INTRODUCTION
Vitamin D deficiency is an epidemic worldwide, turning into a major public health concern even in developed countries with sufficient sunshine and enough food availability (1-3). About 1 billion people worldwide suffer from this condition, while 30-50 % of the general population has vitamin D insufficiency (4-6). Although vitamin D is naturally present in a few foods, it is added to others, and consumed as a supplement, most of the requirements of vitamin D are covered by its synthesis through skin exposure to ultraviolet-B (UVB) radiation in sunlight (80-100 %) (4,7). So far, the best marker of vitamin D status is circulating 25-hidroxyvitamin D (25(OH)D) concentration, though no consensus exists on optimal serum 25(OH)D levels and the threshold for defining vitamin D insufficiency is a controversial subject (3,8).
Vitamin D is a prohormone indispensable for appropriate functioning in the human body. It is classically implicated in the regulation of calcium homeostasis and healthy bone growth, so its deficiency could cause several diseases during life (4). While, in children, vitamin D deficiency increases the risk of developing rickets and muscle-skeletal disruption, in adults is associated with osteomalacia, osteopenia, and osteoporosis, increasing the risk of fractures and falls (4,9). However, these clinically overt manifestations are only “the top of the vitamin D deficiency iceberg” (10,11). Nowadays, it is clear that vitamin D is also involved in a multitude of complex metabolic pathways with potential extraskeletal functions, and because of this, vitamin D deficiency may play other roles in a number of diseases (12). In fact, emerging research supports the possible role of vitamin D against cancer, infection, autoimmune disease, depression, diabetes, and poor outcomes in cardiovascular health (4,13-16). Although convincing, this evidence does not prove causality but supports a hypothesis for further study.
Vitamin D inadequacy not only is frequently observed in vulnerable populations with low consumption of vitamin D food sources and short exposure to sunlight (6), but also children and younger and middle-aged adults, postmenopausal women, and the elderly are at equally high risk for insufficiency worldwide (1,2,6). This state of vitamin D hypovitaminosis is replicated in Spain, a region of southern Europe. Previous studies conducted in Spanish populations have observed that vitamin D intakes are lower than recommended (17,18). In addition, available data from a recent review of vitamin D status in Spain suggest the presence of widespread vitamin D deficiency and/or insufficiency in several population groups of all ages (19) (children (24.3 %) (20), young individuals (61 %) (21), primary health care users (87 %) (22), pregnant women (50.2 %) (23), postmenopausal osteoporotic women (44 %) (24), the elderly whether in the community (79-80 %) or institutionalized (91 %) (25,26)), ranging from 24.3 % to 91 %. Probably this wide variation in prevalence rates across studies partly relates to individual differences in the study population such as age or pre-existing risk factors, together with geographical and seasonal variances, and the 25(OH)D cutoff used to define vitamin D inadequacy.
Nonetheless, in Spain, despite being a country with many hours of sunlight, it seems that vitamin D deficiency has been on the rise. To our knowledge, studies on this matter conducted in La Rioja population are still lacking. Thus, we aimed to describe the prevalence of vitamin D deficiency and insufficiency in at-risk patients attending primary healthcare facilities in La Rioja, a northern Spanish region, according to age, gender, and seasonal variations. In addition, we also examined the prevalence of hypovitaminosis D considering 2 cutoff 25(OH)D levels available in the literature.
MATERIAL AND METHODS
STUDY DESIGN AND STUDY POPULATION
This was a retrospective cross-sectional, descriptive, population-based study that analyzed data from primary health care (PHC) users in La Rioja, a region located in northern Spain (located 42 ° latitude N, 2 ° LW). The study population included 21,490 patients aged 15 to 105 years who regularly or occasionally attended the PHC clinic, with an available serum 25(OH)D measurement corresponding to the first requests from January 2013 to October 2015 (inclusion criteria).
