INTRODUCTION
Hypertension and type 2 diabetes (T2D) has become a global public health concern in the 21st century. Both diseases lead to severe complications such as chronic kidney disease (1) and cardiovascular disease (2), which increase the risk of death over a long period. Both of them are related to lifestyles such as physical exercise (3), alcohol consumption (4), and dietary habits (5,6). Studies have found that about 50 % of T2D patients have hypertension, and 20 % of hypertensive patients have T2D (7). Hypertension coexisting with T2D increases the risk of cardiovascular-related events and makes blood pressure (BP) management more complicated and difficult (8). Drug use alone does not control BP satisfactorily, so lifestyle intervention, such as dietary intervention and exercise, is recommended.
The DASH diet was proposed by National Heart, Lung, and Blood Institute in 1977 to control the BP of hypertensive patients. The DASH eating plan encourages the consumption of potassium-rich vegetables and fruits, including whole grains, poultry, fish, and nuts, and reduces sodium and saturated fat intake (9). There is strong evidence that the DASH dietary pattern can lower BP (10,11), including in patients with T2D and hypertension (12,13). However, as the DASH diet was designed for white ethnicity, it is difficult for Chinese people to follow the original DASH diet. In addition, Chinese people generally prefer salty foods, with an average consumption of 12 g of salt per day (14), but the DASH diet requires a daily consumption of 2300 mg of sodium (equivalent to 5.8 g of sodium chloride) or less (10), which also makes it difficult for the DASH diet to be used in the Chinese population. Among many salt reduction strategies, consuming low-sodium salt is feasible with a low cost. Numerous studies have shown that low-sodium salt can lower BP by reducing sodium and adding potassium (15,16), but it has not been used in the DASH diet so far.
Therefore, in this trial, we used two sodium levels of salt based on a modified DASH diet to investigate the effects of reduced sodium intake on BP in hypertensive patients with T2D based on the modified DASH diet.
MATERIALS AND METHODS
PARTICIPANTS
This study was completed in the Public Health Department of the People's Hospital of Nan'an District, Chongqing, China. A total of 61 hypertensive patients with T2D were included from July to December 2020. Inclusion criteria were age in the range of 50 and 75 years; residence near the hospital, with regular follow-up and without plan of transfer or leaving from July, 2020 to October, 2020; hypertensive patients with T2D (the diagnostic criteria for hypertension are based on the Chinese Guidelines for the Prevention and Treatment of Hypertension (2018 Revised Edition) (24) and the diagnostic criteria for diabetes are based on the Chinese Guidelines for the Prevention and Treatment of T2D (2017 Edition) (25) for those who currently took regular anti-hypertensive/ hypoglycemic drugs; strictly following the two daily meals provided by the investigators during the trial; and the informed consent signed by all the subjects and their family members living together. Exclusion criteria included malignant tumors, acute myocardial infarction, stroke in the past 3 months or other serious disease, expected survival time less than 1 year; increased cortisol disorder or aldosteronism; acute diseases such as upper respiratory tract infection, fever, severe diarrhea; disabilities such as deaf-mute, dementia, severe depression or other mental disorders precluding normal communication; incapability of regular follow-up or loss to follow-up after study entry; renal dysfunction or chronic kidney disease at stage 4 or above; abnormal liver function, with alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels greater than 2 times the upper limit of normal, or total bilirubin level greater than the upper limit of normal; abnormal blood potassium level, < 3.5 mmol/L or > 5.5 mmol/L, or current use of potassium-preserving diuretics; pregnancy or pregnancy possibility, and other contraindications for the use of trial meals; current consumption of low sodium diet or participation in other clinical studies; and other ineligible conditions as adjudicated by investigators.
The study was approved by the Ethics Committee of Chongqing Medical University (approval date: 2020.07.28). The trial was registered at www.chictr.org.cn/. All patients voluntarily participated in the study and signed an informed consent.
