INTRODUCTION
Several studies have investigated malnutrition (1-3) in the hospital setting, showing the impact of nutritional risk (2) on clinical outcome and hospital costs. Some investigations (3) have evaluated factors associated with malnutrition, pointing out the need for greater attention to nutritional care. Correia et al, in 2017 (1), showed that most studies describe a high prevalence of malnutrition, with rates ranging from 40 % to 60 %. The authors reported an increase in malnutrition associated with increased length of hospital stay, and with clinical and infectious complications. Thus, several nutritional indicators (4,5) have been used to assess nutritional status. Some (6) show that in individuals identified by risk screening as being at nutritional risk, the diagnosis of malnutrition should be based on low body mass index or on combined weight loss indexes together with other indicators (6).
Nutritional intervention has contributed to reduce the risk of death and rehospitalization due to complications arising from poor nutritional status (7). In a prospective study (8), the priority of identifying nutritional status by means of nutritional screening instruments in clinical practice, in order to reduce morbidity and mortality rates (8), has been demonstrated. Other investigations have evidenced the importance of nutritional intervention with the use of specific supplements adapted to different clinical conditions (9). Another study (10) investigating nutritional status showed an association with age, nutritional therapy, and food intake, which were related to clinical outcomes such as prolonged hospital stay.
Within this context, hospital weight loss, food consumption, and type of nutritional therapy (10-12) have been investigated in the relevant literature, and have motivated the performance of this study. Thus, the aim of this study was to assess weight loss, the diet prescribed to, and the nutritional status of hospitalized patients and their associated factors.
METHODS
STUDY DESIGN, ETHICAL APPROVAL AND POPULATION CHARACTERISTICS
This was a retrospective study with data collected from medical records at a university hospital, conducted between the years 2018 and 2019. The study was approved by the institution's Research and Ethics Committee. The inclusion criteria adopted were age equal to or greater than 20 years, investigation of nutritional status within 48 hours of hospitalization, and complete nutritional information in the hospital medical records. Patients with incomplete records, terminal illness, and hospitalized only for clinical investigation and/or exams were excluded.
It is worth mentioning that in this hospital department a routine nutritional status assessment is carried out at the very beginning of hospitalization, at most within two days of admission. This procedure is routinely performed in hospital clinical practice by a team of nutritionists, residents and interns trained in nutrition at this institution, who assessed the nutritional indicators of anthropometry, used laboratory tests, administered nutritional screening instruments, and reviewed food histories. These data are routinely recorded in the medical records of inpatients.
For the composition of the sample to be studied in this investigation, all patients admitted to surgery services who met all inclusion criteria in the period defined for the study were selected. Initially 673 patients were recruited for this study, but 52 of them did not meet all the inclusion criteria. Thus, 621 adult inpatients of both genders were considered eligible for the study.
METHODOLOGICAL PROCEDURES
Data concerning type of disease, length of stay, age, gender, recent weight loss, weight loss during hospitalization, subjective global assessment, nutritional risk screening, anthropometry, type of diet prescribed on admission, alteration and acceptance of diet, use of protein-calorie supplementation during hospitalization, and percentage of habitual energy intake in relation to the estimated energy requirements (%HEI/EER) are described below.
Recent weight loss (RWL)
RWL was considered unintentional when the patient reported having lost > 5 % of their weight within the last 3 months, prior to hospitalization (6).
Weight loss during hospitalization
In order to assess weight loss during the hospitalization period, the present study considered the loss of at least 1 kg of weight from admission (1st day of hospitalization) to hospital discharge (last day of hospitalization). This criterion was established by the study authors to take into account in-hospital weight loss.
Subjective global assessment (SGA)
Nutritional status was assessed by the SGA and was classified according to standard cutoff points (13) into well nourished and malnourished (in this study, patients classified as mildly, moderately, and severely malnourished were all considered malnourished).
