INTRODUCTION
The complexity of anti-cancer therapy, including multidisciplinary support, is extremely important for advanced cancer patients. According to the European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines, the nutritional status of all cancer patients should be screened regularly due to a high risk of malnutrition (1). Additionally, the risk is higher in patients with advanced stage of malignancy. The presence of malnutrition in these patients is frequent and limits the response to anti-cancer therapy (1). Among others, malnutrition affects clinical outcome and increases the length of hospital stay, both of which impair quality of life (QoL) (2). Therefore, an assessment of the nutritional status of these patients is strongly required (3). Currently, several screening tools are available to assess nutritional status — for instance, the Nutritional Risk Screening 2002 (NRS 2002) or the Subjective Global Assessment (SGA) tool. In the study by Kaźmierczak-Siedlecka including 84 patients with gastric and esophageal cancer, it was shown that all patients qualified for home enteral nutrition were at risk of malnutrition or malnourished, hence they required nutritional treatment. Very importantly, 40.4 % of them scored “5” in the NRS 2002 tool (4). Thoresen et al. have reported that 65.22 % of advanced cancer patients were malnourished according to the SGA method (5). Anorexia, early satiety, dry mouth, nausea, and pain were the most frequent symptoms affecting food intake (5). SGA has been shown to be the best predictor of clinical outcome in comparison with NRS 2002, as the survey provides individual indicators of nutritional status (e. g., changes in body mass, serum albumin, food intake), and hand-grip [6,7]. Notably, SGA is easy to use and non-invasive. The modified version of SGA is called the Patient-Generated Subjective Global Assessment (PG-SGA), which additionally reports on the presence of nutritional symptoms and short-term weight loss (8). The Global Leadership Initiative on Malnutrition (GLIM) proposed a grading of severity of malnutrition as follows — stage 1 (moderate) and stage 2 (severe) (9). It should be emphasized that GLIM criteria were published in 2019, and therefore the data regarding these criteria and advanced cancer patients are limited (9).
Complex anti-cancer care, among other measures, should be focused on the psychosocial functioning of patients. The presence of cancer significantly deteriorates QoL (10,11). In the study by Ahlam et al., it was shown that a majority of Moroccan patients on advanced palliative care experienced impaired QoL in all aspects of physical and emotional functioning (12). QoL was strongly related to symptoms such as fatigue, loss of appetite, and insomnia. Severe fatigue was noted in 64.2 % of individuals (12). Smith et al. have reported that pain, anxiety, and depression were associated with the impairment of QoL seen in advanced cancer patients (13). Overall, the care of advanced cancer patients involves an assessment and, consequently, maintenance or improvement of QoL (10).
The primary aim of this study was to assess the nutritional status and QoL of cancer patients at advanced stage of their malignancy. The secondary aim was to investigate the impact of malnutrition severity on the QoL of these patients.
MATERIAL AND METHODS
PATIENTS
Participants (n = 35) were recruited by a surgeon and nutritionist at the Nutritional Counselling Centre Copernicus in Gdansk and the Department of Surgical Oncology (Medical University of Gdansk, Poland). Inclusion criteria were: ≥ 18 years old (y.o.), presence of advanced-stage cancer of the upper GI tract or head and neck cancer, and provision of a written, informed consent to take part in this study. The participants were included into this study if they met all inclusion criteria and were hospitalized in or cared for by the above-mentioned institutions. The patients were at an advanced stage of cancer and with no active anti-cancer treatment during enrolment in this study.
STUDY DESIGN
The flow-chart of this study is presented in figure 1. A total of 35 patients were assessed as eligible for this study. Among these, 2 were excluded because they had not provided their written consent to participate in this study.
OUTCOMES
The assessment of nutritional status in study participants was done using the SGA method, which is divided into 3 parts: medical interview, physical examination, and final assessment of nutritional status. Malnutrition was also categorized into stage 1 and stage 2 using the GLIM criteria.
GLIM stage 1 requires one of the following criteria to be met:
1. Unintentional weight loss (5-10 % within the past 6 months, or 10-20 % beyond 6 months),
2.Low BMI (< 20 kg/m² if < 70 yrs, < 22 kg/m² if ≥ 70 yrs),
3. Reduced muscle mass (mild to moderate deficit).
GLIM stage 2 requires one of the following criteria to be met:
1. Unintentional weight loss (> 10 % within the past 6 months or > 20 % beyond 6 months),
2. Low BMI (< 18.5 kg/m² if < 70 yrs, < 20 kg/m² if ≥ 70 yrs),
3.Reduced muscle mass (severe deficit).