Eligible individuals were users who for any medical reason or on their own initiative attended a primary health care center and underwent blood tests for serum vitamin D levels as requested by a doctor. While no consensus exists on precise indications for 25(OH)D testing in at-risk patients, in our study population vitamin D testing was carried out when high suspicion or diagnostic criteria for rickets or osteomalacia existed, or for any other clinical indication based on the professional clinical judgment of a clinician according to the Endocrine Society Clinical Practice Guideline (27). Consequently, from a clinical perspective, candidates for screening were considered patients at high risk for vitamin D deficiency, which therefore justified a 25(OH)D measurement. No other inclusion or exclusion criteria were defined. It should be noted that no individuals were receiving vitamin D supplementation.
The study was conducted in agreement with the 1990 Declaration of Helsinki and subsequent amendments. The use of data for the purpose of this research was authorized by the steering committee of Hospital San Pedro in Logroño, La Rioja, Spain. Since all data handled by the researchers were anonymous and no additional contact with patients was needed, this study did not require a review by a Research Ethics Board.
DATA COLLECTION
From the electronic medical records of the individuals selected we retrospectively collected the following data: age, gender, first serum 25(OH)D measurement, and date of the blood sample request.
The study population was divided into age groups of five years each. Only the first (14-19 years) and last (≥ 85 years) age groups were different in class interval width. Furthermore, the following 4 age groups were also arbitrarily considered in our analyses; 14-29, 30-54, 55-74, and ≥ 75 years. The season during which vitamin D testing took place was categorized into months (January to December), and seasonality by quarters of a year: winter (January to March), spring (April to June), summer (July to September), and autumn (October to December).
ASSESSMENT OF CIRCULATING 25(OH)D CONCENTRATION
Serum 25(OH)D levels were quantified by using a direct competitive chemiluminescent immunoassay method based on the DiaSorin® Liaison System XL, according to the manufacturer's instructions. All tests for serum vitamin D levels were conducted in the central laboratory of San Pedro Hospital, Logroño, which belongs to the Riojan Health Service (SERIS).
Vitamin D status was evaluated according to the different cut-off points indicated in the literature. Because there is no consensus regarding the 25(OH)D cutoff value for defining vitamin D inadequacy, for the purpose of this study the reference ranges used were based upon the recommendations of the US Institute of Medicine (USIOM) (28) and the US Endocrine Society (USES) (27). The USIOM defines vitamin D deficiency, insufficiency, and sufficiency as 25(OH)D concentrations of < 12 ng/mL (30 nmo l/L), 12-20 ng/mL (30-50 nmol/L), and ≥ 20 ng/mL (50 nmol/L), respectively. The USES-recommended 25(OH)D cutoffs to define vitamin D deficiency, insufficiency, and sufficiency/adequacy were < 20 ng/mL, 20-30 ng/mL, and ≥ 30 ng/mL, respectively. Hypovitaminosis D was also defined considering 2 additional cutoff points for 25(OH)D (< 20 ng/mL and < 30 ng/mL).
STATISTICS
All descriptive and comparative analyses were performed using the STATA software, version 15.0 194 (StataCorp LP, Tx. USA). The results are expressed as mean (SD) for quantitative variables and number (%) for qualitative variables, unless otherwise indicated. Differences between groups were examined by an independent Student's t-test or by χ2 or one-way ANOVA tests with Bonferroni's post hoc analysis, as appropriate. All tests were two-tailed, and p values less than 0.05 were considered statistically significant.
RESULTS
The study results are based on the data analysis of 21490 PHC users with a serum vitamin D test measurement corresponding to the first requested blood test from January 2013 to October 2015. Of these, 74.3 % (n = 16,000) were women. The mean ages of the women and men were 62 (range, 14-105) and 63 (range, 14-101) years, respectively. As shown in table I, the average 25(OH)D level was 18.3 (SD, 11.6) ng/mL in the whole sample; 25(OH)D levels were significantly lower in men (17.6 ng/mL) than in women (18.5 ng/mL) (p < 0.001). Regarding age groups, the highest 25(OH)D levels were found in the groups of 55-59, 60-64, 65-69, and 70-74 years of age, and the lowest in the groups of 80-85 years of age and older. In women, the distribution of 25(OH)D levels among age groups showed a similar pattern. However, in men, the highest mean 25(OH)D concentrations were found in the youngest groups (14-19, 20-24, and 25-29 years) whereas the lowest mean levels were recorded in the oldest groups (80-85 years and older).
