INTRODUCTION
Patients with chronic kidney disease (CKD) undergoing hemodialysis (HD) have several hydroelectrolytic and metabolic alterations, which are associated with the therapy itself, representing a strong impact on their body composition and consequently on nutritional status (1).
Anthropometric measurements (weight, height, skinfolds, and circumferences) are widely used in the nutritional assessment of patients with CKD. In clinical practice, measurement of the body mass index (BMI) and sum of four skinfolds (SSKD) and bioelectrical impedance analysis (BIA) are simple and easy-to-apply methods (2).
Dual-energy X-ray absorptiometry (DEXA) is a consensual reference standard method for measuring body fat (BF) in HD patients (3-5). However, this method requires an adequate location, sophisticated equipment, and a trained evaluator, and has a high cost, making it difficult to use in clinical practice (6).
Thus, taking into account the several factors that interfere with the adequate measurement of body composition in dialysis patients, this study aimed to evaluate the concordance of BIA and sum of four SSKD measurement with the reference method DEXA in the estimation of the percentage of total BF of patients with CKD undergoing HD.
MATERIALS AND METHODS
This cross-sectional study was conducted in patients with CKD in five HD centers in the city of São Luís, located in the state of Maranhão, Brazil.
The sample size was calculated considering a population of 1,080 patients with CKD undergoing HD, a power of 80 % to detect a 1.5 % minimum difference between the methods, and an expected concordance of at least 0.4, totaling 226 patients. Taking into account possible losses, the sample size was increased by 25 %. Thus, the minimum sample size was 283 individuals.
The study included 317 patients who met the eligibility criteria: both sexes, age of ≥ 18 years, regular enrollment in an HD program for at least 3 months, dialysis sessions of at least 3.5 h, and agreement to participate in the study (free and informed consent form). Pregnant patients, amputees, and patients with neurological diseases or sequelae of stroke, autoimmune and infectious diseases, cancer, and acquired immunodeficiency syndrome were excluded.
Variables, such as sex, age, self-reported skin color, and income in multiples of the minimum salary (US$ 202.75 in 2016), obtained from the medical records and via individual interviews, were used to describe the study sample.
An anthropometric and body composition evaluation was performed 30 min after the intermediate HD session of the week, as recommended in the NKF-KDOQI (5). Dry weight, height, and the following skinfolds were measured: biceps, triceps, suprailiac, and subscapular using an adipometer (Lange Skinfold Caliper®, USA), in addition to the BIA (Biodynamics® BIA 450 Bioimpedance Analyzer, Seattle, WA, USA) and DEXA based on enCORE (model Lunar Prodigi-GE Healthcare®) findings.
Dry weight was measured with the aid of a calibrated scale (Filizola®, Brazil) and height with a portable stadiometer (Alturexata®, Brazil). BMI was calculated as dry body weight (kg) and height squared (cm).
Waist circumference (WC) was measured using an inextensible, flexible, and millimetric tape (Sanny®) at the midpoint between the last rib and the iliac crest.
The sagittal abdominal diameter (SAD), described as the distance from the small area of the back to the upper abdomen, was also measured using an abdominal caliper (Holtain Kahn Abdominal Caliper®) with a subdivision of 0.1 cm. It was measured in duplicate, and the arithmetic mean was calculated. The measurement was performed with the patients in the supine position and with their knees flexed. The calibrator was positioned at the midpoint between the last rib and the iliac crest, at the height of the intervertebral discs, more precisely between the fourth and fifth lumbar vertebrae (L4-L5) and the upper arm of the calibrator sliding in the upper abdomen until touching it, without compression; at this time the reading was performed (7).
The skinfold was measured in triplicate with the aid of an adipometer (Lange Skinfold Caliper®, USA) on the opposite side of the arteriovenous fistula or catheter. The measurement of the sum of the means of the folds followed the proposal of Durnin and Womersely (8) for the calculation of body density; subsequently, the Siri formula (9) was applied to determine the body fat percentage (%BF).
The %BF was also evaluated using BIA and DEXA. For BIA, a tetrapolar apparatus (Biodynamics® BIA 450 Bioimpedance Analyzer, Seattle, WA, USA) was used, with an 800-to-50-kHz electric current. The patients were placed in the supine position, with their arms extended and separated from the trunk, and their legs separated so that the thighs did not touch. Two electrodes were placed on the hand and wrist and two on the ankle and foot, on the opposite side of the arteriovenous fistula or catheter.
DEXA (Lunar Prodigi, GE Healthcare®) was performed in an interval of up to 24 h after a dialysis session, with the patients in the supine position, wearing specific clothes for the examination, barefoot, and without any accessory or metal object.
