INTRODUCTION
The key of healthy eating seems to consist in choosing an appropriate and adequate amount of food from various food groups. A healthful diet is essential for both good health and nutritional status, and represents a key component of obesity prevention strategies. According to WHO, nearly over 340 million children and adolescents aged between 5 and 19 years were diagnosed with overweight or obesity in 2016 (1). In addition, the prevalence of overweight and obesity within these population groups has risen dramatically from 4 % in 1975 to over 18 % in 2016 (1). A large amount of evidence shows that the portion size (PS) of some foods, especially those consumed in restaurants, has increased dramatically over the last 30 years, along with the prevalence of obesity (2,3), a trend that started in the 1970s and persists nowadays. With a view to invert this situation, individuals need effective strategies to regulate their energy intake in spite of the widespread availability of highly palatable, energy-dense foods (4). Increased PS of commonly served foods is considered a major factor that has contributed to excessive energy consumption and, consequently, to the development of obesity (3,5). Obesity is considered the most common cause of insulin resistance in children (6), as well as of dyslipidemia (7) and type-2 diabetes (8). In the public health setting, research data about food intake, both in individuals and populations, serve as the basis for nutrition monitoring and food policies (5). In this narrative review we focus on the relation between food PS, total energy intake, obesity, and some metabolic syndrome features such as insulin resistance in children and adolescents.
SCOPE AND METHODOLOGY OF THIS REVIEW
The strategy for bibliographic search focused on articles published in the English language from 1952 to December 2019 (including online). The databases used included PubMed, Web of Knowledge, Scopus, Science Direct, and online books. In addition, citations in reviews and paths within databases were also incorporated. Key terms included: portion size, food size, food type, dietary estimation method, portion size estimation, food photography, food model, household measures, obesity, food choice, dietary intake, body mass index (BMI), energy-dense food, energy intake, emotional eating, insulin resistance, diabetes, children, adolescents, satiety, appetite, exposure, reward, model, and pressure to eat.
FOOD PORTIONS. DEFINITION AND ESTIMATION
A portion is defined as the amount of food that we choose to eat for a meal or snack, or the amount of a food that we decide to eat or serve to an individual on a single eating occasion (9). The size of a food portion can be identified as the weight or volume of household measures such as: tablespoons, hand measures, or size of a reference object (10). The concept of PS varies widely between countries, across different population groups, and according to both individual and environmental factors (10). For example, a PS may reflect a person's own choice, the choice of the food producer in a restaurant, or a recommendation by a health professional or the government. PS also reflects ways of eating—for instance, in some cultures the hand-based portion is used to self-serve or measure portions of foods for others (11).
Various methods are used to assess dietary intake, such as single or multiple 24-hour dietary recalls, estimated dietary records, diet history, and food frequency questionnaires. However, since these methods rely on an individual's memory, there is a certain challenge in determining food intake, especially in relation to accurate estimation of food PS. To estimate PS several options are available: directly weighing the amount of food consumed by the participant or estimating the size of food portions via visual comparisons to household measures, food models, or photographs.
Directly weighing food portions
Because foods have to be weighed before consumption, weighing methods for determining portion sizes can only be used with prospective dietary assessment methods and using properly calibrated scales (12). The weighing should be done by investigators or by participants. Although weighed food records are an accurate traditional dietary assessment method, it is time consuming, cumbersome for participants, and costly to implement.
Visual estimation of weights and size
Direct observation using visual estimation is a non-intrusive method of estimating food portions that provides an acceptable alternative (13). To apply this method, observers should be trained to estimate PS by monitoring the weights of foods consumed by participants. The accuracy of estimations may vary according to the type and quantity of food (14). Several studies revealed a good correlation between visual estimates and actual weight (14). Even so, observers may differ on their ability to estimate food weights visually, as they tend to overestimate the weight of the foods consumed and to underestimate plate wastes, which may result in potential bias when estimating sizes of foods with a high volume but low weight (13). Of note, a wide range of methods have been described to quantify outcomes related to PS in research studies, including surveillance and epidemiological analyses, clinical and nutritional studies, and research on eating behaviors (15). The most frequently used measurements are food models, photographs, and household measures (16).