Table I. Mean 25(OH)D values in the study population and according to age group and gender
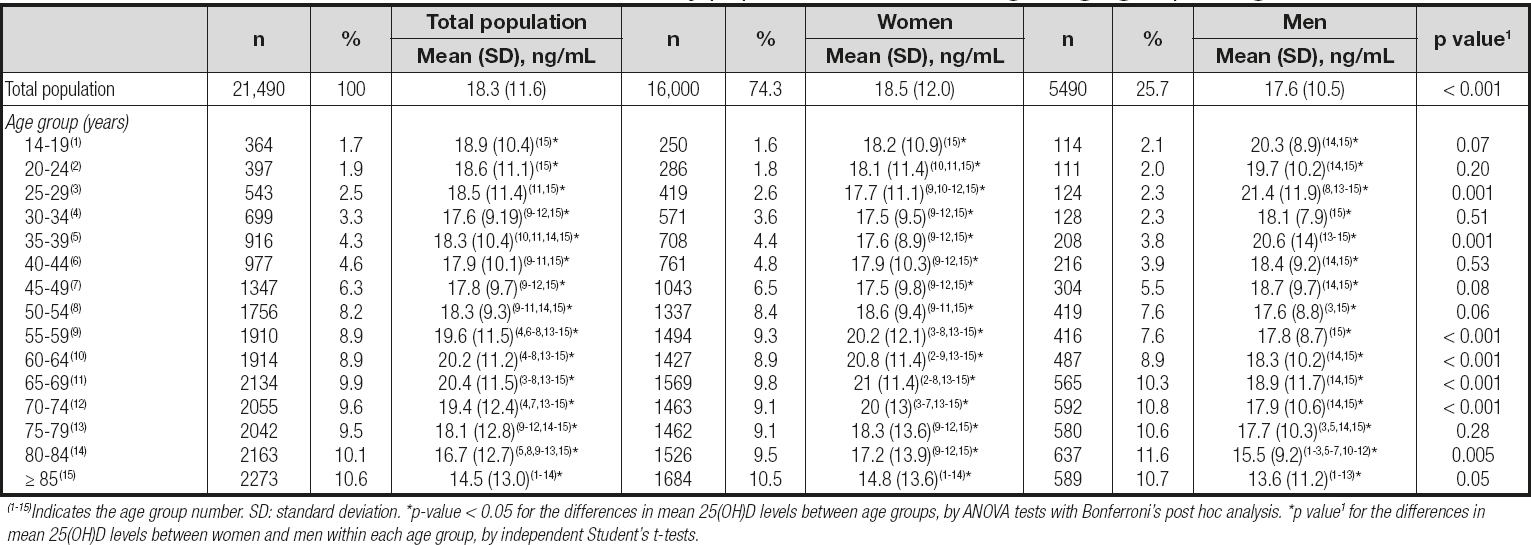
(1-15)Indicates the age group number. SD: standard deviation. *p-value < 0.05 for the differences in mean 25(OH)D levels between age groups, by ANOVA tests with Bonferroni's post hoc analysis. *p value1 for the differences in mean 25(OH)D levels between women and men within each age group, by independent Student's t-tests.
Overall, the prevalence rate of vitamin D inadequacy varied according to the different cutoff values, with significant differences between genders (Table II and Table III). Using the USIOM interpretation of serum 25(OH)D levels, hypovitaminosis D (25(OH)D < 20 ng/mL) was reported in 63.7 % of patients; about half of them (30.9 % of study sample) had vitamin D deficiency (25(OH)D < 12 ng/mL). Furthermore, 32.8 % of subjects were found to have vitamin D insufficiency (25(OH)D = 20-30 ng/mL), and only 10.3 % of the whole sample had sufficient/optimal levels of vitamin D (25(OH)D > 30 ng/mL as USES cutoff) (Table II). As shown in table III, the prevalence rate of hypovitaminosis D was significantly higher in men than in women regardless of 25(OH D cutoffs (p < 0.001). Hypovitaminosis D (25(OH)D < 20 ng/mL) was highly prevalent at 72.6 % among patients over 75 years of age, whereas in the groups of 14-29 and 55-74 years prevalence was 59.8 % and 57.6 %, respectively (Table II). The highest rate of hypovitaminosis D was found in patients over 85 years of age (79.4 %), and the lowest rate in the group of 65-69 years (54.9 %) (Fig. 1). When the cutoff value for defining hypovitaminosis D was set at < 30 ng/mL, prevalence was as high as 89.7 % in the whole sample, and it was slightly but significantly higher in men than in women (91.7 % vs 88.9 %, respectively, p > 0.001), and also in all age groups (Table III and Fig. 2).