Nutritional risk screening (NRS)
Nutritional risk was assessed using the NRS tool, classifying patients as with a score ≥ 3 (at risk) or < 3 (without risk) (14,15).
Anthropometry
Body mass index (BMI) was evaluated according to standard cutoff points for adults (16) and the elderly (17), and body composition parameters such as arm circumference (AC), triceps skinfold (TSF), and arm muscle circumference (AMC) (18,19).
Type of diet prescribed at admission, diet change, diet acceptance, and use of protein-calorie supplementation during hospitalization
The type of diet prescribed during hospitalization was evaluated and classified as general diet (with solid food), soft diet (with soft food), liquid diet (with liquid food), watery diet (water, tea and gelatin; this diet was used during short post-operative periods), enteral and parenteral diet, or fasting (oral fasting). We investigated whether there was any change or alteration (yes/no) in the diet prescribed during hospitalization. For the evaluation of diet acceptance, acceptance was considered to be good when the patient reported consuming the totality of the diet offered; to be regular when the patient reported partial acceptance of the diet (not eating the entire diet offered); and to be poor when the patient had a low dietary intake. The use or not of calorie-protein nutritional supplements in liquid form (yes/no) during hospitalization was also surveyed.
Rate of habitual energy intake in relation to estimated energy requirements (%HEI/EER)
By nutritional anamnesis, the habitual energy intake of the week prior to hospitalization was evaluated through an individualized assessment of all patients, investigating their usual diet (recall of habitual consumption) and type and quantity of food, fractioning, and meal times. This allowed to calculate total energy consumption in relation to estimated energy requirements using the Harris & Benedict equation (20). Subsequently, the rate of energy intake in relation to energy requirements was considered in this study as being: < 75 % or ≥ 75 % (15,21,22).
STATISTICAL ANALYSIS
Initially, a descriptive analysis of the data was performed with the presentation of frequency tables for categorical variables and measures of position and dispersion for continuous variables. Then, for comparison of proportions, a Chi-square test or Fisher's exact test was used when necessary. To compare continuous or orderable measurements between 2 groups, the Mann-Whitney test was applied; and to do so between 3 or more groups, the Kruskal-Wallis test, followed by Dunn's test to find the differences, when necessary, was used. Subsequently, a logistic regression analysis was used to identify factors associated with weight loss during hospitalization. The power of the study was calculated for the results of logistic regressions. Power ranged from 0.70 to > 0.90. For the subjective global assessment (SGA) tool, power was 0.70 (70 % power), and for the other variables it was > 0.90 (> 90 %). The level of significance adopted for the statistical tests was 5 % (23-25).
RESULTS
The average age of the population studied was 57.85 ± 15.23 years, and the length of hospital stay was 10.80 ± 8.91 days. The general characteristics of the population are described in table I.