STUDY DESIGN
This study was a single-blind trial (patients were blinded to the specific grouping). Sixty-one patients were randomly divided into the low sodium salt group (taking 52 % sodium- restricted formula salt + the modified DASH, n = 30) and the common salt group (taking common salt + the modified DASH, n = 31) by a random number table. The amount of salt intake in both groups was controlled at 5 g/day per person according to the WHO-recommended salt standard. After completion of a baseline survey and medical examination, a dietary intervention would be carried out for 8 weeks, in which weeks 1-2 represented the dietary guidance phase, weeks 3-4 the centralized feeding phase (centralized dining at the hospital canteen), and weeks 5-8 the home medical care phase. All participants were told not to change their previous exercise habits and drug use during the intervention. Participants were followed up in the hospital once a week to collect information on outpatient blood pressure (OBP), salt and drug use. In addition, for trial safety, a medical examination was conducted at 4 weeks and the end of the intervention (same as baseline).
THE MODIFIED DASH
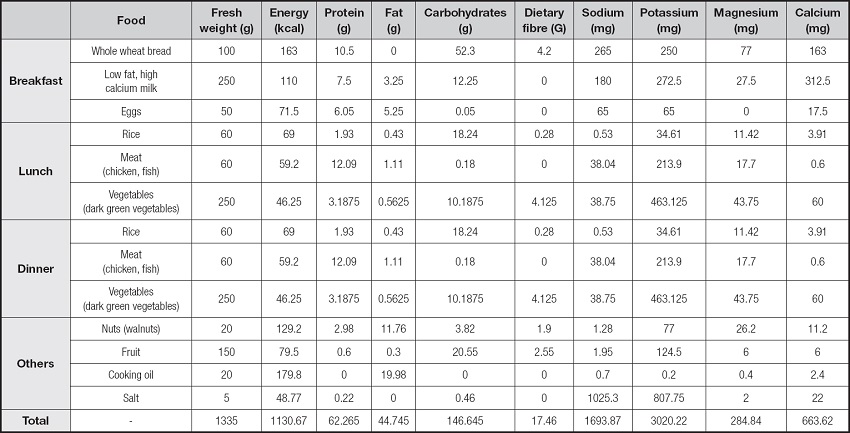
In this study, a modified DASH diet was developed for Chinese patients with T2D and hypertension considering the DASH Dietary Energy Estimation Table, dietary pagoda of Chinese residents (2016), dietary habits and food availability of Chinese residents, as well as the weight and physical activity of the subjects. Special requirements for the modified DASH diet were addition of brown rice, corn, soybeans, red beans and other grains to rice; eating lean meat, poultry, fish and other meat < 120 g/d, with less red meat and more white meat, mainly skinless chicken and fish; drinking a bottle of low-fat and high-calcium milk every day; eating more low-sugar green leafy vegetables, about 500 g a day; eating a moderate quantity of fruits (after meals) and nuts (a handful); daily intake of vegetable oil < 30 grams and salt < 5 grams. Compared with the traditional DASH diet, the modified diet contains less total fat, saturated fatty acids and calories, making it more in line with Chinese eating habits. The modified DASH diet for one person is shown in table I.
SALT
The low sodium salt group received 52 % sodium-restricted formula salt (“Gu Da Chu” developed by Shanghai Institute of Ecological Health Sciences. Name: solid compound condiment, standard of execution: Q/BAAM0009S, food production license number: SC10334042205441; and the main ingredients include potassium chloride (31 %), sodium chloride (52 %), carbohydrates (9.2 %), and protein (4.4 %). The common salt group received common salt (“Jing Xin” developed by Chongqing salt industry group Co., Ltd. Name: purified salt, product standard: NY/T1040, and content of sodium chloride content > 99 %). In Phase 1 and Phase 3, we used 52% low-sodium salt or common salt to completely replace the salt used by the participants at home, and we also provided a quantitative pot and a quantitative spoon for the participants to control the amount of salt used in the family (< 5 g per person per day). In addition, we used an electronic scale (precision: 0.1 g) to weigh salt consumption every week and estimate daily salt consumption for each person in the family.