Household measures
Even though some foods, like eggs, oranges, or soft drinks, can be recorded in units, other food items are often measured in volumes such as cups or tablespoons (16). These measures are familiar and easy to use. However, volume measures may produce considerable error and individual variability in estimating portion weights (17) because foods can be packed tightly or loosely, and certain foods, such as meats and pastries, do not conform to measuring devices (18). Household food measures have led to significant under- or over-estimations of actual portion weight (16). Cons0equently, household measures are not accurate for individuals, but they are still used to produce acceptable data for group estimations in epidemiological studies.
Food models
Food models are also known as fake food models; they are geometric shapes of food samples. Some studies found that having realistic models closer to real food is a better option for children (19). On the other hand, a systematic underreporting of intake was found when three-dimensional plastic food models were used to represent servings, and the magnitude of this underreporting varied across food items. In contrast, when larger-sized food models were used, participants tended to be more accurate in reporting their intake of foods (20,21).
Photographs
In studies that involve telephone recalls or self-administrated dietary surveys, two-dimensional pictures of food shapes were as effective as three-dimensional models in supporting participants to estimate PS (22). Food photographs of various PSs have been reported to be useful in some studies (23), but poor correlations to actual measurements were detected in others (24).
FACTORS AFFECTING FOOD PORTION SIZES ESTIMATIONS
Several studies have been conducted to examine the influence of some specific characteristics of foods, study subjects, and interviewers on the accuracy of PS estimations.
Food type
It is important to know which foods are more reliable to estimate the size of their portions. Significant errors have been reported for some foods such as cakes, salads, butter on toast (25), and amorphous foods such as spaghetti or apple sauce (26), as well as for fish, rice, steak, and cheese (20). However, some studies indicate no consistent association between size estimations and food type (27).
Food size
Some studies found greater difficulties in estimating PS as portion size increases (28). In addition, some investigators reported that large plates are harder to estimate (29), but others did not report any differences related to plate size (27).
Age
Previous studies suggested that children are not able to estimate PS very accurately, even when prompted with visual aids (30). In contrast, recent studies found that children can estimate food PS with an accuracy approaching that of adults (31). However, high-school and college students have also reported difficulties when estimating PS (32).
Gender
The influence of gender on PS estimation has been argumentative, even though some studies report that women are better estimators (12), others report minimal or no differences (20). These differences between genders may reflect a skill attributed to the greater experience of women in measuring food as a function of their reference system, or a biological response to the higher energy needs of men versus women (33).
RELATIONSHIP BETWEEN FOOD PORTION SIZE AND TOTAL ENERGY INTAKE
The consumption of large PSs, especially from high energy-dense foods, has been identified as a major cause of excessive total energy intake (34). Laboratory studies show that increasing PS leads to increased energy intake in adults (35-37), mostly for high energy-density (HED) foods (2,3,34), in children and adolescents over 3 years of age (38-42). This finding is called the "portion size effect" or portion size response. This association has been observed in both laboratory and free-living studies, binding the consumption of large PSs with increased energy intakes across a variety of foods, ages, and body weights (3,43). Interestingly, this impact has been observed with packaged snacks (35), energy-dense casseroles (36,40), unit foods like sandwiches (44) and beverages (45), and even with low energy-dense foods like fruits and vegetables. Additionally, the effect of PS has been also observed in restaurants and offices (46,47), even if participants were served unpalatable foods (48) or with manipulation of plate size (49). To systematically assess the effect of PS on energy intake, several studies were conducted (Table I). A study assessed four US nationally representative surveys from 1977 to 2006 for three age groups (2-6-, 7-12-, and 13-18-year-olds), and found that, in all age groups, larger PSs of pizza were linked with higher energy intakes at eating occasions, whereas in 7-12- and 13-18-year-olds higher energy intakes at meals correspond with larger PSs of sugar-sweetened beverages (SSBs), French fries, or salty snacks (38). In another study, when a PS of 250 or 500 g of a macaroni and cheese entrée was served at a dinner meal to children, the effects of the entrée's PS (p < 0.0001) and energy density (p < 0.0001) on energy intake were independent but promoted meal consumption (39). The same result was noticed with a large portion (p < 0.002), when serving three different sizes (small, medium, large) of macaroni and cheese to children at lunchtime (41). In the study by Fisher JO et al., when preschool-aged children doubled the PS of several entrées (breakfast, lunch, dinner) and a snack during a 24-h period, there was an increase in energy intake from those foods by 23 % (180 kcal) (p < 0.0001) (42). Consequently, these studies showed that the PS effect was strongly and consistently observed across food types, environmental conditions, and study populations.