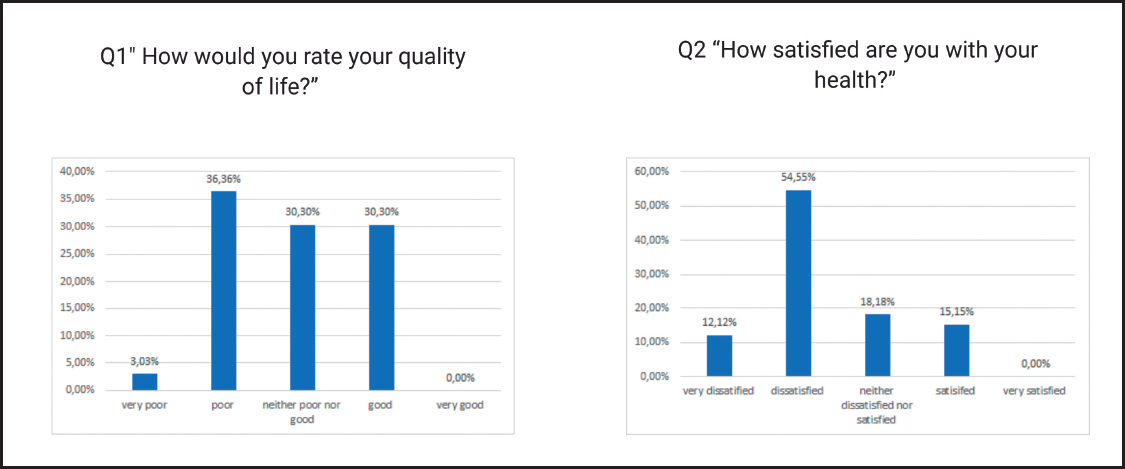
Another endpoint was assessing QoL in advanced cancer patients. This was done using the World Health Organization Quality of Life-BREF (WHOQOL-BREF) questionnaire, which consists of 26 questions divided into 4 domains (D1: environmental, D2: psychological, D3: somatic, and D4: social factors). Additionally, a first question (Q1) “How would you rate your quality of life?” serves as self-assessment of QoL (1 point means “very poor” and 5, “very good”), and a second question (Q2) “How satisfied are you with your health?” serves as self-assessment of health status (1 point means “very dissatisfied” and 5, “very satisfied”).
STATISTICAL ANALYSIS
The statistical analyses were performed using the STATISTICA package, version 13.0, and Microsoft Excel 2019 PL. Normality was tested with the Shapiro-Wilk test. In case of nutritional status assessment, the significance of the difference between groups was tested with Pearson’s chi-squared test. To compare QoL scores between groups, the Mann-Whitney U-test and the Kruskal-Wallis H-test were used, as appropriate. A statistical significance level of p = 0.05 was adopted.
RESULTS
PATIENT CHARACTERISTICS
A total of 35 participants were invited to the study. Two patients refused to take part in the study and were excluded. Statistical analyses were performed for observed cases only. The majority of patients suffered from head/neck (n = 12, 33.33 %) and espohageal cancer (n = 11, 33.33 %). PEG (n = 14, 42.42 %) and jejunostomy (n = 13, 39.39 %) were the most frequent artificial accesses to the alimentary tract in use for enteral feeding.
Patients with head/neck cancer most often were fed via PEG. In case of esophageal and gastric cancer, the most common artificial access to the alimentary tract was jejunostomy (45.45 % and 70 %, respectively). All patients (except one who consumed ONS enriched with protein) received a standard, normo-caloric enteral formula with no additional fiber.
NUTRITIONAL STATUS
Regarding the SGA evaluation (Table III), most of the patients were malnourished (n = 14, 42.42 %) or severely malnourished (n = 14, 42.42 %). Patients with head/neck cancer were more often severely malnourished in comparison to those with esophageal and gastric cancer (n = 7, 58.33 % vs. n = 4, 36.36 % and n = 3, 30 %, respectively); however, the difference was not statistically significant (p = 0.70675).