Table II. Prevalence rate (% (95 % CI)) of vitamin D deficiency, insufficiency, and sufficiency/adequacy in the study population and according to gender
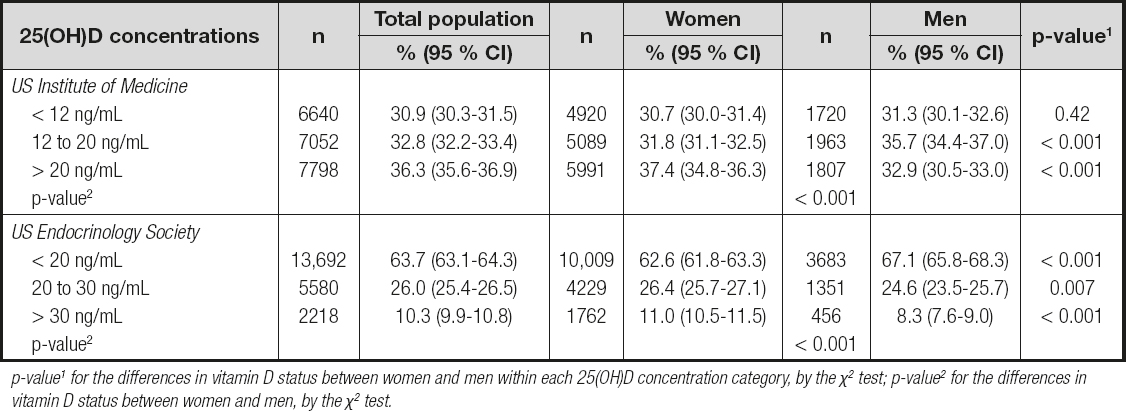
p-value1 for the differences in vitamin D status between women and men within each 25(OH)D concentration category, by the χ2 test; p-value2 for the differences in vitamin D status between women and men, by the χ2 test.
Table III. Prevalence rate (% (95 % CI)) of hypovitaminosis D in the study population and according to age groups and gender
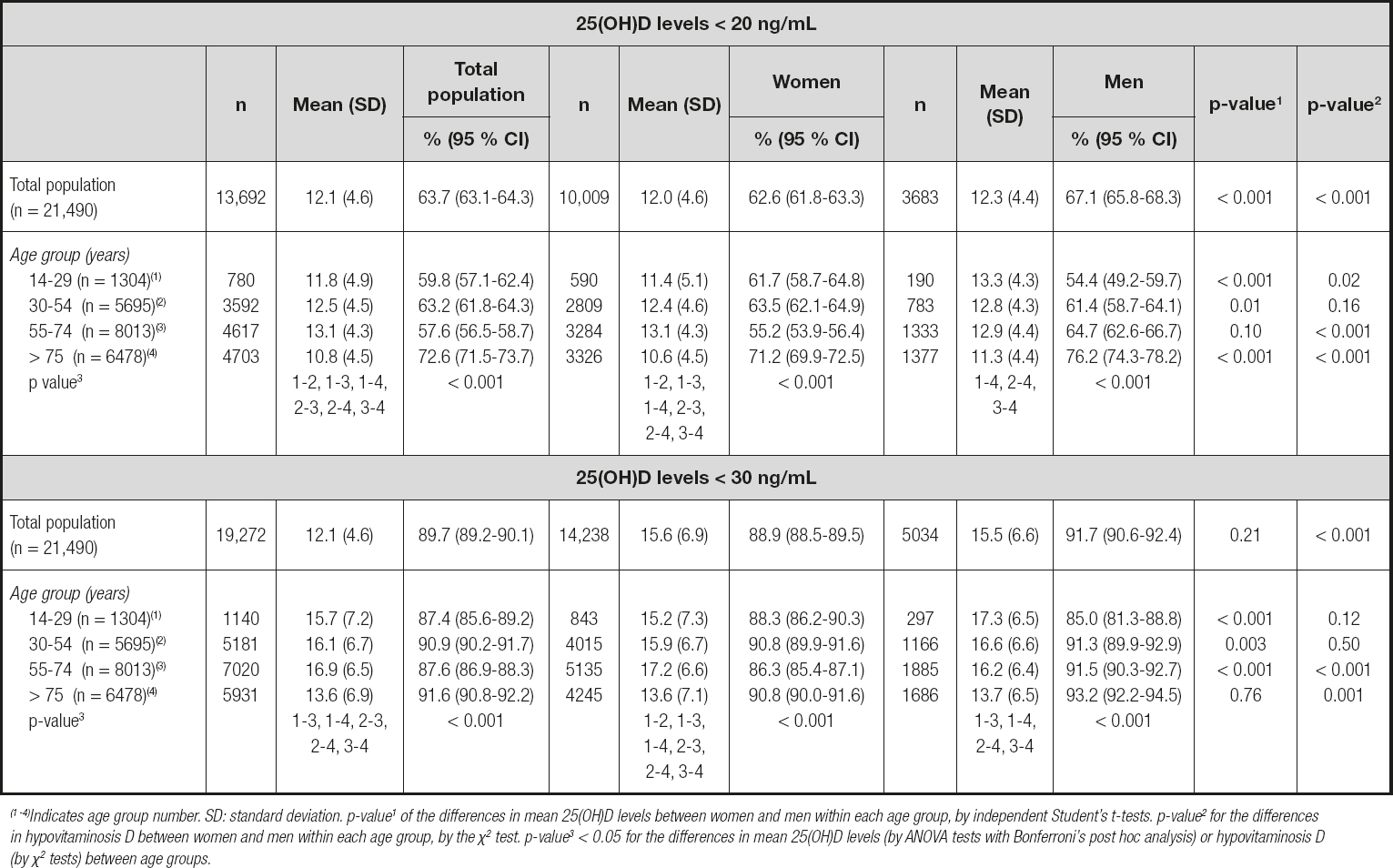
(1 -4)Indicates age group number. SD: standard deviation. p-value1 of the differences in mean 25(OH)D levels between women and men within each age group, by independent Student's t-tests. p-value2 for the differences in hypovitaminosis D between women and men within each age group, by the χ2 test. p-value3 < 0.05 for the differences in mean 25(OH)D levels (by ANOVA tests with Bonferroni's post hoc analysis) or hypovitaminosis D (by χ2 tests) between age groups.

Figure 1. Distribution of the study population according to the USA Institute of Medicine criteria to define vitamin D status by age groups and gender. (1-4) Indicates age group number. P value < 0.05 (groups 5, 8, 9, 10, 11, 12, 14, and 15) of the differences in vitamin D (25 (OH)D <20 ng/mL) deficiency prevalence between gender for ages groups.

Figure 2. Distribution of the study population according to the USA Endocrinology Society criteria to define vitamin D status by age groups and gender. (1-4) Indicates age group number. P value < 0.05 (groups 8-12, and 14) of the differences in vitamin D (25 (OH)D <30 ng/mL) deficiency prevalence between gender for ages groups.
