BACKGROUND
Over 109 million patients worldwide have been affected by Coronavirus Disease 2019 (COVID-19), caused by the SARS-COV-2 virus (1). Studies have shown that approximately 30 % of hospitalized patients require admission to intensive care units (ICUs) and ventilatory support (2).
In Latin American countries, 40-60 % of patients are malnourished at the time of hospital admission (3). This condition seems to impair immune response (4) with increased susceptibility to infection (5,6), which may have a deleterious impact on length of stay, days on mechanical ventilation, and in-hospital mortality (7).
Nutrition screening is defined as the process that allows identifying individuals who are at nutritional risk or already malnourished who would benefit from early nutritional support in order to predict and prevent adverse clinical outcomes. For this purpose, multiple nutritional screening tools have been validated in different clinical settings. However, all of them must be practical, reliable, and quickly appliable in the first 24-48 hours of hospital admission (7).
NUTRIC-Score was the first designed and standardized tool for use in critically ill patients. The original score was modified by excluding IL-6, because of high-cost measurement and low availability in the clinical setting. Global results showed a positive association between nutritional provision and survival at 28 days in patients with a higher NUTRIC-Score. Furthermore, this score is useful to identify the critically ill patients who will benefit most from optimal nutritional support (8).
During the COVID-19 pandemic, some authors have reported an increased prevalence of high nutritional risk in critically and non-critically ill patients from China when using nutrition screening tools such as NRS-2002 and NUTRIC-Score. Nutritional risk as identified by these tools has been associated with higher mortality and longer hospital stay in COVID-19 patients; however, there are no previous reports of associations between nutritional risk and clinical outcomes in Latin-American countries (9-11).
The aim of this study was to describe the association between nutritional risk and length of stay, days on mechanical ventilation, and in-hospital mortality in patients infected with SARS-CoV-2.
METHODS
In a retrospective cohort study, critically ill patients over 18 years of age, with a documented diagnosis of COVID-19, requiring mechanical ventilation from March 1, 2020 to June 30, 2020 at the National Institute of Respiratory Diseases were included. This center is a tertiary respiratory-disease exclusive hospital in Mexico City, Mexico.
ETHICAL CONSIDERATIONS
This study was reviewed and approved by the Institutional Review Board of the National Institute of Respiratory Diseases (Register #C51-20).
DATA COLLECTION
Demographic data included sex, age, height, weight, and body mass index (BMI). Prescribed drugs with nutritional implications (steroids, benzodiazepines, opioids, neuromuscular blocking agents [NBA], sedatives, peripheral nerve blockers, insulin regimens, and vasopressors), as well as PaO2/FiO2 ratio, medical history of non-communicable diseases, and biochemical parameters (acid-base status, electrolytes, glucose, and lipid levels) during the first 24-48 h of mechanical ventilation were collected.
NUTRITIONAL RISK ASSESSMENT
The nutritional risk of each patient was calculated using a modified NUTRIC-Score that includes age, APACHE II, and SOFA scores at admission, number of comorbidities and pre-ICU hospital length of stay during the first 48 hours of mechanical ventilation. High nutritional risk was stablished with a score ≥ 5.
CLINICAL ENDPOINTS
The main endpoint was the number of days under mechanical ventilation. Secondary endpoints included hospital length of stay (LOS) in-hospital mortality and 28-day mortality.
STATISTICAL ANALYSIS
Categorical variables were expressed as frequency rates (%), and continuous variables were expressed as means and standard deviation or median and interquartile range (IQR) values (P25-P75). Means for continuous variables were compared using independent group t-test when data were normally distributed between severe and critically ill groups, or using the Mann-Whitney U-test otherwise. Proportions for categorical variables were compared using the χ² test between two groups. Logistic regression models and linear regression models were used to analyze the association between NUTRIC-Score (treated as a categorical variable) and clinical outcomes (ventilator days, length of stay, and in-hospital mortality) after sex adjustment. Survival at 28 days was assessed using Kaplan-Meier curves with log-rank test, and a Cox proportional hazards model. The statistical analysis was performed using the packages Stata Intercooled (Version 14, STATA Corporation, College Station, TX, USA) and GraphPad Prism (GraphPad Software Inc., San Diego, USA). Statistical significance was defined as p < 0.05.
RESULTS
A total of 112 patients on mechanical ventilation were included in the analysis. The demographic characteristics and clinical features of patients are listed in table I. Average age was 56.1 ± 12.6 years, and 34.8 % of the sample was over 60 years. There was a male predominance overall (71.4 %), and the mean age of females (60.7 ± 13.5 years) was higher than that of males (54.3 ± 11.9 years; p = 0.01). The average BMI of patients was 30.1 ± 5 kg/m2; 39.3 % were overweight and 47.3 % were obese. The most common comorbidities were hypertension (n = 31, 27.6 %) and diabetes (n = 38, 34 %). Based on NUTRIC-Score, 74 (66 %) were at high nutritional risk and 38 (34 %) were at low nutritional risk. The mean APACHE II and SOFA scores were 21 ± 5 and 9 ± 2, respectively. Any degree of acute kidney injury was diagnosed in 45.5 % of patients.