Table II. Characteristics of patients with head/neck, espohageal, gastric cancer according to type of nutritional support/artificial access to the alimentary tract

ONS: oral nutritional supplement; PEG: percutaneous endoscopic gastrostomy; NCJ: needle catheter jejunostomy.
Table III. Assessment of nutritional status based on the SGA tool
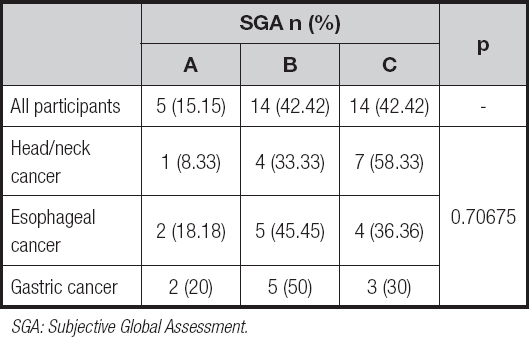
SGA: Subjective Global Assessment.
According to the 2019 GLIM criteria, ntwenty-three patients (69.7 %) were severely malnourished. Patients with head/neck advanced cancer suffered from severe malnutrition more often than those with esophageal or gastric advanced cancer (n = 9, 69.7 % vs. n = 8, 72.73 % and n = 6, 60 %, respectively); however, the difference was not statistically significant (p = 0.72151).
QUALITY OF LIFE
The assessment of QoL is presented in table V. Among all participants, the highest impairment of QoL was seen in Q2, D1, and D2. Patients with esophageal and advanced gastric cancer had better QoL in Q2 and all domains in comparison with subjects with advanced head/neck cancer; the difference was not statistically significant, though. Moderately malnourished patients (GLIM stage 1) had better QoL in Q1, Q2, and all domains when compared to severely malnourished individuals; the difference was statistically significant in Q1, D1, and D2. Patients at risk of malnutrition (SGA A) had better QoL in Q1 and all domains as compared to malnourished subjects (SGA C); the difference was significant statistically in D2 (p = 0.0310). Additionally, moderately malnourished (GLIM stage 1) patients with advanced head/neck cancer had better QoL in Q2 and all domains when compared to those severely malnourished (GLIM stage 2); the difference, however, was not statistically significant. Moderately malnourished (GLIM stage 1) patients with advanced esophageal cancer had better QoL in Q1, Q2, and all domains in comparison to those who were severely malnourished (GLIM stage 2); the difference was statistically significant in Q1 and D1. Moderately malnourished (GLIM stage 1) patients with advanced gastric cancer had better QoL in Q1, D3, and D4 when compared to those who were severely malnourished (GLIM stage 2); the difference was significant statistically in Q1.
Table IV. Assessment of nutritional status based on the 2019 GLIM criteria
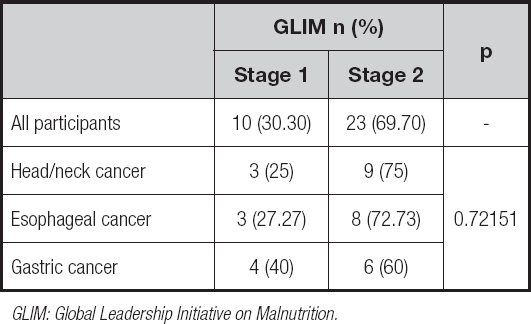
GLIM: Global Leadership Initiative on Malnutrition.
Table V. Assessment of QoL

ONS: oral nutritional supplement; GLIM: Global Leadership Initiative on Malnutrition; SGA: Subjective Global Assessment; Q1: question 1 “How would you rate your quality of life?”; Q2: question 2 “How satisfied are you with your health?”; D1: environmental domain; D2: psychological domain; D3: somatic domain; D4: social factors.
The patients’ self-assessment of QoL and satisfaction with their health status is presented in figure 2. A total of 36.36 % (n = 12) self-assessed QoL as “poor”. Notwithstanding this, 54.55 % (n = 18) of patients declared they were dissatisfied with their health.
DISCUSSION
The assessment and improvement of the nutritional status and QoL of cancer patients have been recognized as an important part of complex anti-cancer care. Previous trials have demonstrated that in cancer patients QoL and nutritional status deterioration is frequent. However, the studies assessing the severity of malnutrition in advanced cancer patients according to the GLIM criteria are very limited. Additionally, to the best of our knowledge, the present study is the first to assess the impact of malnutrition severity, based on the GLIM 2019 criteria, on QoL in advanced cancer patients. The present study assessed the nutritional status and QoL of patients with advanced head/neck, esophageal, and gastric cancer.