FOOD PORTION SIZES AND EMOTIONAL EATING
There are several factors that affect food intake, including metabolic needs (50), emotional states, motivations, and self-regulatory processes (51). To maintain energy balance, cognitive control responds by reducing or increasing food intake in order to cope with stress and negative emotions (52,53). However, it seems likely that consumption of large food portions, with high energy density, facilitates the increase of energy intake (54). Some studies found that external factors and emotional states, and their scores for dietary curb, were significant predictors of food intake. They also found that subjects who scored high on dietary restraint or emotional disinhibition increased their food intake in the presence of larger PSs, which means that a negative or positive mood was significantly associated with greater food and calorie intake across groups (51). In children, a positive association was observed between emotional eating and the frequency of sweet and fatty food consumption, which may contribute to the development of overweight (55), even though the study did not quantify the PS of the consumed food. The relationship between emotional eating and dietary patterns, mainly PS, has not been examined in young children. More studies are needed to analyze the possible influence of emotional eating on food intake in response to dietary manipulations of food PS and energy density.
FOOD PORTION SIZES AND OBESITY, RELATED METABOLIC COMPLICATIONS
FOOD PORTION SIZES AND OBESITY
Although PS has been increasing over time, the effect on weight has not been clearly predictable. Several short-term controlled feeding trials, and epidemiological studies, assessed the association between food PS and body weight, as well as some adiposity indices, showing mixed findings.
In adults, several studies were performed. A midday meal manipulation with a four-week trial showed that larger portions were associated with a weight gain of 0.64 ± 1.16 kg, whereas this change in the standard portions group was 0.06 ± 1.03 kg (56); these weight changes were not significant over time or between test periods. Even so, Rippin et al. (57) found limited evidence on the association between the PS of energy dense foods and BMI in subgroups analyzed from the French and UK national dietary surveys. To assess body weight changes during PS manipulation, an intervention study observed a non-significant increase in body weight after providing a 50 % larger lunch for 1 month (56). However, possibly the PS effect was too small to result in weight change due to the small sample size of the study, and the fact that only one meal of the day was manipulated with controlled PS throughout the intervention period. In another short-term study, a significant increase in mean body weight, for men and women, was observed after larger portions were served on all eating occasions (58). However, these findings are based on cross-sectional analyses, and it still remains unclear whether the association between PS and obesity is causal or associative only. Meanwhile an effective weight loss was well documented with meal replacement products and portion-controlled entrées (59).
Several studies observed a positive relationship between increasing PS and obesity in children (60,61) and adolescents (9,62) (Table II). Fisher JO and Birch LL study on girls, aged between 5 and 7 years, found that those who ate large amounts of snack foods in the absence of hunger were 4.6 times more likely to be overweight (60). This was confirmed by another study conducted in children and adolescents, which found that PS and energy content per meal were significantly associated with BMI percentile in boys 6 to 11 years of age and in children 12 to 19 years of age. However, no relationships were found among children 3 to 5 years and girls 6 to 11 yearsof age (63). Another French study on children aged between 3 and 11 years, taken from the 1998-1999 cross-sectional study, observed that overweight in children aged 3 to 6 years was positively associated with the PS of biscuits (p = 0.0392) and sweetened pastries (p = 0.0027). Also significantly positive trends were observed for PSs of croissant-like pastries (p = 0.0568) and meat (p = 0.0574) (64). In UK adolescents, there was also a positive association between PS of biscuits and cakes and BMI (9).
Unfortunately, these studies cannot be taken as proof of causality in children, mainly because they are not reflecting their eating in a free-living context. Consequently, long-term studies are needed to determine the causal link between increasing PS and obesity. However, these studies concluded that reducing PS may be an effective tool for weight control.
FOOD PORTION SIZES, GLYCEMIC INDEX, AND INSULIN RESISTANCE
In 1981 the glycemic index (GI) concept was proposed by Jenkins and colleagues to describe the rate of carbohydrate absorption after a meal (65). GI is defined as ‘the area under the glucose response curve after consumption of 50 g of carbohydrates from a test food divided by the area under the curve after consumption of 50 g of carbohydrates from a control food, either white bread or glucose' (66). Food PS has a major effect on the glycemic index value because glycemic responses are related to carbohydrate load (65). The usefulness of glycemic load (GL) is based on the idea that a high GI food consumed in small portions would have the same effect on blood sugar as larger portions of a low GI food (66,67). Although the effect of PS on GI was mentioned from 1981, there are no experimental studies measuring the effect of PS on GI in children and adolescents.