Table I. General characteristics of the studied population (n = 621 patients)
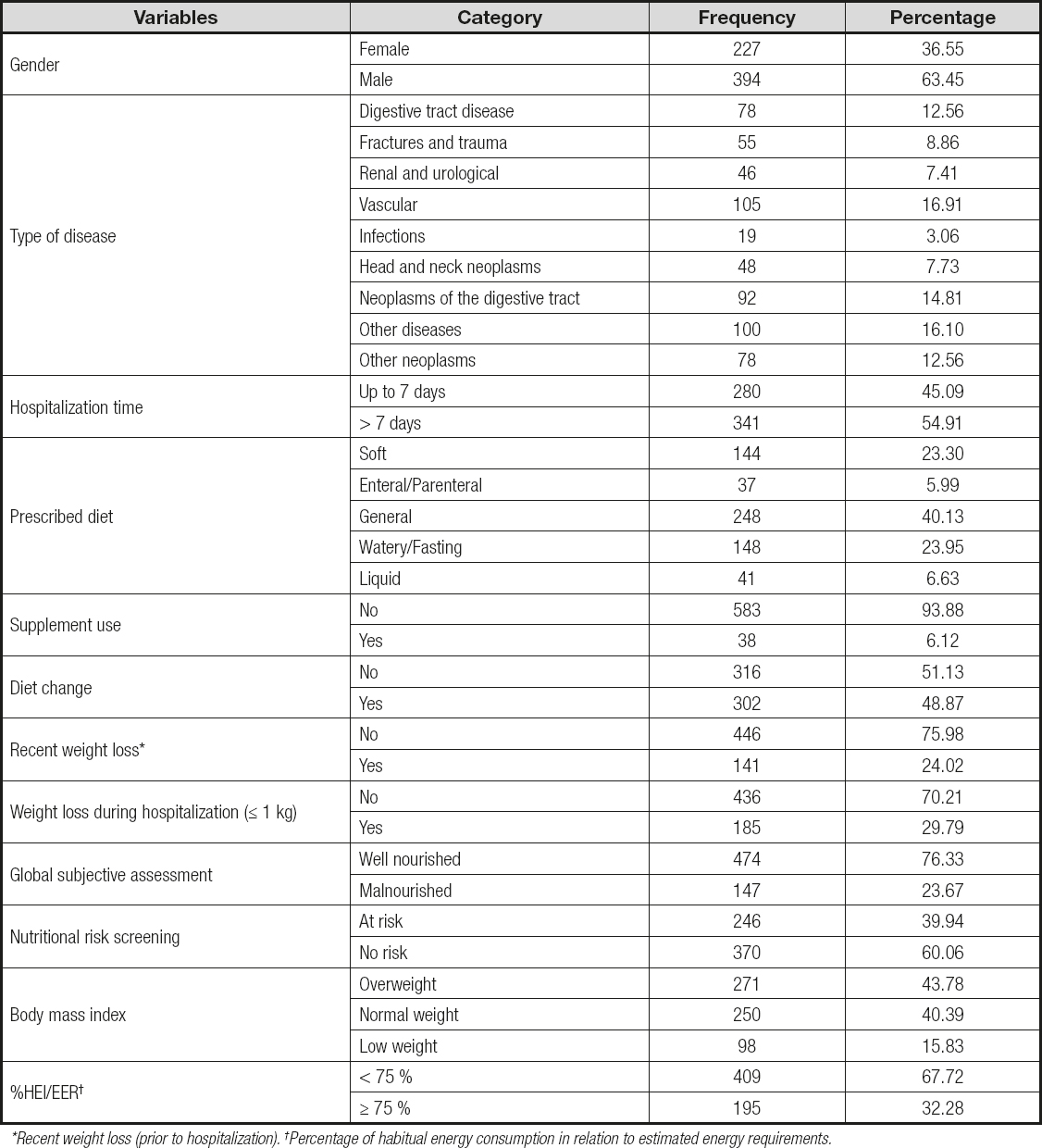
*Recent weight loss (prior to hospitalization). †Percentage of habitual energy consumption in relation to estimated energy requirements.
When comparing the groups of patients with and without weight loss during hospitalization, there was a significant difference for length of stay (p < 0.0001), fasting time (p = 0.0002), SGA (p = 0.0351), and type of disease (p = 0.0171). In the study of factors associated with weight loss by logistic regression analysis, it was found that patients who experienced weight loss during hospitalization were associated with a longer hospital stay (p < 0.0001; OR = 1.052; 95 % CI = 1.030; 1.073), malnourishment by SGA (p = 0.0358; OR = 1.520; 95 % CI = 1.028; 2.248), digestive tract diseases (DTD) (p = 0.0081; OR = 3.177; 95 % CI = 1.351; 7.469), and digestive neoplasms (p = 0.0407; OR = 2.410; 95 % CI = 1.038; 5.597) (Table IIA). The other variables studied did not show a statistically significant difference (Tables IIA and IIB).