BP MEASUREMENT
Participants were followed up in the hospital once a week. OBP was measured for three times by trained professionals and completed between 8-9 am, with an interval of about 2 min. The average of the last two OBP measurements was used for the analysis. Automated upper-arm cuff devices according to the oscillometer technique were adopted (manufacturer: Omron, Dalian, Co., Ltd. Product name: “Omron” electronic sphygmomanometer. Model: HEM-7130).
LABORATORY MEASUREMENTS
Laboratory measurements included 24-hour urinary electrolytes, blood electrolytes, blood lipids, liver function, renal function, urinary creatinine, and urinary albumin. All indexes were tested in the Second Affiliated Hospital of CQMU, and we reported the results to patients in a timely manner.
STATISTICAL ANALYSIS
The statistical analysis was carried out using the SPSS 24.0 (IBM, Armonk, NY, USA) program. Quantitative normal-distribution data were described as mean and standard deviation, and the t-test was used to compare differences between groups. Qualitative data were described by frequency, and Pearson's chi-square test was used to compare the differences between groups. Non-positive distribution data are expressed as median and quartiles, and Friedman's Rank Test was used. A repeated measures analysis of variance (RMANOVA) was used to analyze the changes of physical examination indexes during the intervention. The Generalized Estimating Equation (GEE) was used to compare the changes in BP during each week, and Bonferroni's method was used for comparison between groups. P-values < 0.05 were considered statistically significant.
RESULTS
BASELINE CHARACTERISTICS
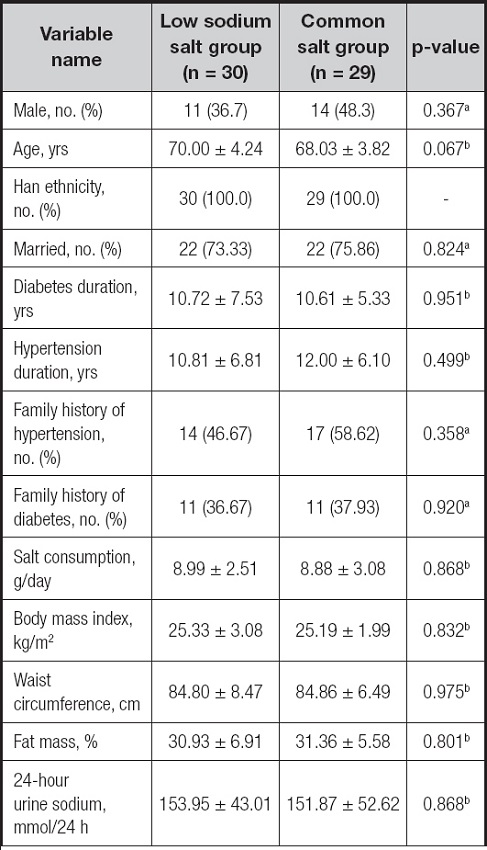
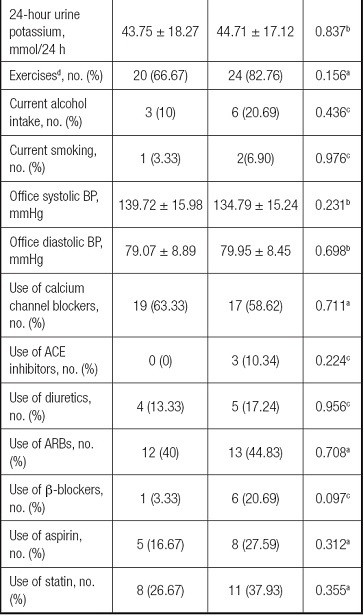
A total of 61 patients were included, and 2 patients were lost to follow-up (due to low back pain and job transfer); 59 patients (30 in the low sodium salt group and 29 in the common salt group) completed the 8-week intervention. There were no differences between the two groups regarding demographic features, lifestyle characteristics, anthropometric indices, 24-hour urine sodium and potassium values, and OBP values (Table II).
