when tubular disorder progresses. We suggest that the use of normalization of the urinary marker to urine creatinine ratio should be discussed.