Table IIA. Descriptive analysis of the variables studied and factors associated or not with weight loss during hospitalization (weight loss of at least 1 kg during hospitalization)
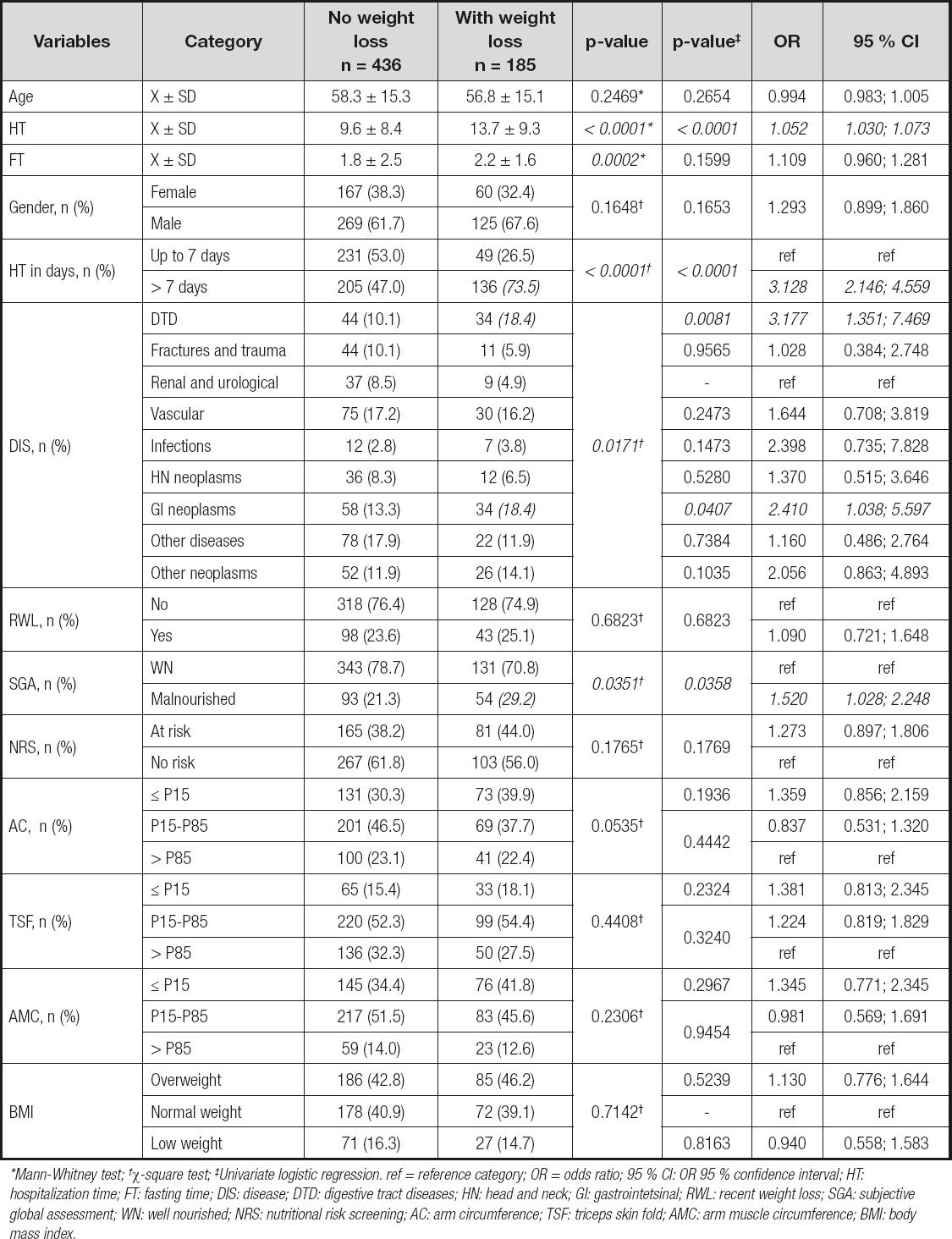
*Mann-Whitney test; †χ-square test; ‡Univariate logistic regression. ref = reference category; OR = odds ratio; 95 % CI: OR 95 % confidence interval; HT: hospitalization time; FT: fasting time; DIS: disease; DTD: digestive tract diseases; HN: head and neck; GI: gastrointetsinal; RWL: recent weight loss; SGA: subjective global assessment; WN: well nourished; NRS: nutritional risk screening; AC: arm circumference; TSF: triceps skin fold; AMC: arm muscle circumference; BMI: body mass index.