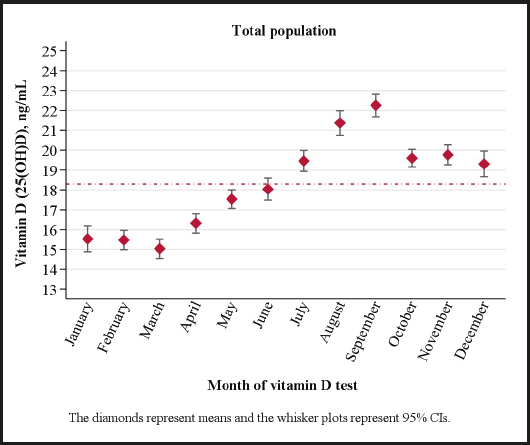
As expected, season had a significant effect on 25(OH)D levels (Table IV and Fig. 3). March (15.1 ng/mL) was the month of the year in which the lowest 25(OH)D levels were found, whereas the highest levels were observed in September (22.2 ng/mL) (Fig. 3). The mean level of 25(OH)D in winter was significantly lower than in the other seasons (p < 0.001), with significant differences in levels between spring, summer, and autumn regardless of age group. The highest levels of 25(OH)D were found in the summer (20.9 ng/mL), with mean values above 20 ng/ml in all age groups except in patients over 75 years of age (17.7 ng/mL) (Table IV).
Table IV. Mean vitamin D (ng/mL) levels according to age group and season of the year
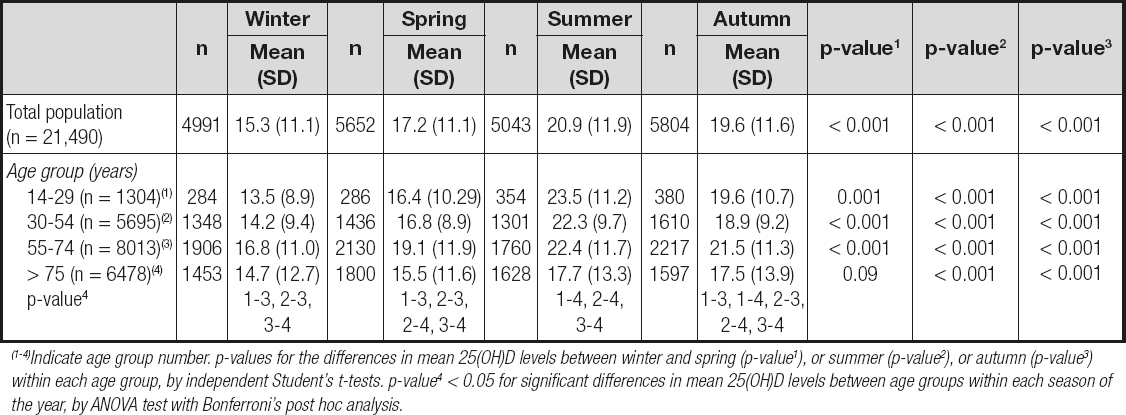
(1-4)Indicate age group number. p-values for the differences in mean 25(OH)D levels between winter and spring (p-value1), or summer (p-value2), or autumn (p-value3) within each age group, by independent Student's t-tests. p-value4 < 0.05 for significant differences in mean 25(OH)D levels between age groups within each season of the year, by ANOVA test with Bonferroni's post hoc analysis.
Hypovitaminosis D rates during winter, spring, summer, and autumn were 76.5 %, 68.7 %, 51.8 % and 58.3 %, respectively (p < 0.001) (Table V). Winter and spring were the seasons in which hypovitaminosis D was higher in all age groups as compared to summer or autumn (p < 0.001). Patients whose age was over 75 years exhibited rates of hypovitaminosis D in all seasons when compared to other age groups except for winter, where hypovitaminosis D rate was higher in the youngest (14-29 years) and/or middle-aged (30-54 years) groups (Table V).
Table V. Prevalence rate (% (95 % CI)) of hypovitaminosis D in the study population, according to age group and season of the year

p-value for the differences in hypovitaminosis D between winter and spring (p-value1), summer (p-value2), or autumn (p-value3) within age groups, by the χ2 test; p-value4 is for the differences in hypovitaminosis D between age groups within each season of the year, by the χ2 test.