BP MEASUREMENTS DURING THE STUDY
The results of GEE showed that one week after intervention, systolic blood pressure (SBP) in the low sodium group and the common salt group decreased by 9.13 % (-12.17 mmHg, p < 0.001) and 5.16 % (-7.16 mmHg, p = 0.012), respectively, and diastolic blood pressure (DBP) decreased by 9.81 % (-7.25 mmHg, p < 0.001) and 6.79 % (-5.29 mmHg, p < 0.001), respectively. At 4 weeks, SBP in the low sodium group and the common salt group decreased by 13.12 % (-17.48 mmHg, p < 0.001) and 8.26 % (-11.47 mmHg, p < 0.001), respectively; DBP decreased by 10.76 % (-7.95 mmHg, p < 0.001) and 7.24 % (-5.64 mmHg, p < 0.001), respectively. At the end of intervention, SBP was reduced by 10.74 % (-14.32 mmHg, p < 0.001) in the low sodium group and 7.91 % (-10.98 mmHg, p < 0.001) in the common salt group, while DBP decreased by 8.55 % (-6.32 mmHg, p < 0.001) and 6.73 % (-5.24 mmHg, p = 0.001). However, there were no statistically significant differences in SBP and DBP between groups (SBP: -0.28 mmHg, p = 0.929; DBP: -3.32 mmHg, p = 0.093) (Table III & Table IV).
Table III. Changes in SBP from baseline during the study
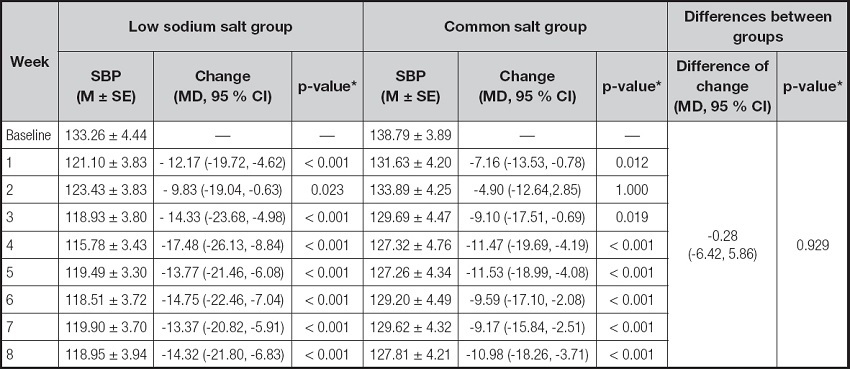
M } SE: mean ± standard error; MD: mean difference.
*The GEE was used for analysis, adjusting gender, age, annual family income, education level, marital status, smoking, drinking, exercise, family history of hypertension, age of hypertension, waist-to-hip ratio, baseline BMI and statins, aspirin use.
Table IV. Changes in DBP from baseline during the study
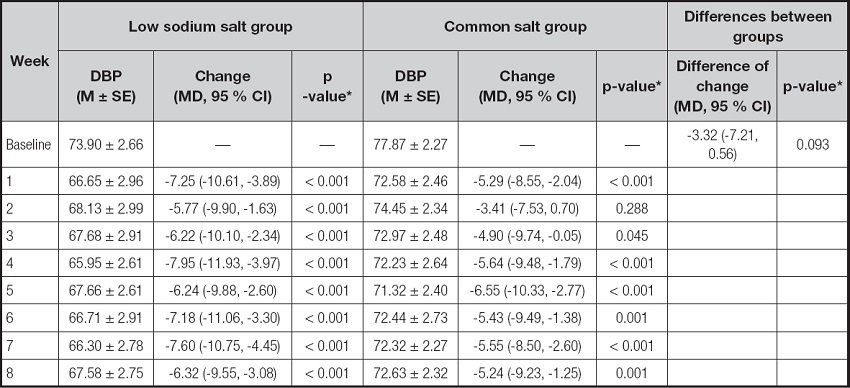
M ± SE: mean ± standard error; MD: mean difference.