Table IIB. Descriptive analysis of the variables studied and factors associated or not with weight loss during hospitalization (weight loss of at least 1 kg during hospitalization)
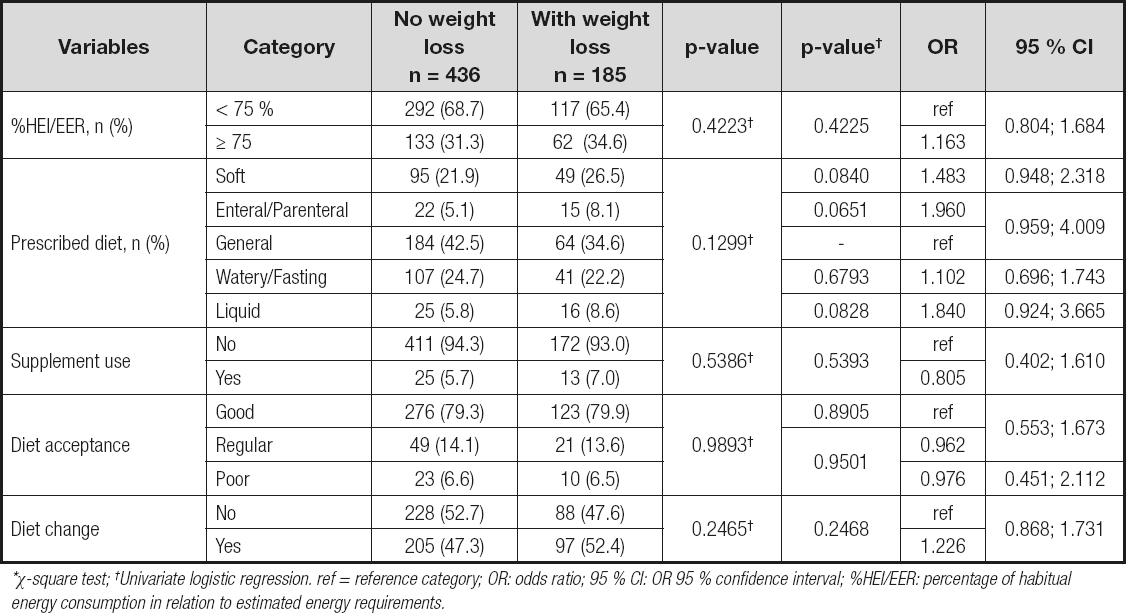
*χ-square test; †Univariate logistic regression. ref = reference category; OR: odds ratio; 95 % CI: OR 95 % confidence interval; %HEI/EER: percentage of habitual energy consumption in relation to estimated energy requirements.
Table III shows a comparison between the types of diet prescribed during hospitalization and study variables. There was a statistically significant difference in the relationship between all study variables and type of diet prescribed during hospitalization. There was a significant difference between types of diet according to malnutrition classification by SGA, with a higher percentage of enteral and parenteral diet (p < 0.0001; chi-square test). There was a significant difference between types of diet according to type of disease (p < 0.0001; Fisher's test). It was found that patients with digestive tract disease were prescribed fasting, water, and liquid diet with greater frequency. In cases of head and neck neoplasms and digestive tract neoplasms, a higher percentage of enteral and parenteral diets was observed (Table III).