According to the ESPEN, malnutrition leads to impairment of physical and mental functions, deteriorates QoL, and increases treatment costs (14). Additionally, it is associated with incremental morbidity and mortality [9,15]. Therefore, the assessment of nutritional status and, consequently, the identification of patients at risk of malnutrition, malnourished or severely malnourished are necessary for the potential introduction of an appropriate nutritional treatment. The PG-SGA is an international method used to assess nutritional status (14). In the present study, according to the SGA, 84.84 % of patients were evaluated as malnourished (SGA B + C), while 42.42 % subjects amongst all participants were severely malnourished (SGA C). Similarly, Wiegert et al. evaluated the nutritional status of advanced cancer patients in palliative care (n = 120) in Brazil using the PG-SGA instrument (16). It was shown that 94.2 % of patients were malnourished (16). Moreover, another trial including 172 advanced cancer patients also in Brazil, showed that 83.6 % of these patients were malnourished (PG-SGA B + C) (17). The results of the above-mentioned studies have confirmed that malnutrition occurs commonly in advanced cancer patients, revealing a need for assessment of nutritional status in this group of patients. Patients with head/neck cancer are particularly at high risk of malnutrition. The location and size of these tumors have a significant impact on the swallowing process, hence on food intake (18). Therefore, an appropriate nutritional support should be introduced as soon as possible to prevent the development of malnutrition in these patients. In our study, we report that patients with head/neck cancer were most often fed via PEG, and all of them received enteral formulas. Additionally, the present study has shown that patients with advanced head/neck cancer suffer from severe malnutrition (SGA C) more often than those with esophageal and advanced gastric cancer (58.33 % vs. 36.36 % and 30 %, respectively); however, the difference was not statistically significant (p = 0.70675). Similar results were noted when GLIM criteria were taken into consideration (75 % vs. 72.73 % and 60 %, respectively; p = 0.72151).
In the present study, 54.55 % of all participants declared that they were dissatisfied with their health. Moreover, 36.36 % of patients self-assessed their QoL as a poor. A major deterioration of QoL was noted in the environmental and psychological domains. Notwithstanding this, a significant difference in the self-assessment of QOL and particular domains was not noted. Enteral nutrition is known to be a life-saving procedure; however, feeding via an artificial access to the alimentary tract is not physiological or comfortable for patients (19). Similarly, patients with advanced head/neck cancer had a more deeply impaired QoL as compared to subjects with esophageal and gastric advanced cancer; however, the difference again was not statistically significant. Patients with cancer of the head/neck or upper portions of the gastrointestinal tract often cannot consume food orally or swallow because of pain, thus, they require enteral nutrition. Consequently, tube-feeding often causes a loss of social contacts as well as an impairment in self-assessed physical appearance (19). Moreover, we reported that moderate malnutrition (GLIM stage 1) was correlated with a better QoL when compared to a severe stage (GLIM stage 2). Patients at risk of malnutrition (SGA A) had a better QoL in 4 domains when compared to severely malnourished subjects (SGA C); however, the difference was statistically significant in the psychological domain. Similar results were obtained in the study by Shahmoradi et al. (20). It was shown that PG-SGA scores significantly correlated with quality of life scores (r2 = 0.38, p < 0.05), psychophysiological well-being (r2 = 0.37, p < 0.05), functional well-being (r2 = 0.42, p < 0.05), and well-being (r2 = 0.07, p < 0.05) (20). Indeed, it confirmed that malnutrition, and more precisely the severity of malnutrition, affects a patient’s QoL.
To the best of our knowledge this is the first study comparing the QoL of patients with different stages of malnutrition according to the new 2019 GLIM classification. In summary, in this study we demonstrated that nutritional status and QoL deteriorate in patients with head/neck, esophageal, and gastric cancer. According to both tools, SGA and 2019 GLIM criteria, most of them were severely malnourished. Additionally, the severity of malnutrition has an impact on the QoL of cancer patients. Severe malnutrition significantly impairs QoL in the psychological (GLIM stage 2, SGA C) and somatic domains (GLIM stage 2).
The present study has some limitations. Firstly, the sample size is small. Secondly, the group is non-homogenous. No specified data concerning tumor stage and ongoing oncological therapy were reported.