*The GEE was used for analysis, adjusting gender, age, annual family income, education level, marital status, smoking, drinking, exercise, family history of hypertension, age of hypertension, waist-to-hip ratio, baseline BMI and statins, aspirin use.
URINE TEST RESULT
An analysis of RMANOVA for repeated measures indicated that 24-hour urine sodium (the low sodium salt group: -49.29 mmol/24 h, p < 0.001; the common salt group: -27.62 mmol/24 h, p = 0.015) decreased significantly in both groups after 4 weeks of intervention. However, 24-hour urine sodium (the low sodium salt group: -23.41 mmol/24 h, p = 0.015; the common salt group: -17.83 mmol/24 h, p = 0.091) decreased significantly only in the low sodium salt group at the end of the intervention. An increase in 24-hour urinary potassium (p = 0.020) and a decrease in the sodium/potassium ratio (p < 0.001) were observed in the low sodium salt group, but not in the common salt group (p > 0.05) (Table V).
Table V. Changes of urine test results during the study
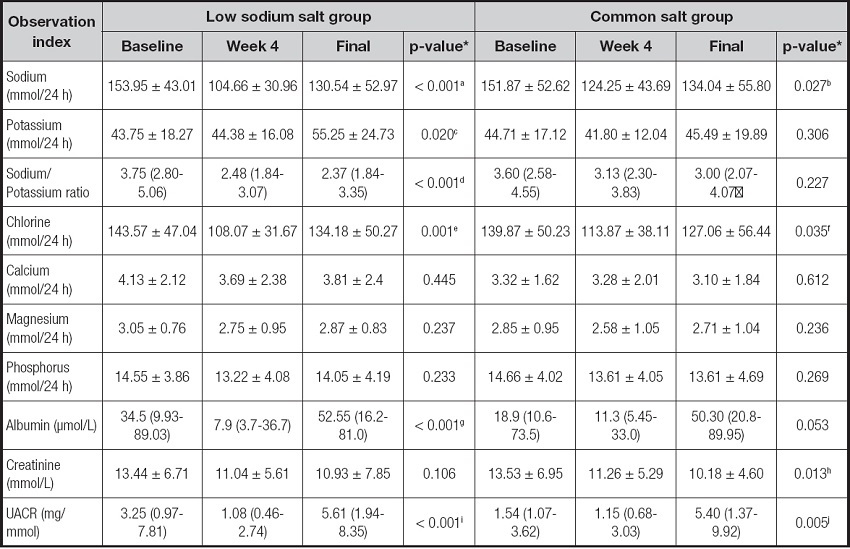
*The RMANOVA was used for analysis. a: baseline vs week 4 (p < 0.001); baseline vs final (p = 0.0150); week 4 vs final (p = 0.006); b: baseline vs week 4 (p = 0.015); c: baseline vs final (p = 0.028); week 4 vs final (p = 0.018); d: baseline vs week 4 (p < 0.001); baseline vs final (p = 0.001); e: baseline vs week 4 (p = 0.002); week 4 vs final (p = 0.005); f: baseline vs week 4 (p = 0.017); g: baseline vs week 4 (p = 0.035); week 4 vs final (p < 0.001); h: baseline vs week 4 (p = 0.036); baseline vs final (p = 0.018); i: baseline vs week 4 (p = 0.017); week 4 vs final (p < 0.001); j: baseline vs final (p = 0.017); week 4 vs final (p = 0.017).