DISCUSSION
This study explored for the first time vitamin D status in at-risk patients attending primary healthcare facilities in La Rioja, Spain. Our results have shown that hypovitaminosis D was highly prevalent in our region of study. More than two-thirds of the population were vitamin D deficient (30.9 %) or insufficient (32.8 %) according to the USIOM criteria. Vitamin D hypovitaminosis was more prevalent in men (67.1 %) than in women (62.6 %), and up to 72.6 % of patients older than 75 years had 25(OH)D levels below 20 ng/mL. Using a stricter criterion, as the USES cutoff point (30 ng/mL) for defining vitamin D insufficiency, the prevalence rate rose to as high as 92.7 %. As expected, winter was shown to be an important risk factor for decreased 25(OH)D levels.
Our findings indicate a breakthrough in identifying the burden vitamin D represents in order to control and improve the prognosis of this condition. In addition, they support the relevance of vitamin D status screening as part of the routine laboratory bloodwork usually ordered by primary care physicians, especially for groups potentially at risk of inadequacy, and providing appropriate population-based interventions to combat this global public issue associated with serious consequences for health (16). Along these lines, some countries have adopted public health policies that include food fortification, and vitamin D supplementation for high-risk population groups (4).
Circulating 25(OH)D levels in the blood are subject to cyclical variations over the course of the year based on genetic (ethnicity, gender, polymorphisms), environmental, and lifestyle factors (UVB exposure, skin pigmentation, clothing style, diet, dietary supplements use), advanced age, and the presence of certain physiological or chronic diseases (4). This suggests that the number of factors contributing to vitamin D deficiency, and their interrelations, should be taken into account when it comes to making an adequate clinical decision (29). Furthermore, it is essential and imperative to guide future public health policies.
Globally, vitamin D insufficiency is prevalent in all regions of the world (2,3). The high prevalence of vitamin D deficiency observed in the current study is comparable to what was previously found in various subpopulations in Spain (17,18,30); the prevalence of 25(OH)D levels lower than 20 ng/mL ranged from 61 % among the youth (21) to 87 % among middle-aged adults (22,23); and in the elderly, whether institutionalized or living in the community, this prevalence ranged from 79 % to 91 % (24-26). Clearly, vitamin D insufficiency is the result of a complex interplay of the aforementioned factors. However, in Spain, despite being a country with many sunlight hours (mean, 2,900 hours/year) (31), a diminished or absent vitamin D synthesis in the skin might partly explain the high prevalence of insufficiency in the Spanish population, including that of La Rioja. It has been proposed that climate change has affected the availability of ultraviolet rays in the region; to be sure, in Spain's location above parallel 35 ° N, the oblique incidence of solar rays conditions that most UVB radiation be absorbed by the ozone layer.
As a consequence, in the last few years, European and Spanish populations have been less exposed to ultraviolet rays, which has compromised cutaneous vitamin D synthesis, particularly during the winter (32). In this context, Serrano et al. (33) estimated the time needed to obtain the recommended daily dose of 1000 IU in Valencia, a Spanish province at 39 ° N. It was found that around midday (between 12:30 and 13:30 h) in January, with 10 % of the body exposed, more than two hours of solar exposure are necessary to obtain an optimal vitamin D dose, whereas the rest of the year exposure time ranges from 7 min in July to 31 min in October (33). Thus, the low 25(OH D levels observed in our at-risk population in La Rioja (42 ° N) perhaps do not represent an unexpected problem, which may be speculatively accounted for by scarce contents of vitamin D in the diet that cannot be compensated for by vitamin D synthesis in the skin following exposure to UVB, all of this combined with darker skin pigmentation, sunscreen use, and clothing.