Table III. Comparison of study variables by types of prescribed diet

*Kruskal-Wallis test; †χ-square test; ‡Fisher's exact test; ¦Differences between soft and general diets; soft and liquid. GD: general diet; SD: soft diet; LD: liquid diet; WDF: watery diet and fasting; EPD: enteral and parenteral diet; F: female; M: male; DTD: digestive tract disease; HN: head and neck; DT: digestive tract; Dis: diseases; RWL: recent weight loss; SGA: subjective global assessment; WN: well nourished; M: malnourished; NRS: nutritional risk screening; AC: arm circumference; TSF: triceps skin fold; AMC: arm muscle circumference; BMI: body mass index.
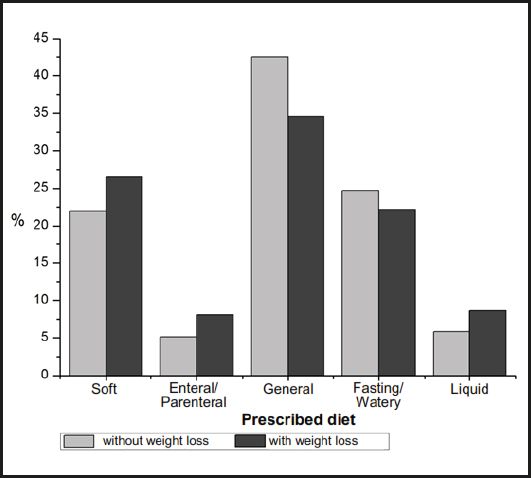
Figure 1 shows the percentage distribution of the type of diet prescribed during hospitalization, according to weight loss (loss, or no loss, of at least 1 kg of weight during hospitalization). There was no statistically significant difference between patients who presented or did not present weight loss during hospitalization and the types of diets prescribed (p = 0.1299; chi-square test).
DISCUSSION
This investigation showed that patients who were hospitalized for a period longer than 7 days had a three-fold greater risk of experiencing weight loss. Those who were malnourished according to the SGA had a 1.5 times greater risk. Patients diagnosed with digestive tract diseases were 3.2 times more likely to experience weight loss when compared to those with kidney and urological diseases. And patients with digestive neoplasms had a 2.4 times greater risk of presenting weight loss when compared to patients with renal and urological diseases.
A few recent studies have shown data similar to the findings of our study, such as the study by Takaoka et al. in 2017 (26); they investigated nutritional status during hospitalization using nutritional tracking instruments and laboratory exams. The authors showed that increase in hospital stay was associated with several nutritional indicators such as SGA, NRS-2002, serum albumin, and weight loss, among others (26). Another study performed by Orlandoni et al. in 2017 (27) pointed out that malnutrition was an independent predictor of length of hospital stay and mortality, and that malnourished patients were hospitalized for almost three more days, compared with non-malnourished patients. The authors also showed that risk of death during hospitalization was 55 % higher in malnourished patients (27). Different findings were observed in the study by Cano-Torres et al., also in 2017 (28), where nutritional intervention and dietary advice contributed to a reduction in length of hospital stay but not in mortality among hospitalized malnourished patients. Other findings report that hospitalized patients may suffer from inadequate nutritional therapy, and the risk of developing malnutrition may increase during hospitalization (29).
A prospective study (30) that evaluated changes in nutritional status during hospitalization in Canada investigated SGA and body weight measurements during hospital stay and at discharge. Using multivariate analysis models, the authors showed that the decline in nutritional status according to SGA and weight loss ≥ 5 % were significantly associated with a longer hospital stay (30).
In an observational study conducted by Rattray et al. in 2017 (31), the nutritional adequacy of the diets prescribed and consumed by inpatients was assessed, and both supply and intake were considered adequate when they met ≥ 75 % of their estimated needs. In the study in question (31), it was observed that the average amount of energy and protein supplied to and consumed by the patients was significantly lower than the estimated average needs. The authors also observed that patients on liquid oral diets had a lower energy intake, showing that inpatients on liquid oral diets could develop a higher risk of malnutrition (31).