Patient characteristics are presented as frequencies and percentages for categorical variables, and means and standard deviations for numeric variables. Shapiro-Wilk's test was used to test the normal distribution of numerica variable. The Mann-Whitney test was employed to determine the potential differences between sex and the Wilcoxon-signed rank test to verify the difference between the means of DEXA, BIA, and SSKD measurements. The concordance among the %BF evaluated using the three methods was analyzed by sex and tertile through the Lin's concordance correlation coefficient (CCC-L) using the statistical program STATA 14.0 and assuming a significance level of 5 % for all analyses.
This work was submitted to the Ethics Committee of the University Hospital of the Federal University of Maranhão in compliance with the requirements required by the Resolution of the National Health Council No. 466/12 and its complementaries for research involving human beings, being carried out in accordance with the Declaration of Helsinki, obtaining its approval through the consolidated opinion nº 275.351.
RESULTS
The study sample consisted of 317 individuals with a mean age of 50.4 ± 14.9 years, who were predominantly men (62.4 %) and self-reportedly black or brown (74.4 %), who lived in the interior of the state (31.1 %), and who earned between 1 and 4 minimum wages (56.73 %) (data not shown).
In the total sample, the mean BMI was 23.4 ± 3.6 kg/m²; mean WC, 86.3 ± 10.7 cm; and mean SAD, 18.7 ± 2.6 cm, with no significant differences between men and women (p > 0.05). Regarding the distribution of BF assessed using DEXA, there was a significant difference between the men and the women for both the android fat percentage (%AF) and gynoid fat percentage (%GF), with the women displaying the highest means (p < 0.0001) (Table I).
Table I. Descriptive, anthropometric, and body composition characteristics of patients on hemodialysis

BMI: body mass index; WC: waist circumference; SAD: sagittal abdominal diameter; AF: android fat; GF: gynoid fat.
The mean %BF measured using DEXA was 29.3 ± 9.3. The women had a higher mean %BF than the men (p < 0.001). In the comparison of the measurements among the three methods, there was a significant difference between the means of the total %BF evaluated using DEXA and SSKD measurement (p < 0.001), and between those evaluated using BIA and SSKD measurement (p < 0.001). In both sexes, a significant difference was observed among the three methods (p < 0.05) (Table II).
Table II. Total body fat of hemodialysis patients estimated by the SSKD, BIA and DEXA methods

SSKD: sum of four skinfolds; BIA: electrical bioimpedance; DEXA: dual-energy X-ray absorptiometry. *DEXA versus SSKD; †DEXA versus BIA.
Table III presents the CCC-L between the three methods used after stratification by sex. Although similar in terms of statistical significance (p < 0.001), SSKD measurement presented higher concordance coefficients than did BIA. Lower concordance coefficients were observed between SSKD measurement and BIA but were significant (p < 0.001).
Table III. Lin's concordance correlation coefficient between the SSKD, BIA, and DEXA methods by sex, in the estimation of total body fat (%) for patients on hemodialysis
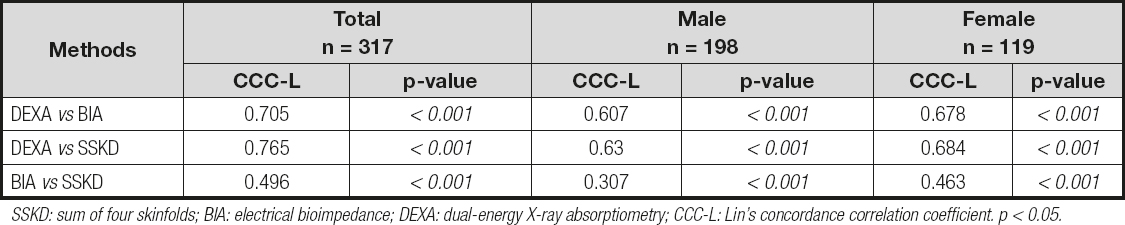
SSKD: sum of four skinfolds; BIA: electrical bioimpedance; DEXA: dual-energy X-ray absorptiometry; CCC-L: Lin's concordance correlation coefficient. p < 0.05.
Owing to the lack of cut-off points for the %BF specific to the population of patients with CKD receiving HD, we decided to organize the study sample in tertiles, stratifying them into low, median, and high %BF. There was a decrease in the CCC-L between the methods evaluated by tertiles. However, SSKD measurement presented a higher CCC-L with DEXA in the first tertile (8.2 % to 26.0 %, p < 0.001) and in the second tertile (26.1 % to 34.4 %, p < 0.001). Thereafter, BIA presented a higher concordance with DEXA in the third tertile (above 34.4 %, p < 0.001) (Table IV).
Table IV. Lin's concordance correlation coefficient between the PC, BIA and DEXA methods by tertiles, in the estimation of total body fat (%) for patients on hemodialysis

SSKD: sum of four skinfolds; BIA: electrical bioimpedance; DEXA: dual-energy X-ray absorptiometry; CCC-L: Lin's concordance correlation coefficient. p < 0.05.
DISCUSSION
This study aimed to analyze BIA and SSKD measurements in the evaluation of total %BF because both are simple and widely used methods.