In the current study, serum 25(OH)D levels were significantly lower in men than in women. Also in agreement with previous studies (2,30), vitamin D deficiency (< 20 ng/mL) affected males and females differently, being more prevalent among men, especially among middle-aged adults (55-74 years) and the elderly over 75 years of age. The presence of intrinsic sexual dimorphisms at the molecular and cellular levels, and of differing sex hormones including sex hormone-binding globulin (SHBG), estradiol, and testosterone, may be responsible for these sex differences (34,35). Furthermore, sex differences might also be partly explained by other factors such as adiposity and fat distribution, smoking, physical activity, and clothing/eating habits. However, neither sex hormones nor these sex-specific factors were determined in the current study. Perhaps, sex disparities regarding the use of health services result in a sample where women represent almost 75 % of subjects. This might lead to an underestimation of the overall prevalence of vitamin D deficiency in men. The highest rate of hypovitaminosis D observed in patients with advancing age might be explained by changes in lifestyle and living conditions. The elderly population has been shown to increase indoor and sedentary activities, and to reduce social life; as a consequence, there is a decrease in sunlight exposure (36) that, along with a reduced ability to synthesize vitamin D (4) and conservative clothing habits, might result in a suboptimal vitamin D status. The decrease in food intake and gut absorption (37), medication use, and pre-existing risk factors usually associated with ageing could provide further explanations. We observed an opposite gender association for vitamin D deficiency in younger people (14-29 years), with women exhibiting here a higher prevalence. This may have been due to the fact that in populations at productive ages regular sun exposure tends to decrease because of changes in lifestyle, with an increased amount of time spent in indoor activities. The liberal use of sunscreen, a pattern especially common among younger women when compared to men, may also support these findings (38). Therefore, in order to ensure sunlight exposure, a promotion of suitable outdoor activities for the different age groups should be included in the setting of health care counseling.
We observed, as in the rest of the world and in other regions of Spain (2,30,33,39), a seasonal variation in serum 25(OH)D levels, with the highest levels being found at the end of summer (August and September), and the lowest levels at the end of winter (February and March). In the current study, the prevalence of hypovitaminosis D followed a seasonal pattern ranging from 51.8 % to 76.5 %, with higher rates in winter in all age groups as compared to summer or autumn. Few hours of sunlight exposure, limited cutaneous synthesis of vitamin D, and the excessive exposure time that is required may account for the low 25(OH D levels recorded during the months of winter. Patients over 75 years exhibited high rates of deficiency or insufficiency throughout the year; however, in winter, the most severely affected age groups included the youngest sample and middle-aged adults. In winter, one individual may require more than two hours of sun exposure to obtain an optimal dose of vitamin D (33). Thus, it is possible that the oldest group of people had spent more minutes in the sun during the middle hours of the day during winter.
Finally, as of today, the optimuml serum level of 25-hydroxyvitamin D remains controversial. It was remarkable for us to find that, when 30 ng/mL and 20 ng/mL were the USES-based cutoff values for vitamin D insufficiency and deficiency, respectively, as many as 89.7 % of patients had insufficient levels and 63.7 % of these were even classified as deficient in vitamin D. This finding suggests that the cutoff value proposed by different international (27,40) and Spanish (41) scientific societies for sufficient or desirable vitamin D levels, namely above 30 ng/mL, invariably shows an important prevalence of subclinical vitamin D deficiency in our at-risk population. In fact, many clinicians frequently report that many healthy people are probably misclassified as deficient in vitamin D.
The main strengths to be considered for our study include a large sample for whom information on 25(OH)D concentrations was available, and the use of the Liaison test, which assesses total 25(OH)D concentrations (i.e., vitamins D2 and D3). However, our study has an important limitation that must be commented on. First, our sample was shaped by an at-risk population instead of healthy subjects, and most of the patients included were women; therefore, the study did not fulfil the criteria for representativeness of the population. However, we examined vitamin D levels in patients with no vitamin D supplementation. Therefore, the prevalence of hypovitaminosis D observed probably reflects the true figure for the general population. Second, the amount of time that our patients spent in the sun was not recorded. We did, however, use the season as a proxy for sun exposure. Third, lifestyle factors such as physical activity and diet, or pathological conditions, were not considered, and they are factors that should be considered in future studies.
CONCLUSIONS
In La Rioja, Spain, hypovitaminosis D was highly prevalent among PHC users, especially in the older age groups and during the winter months. In order to prevent vitamin D deficiency, healthcare advice should be focused on ensuring an optimal vitamin D status through adherence to healthy lifestyles, including a complete and varied diet rich in vitamin D food sources and promotion of outdoor activities, especially during the winter months when sunlight hours tend to decrease.