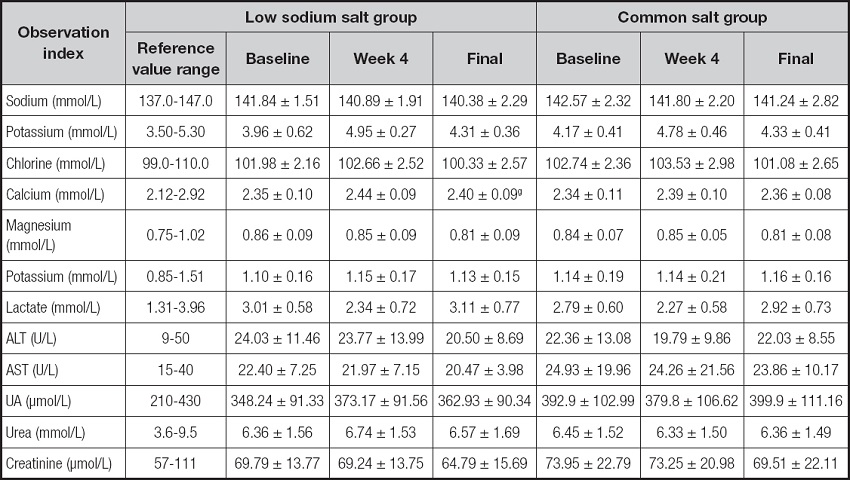
SERUM TEST RESULT
Compared with baseline, changes in sodium, potassium, chlorine and calcium in serum electrolyte concentration were observed in both groups, and the change trend was the same as that of 24-hour urine electrolytes. No serious adverse events occurred during the intervention. After the intervention, 2 items of liver function (AST, ALT) and 3 items of kidney function (uric acid, urea, creatinine) were in the normal range (Table VI).
DISCUSSION
The Chinese Guidelines for the Management of Hypertension (2018) (17) recommend that the target of hypertension combined with diabetes should be < 130/80 mmHg. Therefore, patients with hypertension and T2D should have a more strict BP control than those with normal hypertension. A large number of studies have repeatedly demonstrated that consumption of the DASH diet could decrease BP in hypertensives (10,11), but it has been less commonly used in hypertensive patients with T2D. In the study by Azadbakht et al. (13), after 8 weeks of DASH diet intervention among patients with T2D, the intervention group had a significant BP reduction compared with the control group. Paula et al. (14) also had a similar conclusion, but in the study of Hashemi et al. (18), there was no significant difference in the reduction of BP between the DASH diet and the control diet. To our knowledge, this is the first study to evaluate the effect of reduced sodium intake on BP in Chinese hypertensive patients with T2D under a modified DASH diet.
Studies have shown that high dietary sodium intake can lead to high BP by inhibiting the activity of Na+-K+-ATPase pumps in cell membranes (22), damaging vascular endothelial function (23) and activating the renin-angiotensin-aldosterone system (RAAS) (24). There is substantial evidence that reducing sodium intake lowers BP in persons with hypertension. Contrary to the effect of sodium on BP, potassium can lower BP by stimulating Na+-K+-ATPase pumps and the opening of potassium channels in vascular smooth muscle cells and adverse nerve receptors (25). Previous studies (26,27) suggest that the high level of potassium in the DASH diet is important for its hypotensive effects. The DASH diet also recommends reducing dietary sodium and consuming more potassium-rich fruits and vegetables [9], but it is hard to achieve the desired effect by supplementing potassium with food. Studies have shown that increasing potassium intake by consuming low sodium salt is an effective and economical way (28). In the 18 % substitute salt experiment by Professor Wu Yangfeng, the BP lowering effect of low sodium salt (sodium chloride 18 %, potassium chloride 35 %) has been demonstrated in the same type of phase 1 single-arm trial (28,30). However, the promotion of formula salt remains a challenge because it contains different ratio of sodium to potassium from that of ordinary salt, leading to a peculiar taste.