Both BIA and SSKD measurements presented a significant concordance with the reference method DEXA, with better results for SS measurement.
SSKD measurement is widely used in clinical practice because it is a non-invasive and low-cost technique. Despite the divergences regarding its accuracy in states of hyperhydration and edema, and possible errors among evaluators, it has shown good results when compared to DEXA in the evaluation of BF in HD patients (10).
A probable explanation for the better performance of SSKD measurement in our study is the fact that it does not take water into account in the estimation of total %BF in its predictive equations (7,8). In addition, the measurements were performed by trained evaluators and after HD sessions to reduce the interference of water.
Conversely, BIA is a non-invasive, portable, and relatively inexpensive tool (11); however, its accuracy can be affected by the equipment used, food and water intake, physical activity, menstrual cycle, and alcohol consumption (12).
BIA primarily estimates total body water through derived vectors, and calculates BF assuming a hydration constant of 73 % of fat-free mass (FFM); therefore, the equations result in a greater margin of error in the measurement of BF, as the result depends on the estimation of body water and FFM, which may be overrated in hyperhydration states such as that commonly found in HD patients (13).
Furthermore, the conventional BIA approach involves the use of predictive equations that can produce inadequate estimates in HD patients because volume overload is a common complication in these patients, especially if associated with hypertension and hypertrophy of the left ventricle (14).
In agreement with our findings, the European Consensus on Nephrology emphasizes that, for a detailed assessment of nutritional status, anthropometric methods such as SSKD measurement are also useful, considering that they are inexpensive and easy to apply, despite being less accurate than DEXA (4). The newest update from the National Kidney Foundation (NKF-KDOQI) ratified the above-mentioned statement, recommending that in adults with CKD undergoing HD, and in the absence of edema, skinfold thickness measurements must be performed to evaluate BF (5).
Sánchez-Ramírez et al. (15) sought to evaluate the body composition assessment methods BIA and SSKD measurement in patients on dialysis treatment. They found high and significant correlations between BIA and SSKD measurement, with a stronger correlation for FFM evaluation. Nevertheless, as highlighted in the study, some variables, such as age, sex, and extracellular water, influenced different degrees of variability of body composition, regardless of the assessment method employed. Moreover, unlike in our study, a gold standard method was not used for comparison.
Eickemberg et al. (16) emphasized that the development of specific equations for the Brazilian population in different age groups should be prioritized, including patients with CKD, when assessing body composition using BIA.
In their comparison of SSKD measurement and BIA with the gold standard method DEXA in the estimation of the total %BF of patients undergoing HD, other authors also reported that SSKD measurement better estimates BF in these patients.
Rodrigues et al. (17) evaluated BF using the 4-frequency multi-frequency BIA method and found that BF was underestimated, both before and after HD, more significantly among women than among men. In addition, they found more accurate results with SSKD measurement before and after HD, which was similar with the gold standard method DEXA.
In their study comparing the amount of BF measured using SSKD evaluation and bioimpedance spectroscopy with that measured using DEXA as the reference method, Rymarz, Szamotulska, and Niemczyk (18) concluded that SSKD evaluation seems to be more reliable than BIA when assessing patients with CKD classified under stages 4 and 5. However, methods based on BIA techniques can potentially provide more data, including those in cases of hyperhydration.
Kamimura et al. (19) reported that BIA worked differently from DEXA when the findings were analyzed by sex, underestimating BF in men and overestimating such in women undergoing HD (p < 0.001); this corroborates our findings in which the mean %BF assessed using BIA was different from that assessed using DEXA in both women and men.
Interestingly, although both methods presented higher coefficients of concordance for women in our study, especially SSKD measurement, there was no significant concordance for any method considering the first tertile for this gender. In other words, for a %BF between 8.2 % and 26 %, no method presented a significant concordance with DEXA. Owing to the scarcity of studies on this topic and stratification in the HD population, this finding needs further investigation.
The lack of cutoff points and specific equations for the HD population was the limiting factor in our study. Nevertheless, the strengths of this study include the use of a gold standard method, i.e., DEXA, for the evaluation of %BF, and the fact that the study was conducted in five HD centers located in the capital city of Maranhão state.
Our findings provide important contributions to the evaluation of the body composition of HD patients by identifying a simple method, such as SSKD measurement, for use in clinical practice; these may then help with the development of low-cost and easily applicable strategies for nutritional assessment.
CONCLUSION
SSKD measurement was more concordant with the reference method, DEXA, as compared with BIA, possibly because it did not take into account the water component in the predictive equations for BF.
Thus, as our study used a gold standard method to evaluate the reproducibility of the methods, SSKD measurement may be used in clinical practice, considering its low cost and good accuracy in this population.
We emphasize the need for further research on this topic to elucidate issues often associated with the challenge of assessing body composition in HD patients.