Table I. Demographics, clinical, and nutritional characteristics of COVID-19 critically ill patients at the onset of mechanical ventilation

OUTCOMES ASSOCIATED TO NUTRITIONAL RISK
In- hospital mortality was 48.2 % in the whole sample. Patients with high nutritional risk had higher mortality than low-risk patients (p = 0.03). The average LOS was 25 days (IQR, 16-41), and the duration of mechanical ventilation (MV) was 17 days (IQR, 9-27) in discharged patients (Table II)
Table II. Clinical outcomes of COVID-19 critically ill patients by nutritional risk
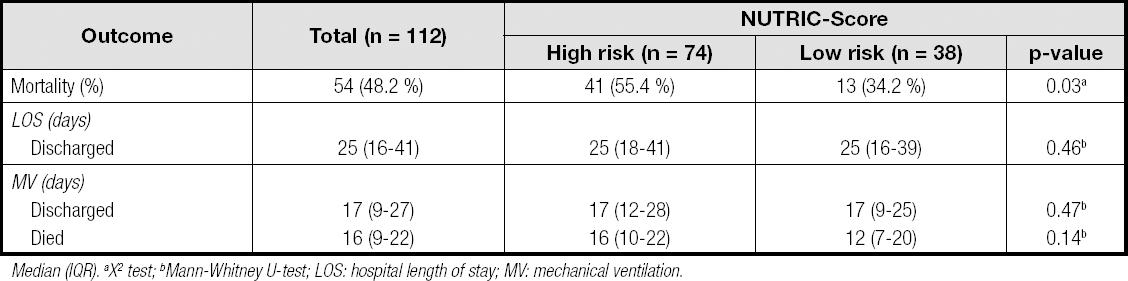
Median (IQR). aX2 test; bMann-Whitney U-test; LOS: hospital length of stay; MV: mechanical ventilation.
In logistic regression models, high nutritional risk was associated with increased mortality risk (OR: 2.38, 95 % CI, 1.06-5.38, p = 0.036). No associations for hospital length of stay and ventilation days were observed (Table III).
TWENTY-EIGHT-DAY MORTALITY RISK
A survival analysis at 28 days was performed. A total of 73 patients had been discharged or had died on day 28 (48 with high nutritional risk and 25 with low nutritional risk). The number of patients who died on the first 28 days was 33 in the high nutrition risk group and 11 in the low nutrition risk group. Differences (p = 0.04) were observed with a higher 28-day mortality in the group at high nutritional risk (Fig. 1). In the Cox model adjusted for sex the high nutritional risk group was associated with a higher 28-day mortality (HR: 2.05, 95 % CI: 1.01-4.23, p = 0.04) when compared to the low risk group.
DISCUSSION
This study is the first one to describe an association between nutritional risk and clinical outcomes in Latin-American critically ill patients with COVID-19. Patients affected by this pandemic disease are at nutritional risk. According to Liu et al., nutritional risk is present in 85.8 % of non-critically ill patients (11). In critically ill COVID-19 patients, Zhang et al. reported a prevalence of high nutritional risk in 61 % of the patients in a retrospective study with data from three ICUs in Wuhan, China (n = 136). In our study, we found that 66 % of critically ill COVID-19 patients were at high nutritional risk according to NUTRIC-Score calculations at ICU admission, which is similar to the findings by Zhang et al.
Additionally, patients in the study by Zhang et al. were predominantly elderly, with 63 % of participants being older than 65 years of age, in comparison with only 34.8 % of patients in our sample being over the age of 60 years. Hypertension and diabetes were the most commonly reported comorbidities in both studies. The prevalences of hypertension and diabetes were 50 % and 41 %, respectively, in the study by Zhang et al., in comparison with prevalences of 27.6 % and 34 %, respectively, in our study. Hemodynamic instability with vasopressor requirements and acute kidney injury (AKI) were present in 51.3 % and 45.5 %, respectively, of the participants in our study, which does not differ from the 66 % and 41 % reported by Zhang et al. Older age, multiple comorbidities, and disease severity contribute to increased nutritional risk detection using tools such as NUTRIC-Score.
Higher nutritional risk was associated with adverse clinical outcomes in similar patients. Zhao et al. demonstrated in critically ill patients with COVID-19 that higher nutritional risk (using the NRS score) was associated with a higher risk of mortality (OR: 2.23, 95 % CI, 1.10-4.51, p = 0.026); they also did not observe any association between nutritional risk and LOS (9). Using NUTRIC-Score in 136 critically ill COVID-19 patients, Zhang et al. reported a higher mortality in the high nutritional risk group (HR: 2.01, 95 % CI, 1.22-3.32, p = 0.006) (10). In our sample, high nutritional risk was associated with mortality risk (OR: 2.4, 95 % CI, 1.05-5.47, p = 0.046); however, we observed a high prevalence of overweight and obesity in this sample, which may have influenced the association.
Our study has some limitations. First, all data were obtained from a single center, which may result in concerns regarding the generalization of our conclusions. Second, we only assessed critically ill patients. Third, long-term survival outcomes were not accessible due to the impact of COVID-19 on the workload of the nutrition department. More studies are needed to elucidate the impact of nutritional therapy on nutritional status, infection course, and clinical outcomes.
