In our study, no association was observed between the type of diet that was prescribed on admission and the weight loss that occurred during hospital stay (p = 0.1299) (Fig. 1). Thus, we can suggest that further investigations should be carried out of hospital diets in order to better meet the energy and nutritional needs of hospitalized patients, contributing to a reduction in weight loss and hospital malnutrition. In a recent retrospective study (32) investigating the relationship between weight changes, diet, and dietary intake changes in patients with cancer, the authors found a significant positive correlation between dietary energy or protein consumption and weight change. Another finding of the study (32) was a correlation between anorexia and weight loss; but the authors found no similar correlation between changes in dietary intake and changes in weight (32). The study also pointed out that patients with advanced cancer and weight loss could be consuming diets insufficient to maintain body weight (32). In any case, it is essential to monitor dietary consumption and the evolution of body weight throughout hospitalization. A prospective observational study (33) that investigated the clinical characteristics and long-term results of unintentional weight loss in outpatients, showed the relevance of monitoring long-term clinical evolution in patients with unexplained weight loss (33).
And in a prospective study in a Brazilian hospital (34), factors related to the reduction of prescribed enteral therapy were investigated, showing that operational problems, gastric stasis, and accidental loss of the gastric tube, among others, were the main reasons for inadequate food intake.
The findings of the present study are interesting and can easily illustrate clinical scenarios for several underlying conditions. Our findings also point out the importance of investigating weight loss, of assessing type of diet and food consumption, and of daily, continuous monitoring of the nutritional aspects of hospitalized patients. Some works are in line with the proposal of our investigation, such as a cross-sectional study (35) to investigate the tracking of malnutrition through anthropometric and laboratory indicators in patients admitted to medical wards. The authors observed a longer hospital stay in malnourished patients, evidencing that malnutrition was more common among patients with malignancies (35).
It is important to note that the variables and/or all nutritional indicators investigated in the present study are currently instruments in use for the nutritional assessment and monitoring of hospitalized patients, and have been used in other investigations reported in the relevant literature. This is the case of a study that assessed the prevalence of malnutrition (29) and determined the daily caloric intake of hospitalized patients. The nutritional risk found by the NRS was 44.6 % (29), an index similar to that found in the present investigation, where we verified a 39.9 % rate of nutritional risk. As for malnutrition by SGA, the authors found a 53.6 % rate of malnutrition (29) while in our study it was 23.6 %. Possibly, the malnutrition found here by the SGA may have been underestimated in relation to the nutritional risk obtained by the NRS.
Finally, in the present study it was observed that all the variables studied showed a significant association with the type of diet prescribed at hospital admission (Table III). Although no direct relationship was found between diet and weight loss during hospital stay (Table IIB), due to the fact that we found these differences in relation to the type of diet prescribed, we can suggest that "indirectly" there is an association of weight loss during hospitalization with the prescribed diet. The diet prescribed was not directly related to weight loss but through the factors that are associated with diet prescription (in these factors there was a significant difference).
CONCLUSION
Malnutrition, diseases, digestive neoplasms, and length of stay were associated with weight loss during hospitalization. The findings of this study highlight the relevance of nutritional and dietary monitoring of hospitalized patients.
STUDY LIMITATIONS
This study had some limitations inherent to the type of retrospective study, in relation to other prospective and controlled studies, with loss of some nutritional variable data. That is why there was less information for some of the nutritional variables analyzed when compared to others. On the other hand, retrospective studies have the advantage that all the nutritional parameters that were evaluated reflected the actual conditions of routine hospital care, as it actually happens in daily hospital clinical practice, and not in a controlled manner, which could make the outcome artificial.












 Curriculum ScienTI
Curriculum ScienTI