Insulin resistance, impaired glucose tolerance, and type-2 diabetes are considered ominous public-health issues in all age groups (6,8). Studies found that childhood obesity causes hypertension, dyslipidemia, chronic inflammation, a tendency to increased blood clotting, endothelial dysfunction, and hyperinsulinemia (7,68-70). The clustering of cardiovascular disease risk factors, known as the insulin resistance syndrome, has been identified in pre-pubertal children (71).
Insulin resistance is a key component of the metabolic syndrome, in turn a cluster of cardiometabolic factors with increasing prevalence in children and adolescents, and associated with obesity (72,73). The relationship between metabolic syndrome and diet among children and adolescents remains poorly understood. In adults, studies have shown that dietary patterns characterized by high intakes of fruits and vegetables are generally associated with a lower prevalence of the metabolic syndrome (74,75). Although the development of obesity in genetically stable populations has been increasing (8), studies examining insulin resistance, metabolic syndrome, and their association with diet, especially PS in children and adolescents, are still scarce. It is still unknown whether individual dietary components, or overall diet can independently affect metabolic syndrome in this age group.
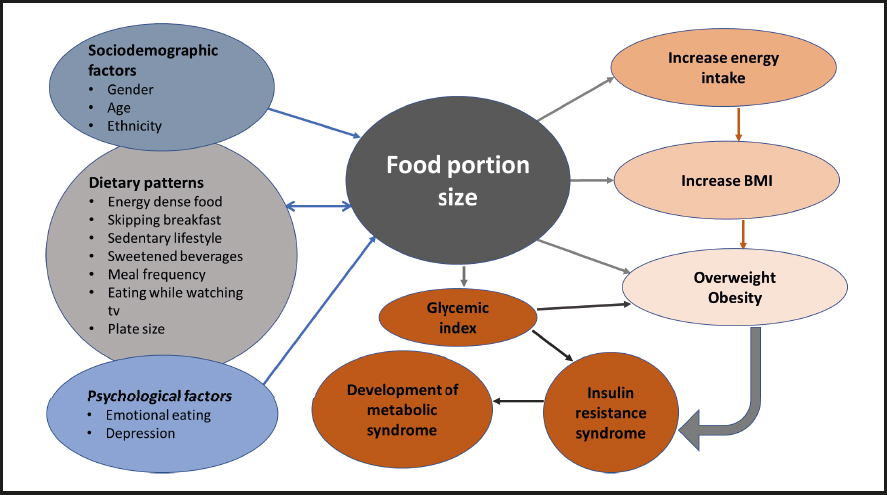
The flow diagram of the underlying factors affected by PS are found in figure 1. High PS is related to obesity and other metabolic complications, whereas many factors such as sociodemographic parameters (gender, age), dietary patterns including energy-dense food, skipping breakfast, and sedentary lifestyle, alongside with psychological factors like emotional eating, were found to have a direct effect on the consumption of large food PSs. As illustrated in figure 1, there is an interchangeable relation between dietary patterns and food PS. For example, the consumption of energy-dense foods was linked with large PSs and vice versa. Furthermore, once a larger portion is chosen, energy intake and—consequently—BMI will increase. Similarly, high food PSs increase glycemic index levels, thus contributing to both insulin resistance and metabolic syndrome. Of note, increasing energy intake could cause an increase in BMI and the development of overweight and obesity, which in turn could contribute to insulin resistance and metabolic syndrome.
CONCLUSION
Food and drink PS has been increasing in recent years. However, it has not been possible to establish a direct causal link between large food PS, especially in the case of energy-dense foods, and obesity as well as certain metabolic syndrome features. To date there are no long-term, randomized, controlled trials to assess the exposure to large portions of food and its effects on body weight. Clearly, there is an urgent need to develop a well-articulated research framework that systematically tests the interaction between selection of food PS and development of obesity, insulin resistance, and metabolic syndrome in both children and adolescents.