We used the salt with a sodium chloride content of 52 % and a potassium chloride content of 31 % in the low sodium salt group, providing a daily intake of 1,693.87 mg of sodium and 3,020.22 mg of potassium, whereas the common salt group took salt with a sodium chloride content of > 99 %, giving patients a daily intake of 2,617.57 mg of sodium and 2,212.47 mg of potassium. Participants had a high compliance with the intervention, and noone dropped out. As the golden criteria to determine the intake of sodium, 24-hour urine electrolytes have been widely used in scientific research (21). We calculated the 24 h urine sodium from three physical examinations — the 24 h urine sodium decreased in two groups, and the 24 h urine potassium only increased in the low sodium salt group significantly. Mean sodium intake at baseline was 3540.85 mg in the low sodium salt group and 3493.01 mg in the common salt group. At week 4 and end of intervention, sodium intake was reduced in both the low sodium salt group (-1133.67, -538.43 mg) and the common salt group (-635.26, -410.09 mg). However, mean potassium intake at baseline was 1706.25 mg in the low sodium salt group and 1743.69 mg in the common salt group. At week 4 and at end of intervention, sodium intake was increased in the low sodium salt group (24.57, 448.5 mg), but not in the common salt group (-113.49, 30.42 mg). Overall, sodium reduction on the DASH diet had a significant effect on reducing sodium intake, and the use of low sodium and high potassium salt significantly increased potassium intake.
Our study showed that SBP and DBP were significantly reduced at week 1, at week 4 and at the end of the intervention in the low sodium salt group (SBP: -12.17, -17.48, -14.32 mmHg; DBP: -7.16, -11.47, -10.98 mmHg) and the common salt group (SBP: -7.25, -7.95, -6.32 mmHg; DBP: -5.29, -5.64, -5.24 mmHg), with the most pronounced drop at week 4. From baseline to the end of the intervention, there were no statistically significant differences in systolic and diastolic BP between the two groups (SBP: -0.28 mmHg, p = 0.929; DBP: -3.32 mmHg, p = 0.093). But we observed that the decrease of SBP in the low sodium salt group appeared earlier and more significantly than that in the common salt group. In a cohort randomized trial of 20,995 hypertensive patients by Neal Bruce et al. (29), 24-hour urinary sodium excretion (-350 mg), 24-hour urinary potassium excretion (803 mg) and mean SBP (−3.34 mmHg) were significantly different between the salt substitute (75 % sodium chloride and 25 % potassium chloride) and the regular salt groups. The observed changes in 24-hour urinary sodium and potassium excretion are of a magnitude consistent with the measured decline in SBP. Finally, after five years of follow-up, the salt substitute group (low sodium and high potassium) had a lower rate of stroke, cardiovascular events, and death from any cause than did the regular salt group. Long-term effects of low sodium and high potassium on hypertension had been widely claimed. However, our study was conducted based on diet, which greatly interfered with the life of patients and was easily affected by social factors, so long-term observation could not be carried out. Therefore, we speculate that the application of low-sodium salt in the DASH diet may have more beneficial and significant effects on BP reduction in hypertensive patients with T2D if long-term, large size study is carried out.
Most evidence for the DASH diet comes from either short-term feeding studies (11,19) or dietary behavioural intervention studies (20), but this study combined feeding and dietary behaviour interventions. Interestingly, although the dietary and salt requirements for participants during the dietary behaviour intervention were the same as those during the feeding trial, we still observed a mild increase in BP in phase 3, as confirmed by the changes in urine sodium and potassium in 24 hours urine analysis. The possible reason for this increase is cooking meals at home that meet DASH nutritional requirements is affected by many factors, leading to the relatively poor adherence. On the other hand, the modified DASH diet menu contains coarse grains, low-fat milk, and nuts that do not meet Chinese diet habits. In the future, we should strengthen health education on diet to change the dietary behavior of Chinese people with hypertension and T2D.
The high potassium content of the low-sodium salt is thought to cause hyperkalemia and safety monitoring should be conducted. During the study period, no serious adverse events occurred, and the safety of the participants was monitored and confirmed. Serum test results showed that there was a slight increase in potassium during the intervention period, but it was still within the normal range. In addition, there was no significant difference in the changes of AST, ALT, UA, Urea.
CONCLUSIONS
Under the modified DASH diet, both 52 % sodium salt and common salt can improve BP in community hypertensive patients with T2D who took regular medication, with certain safety. The 52 % sodium salt may improve sodium and potassium intake more significantly than the common salt. There is reason to believe that long-term adherence to 52 % sodium salt can be the more rational intake of sodium and potassium, to achieve health promotion. This is an effective nutritional strategy for BP control in patients with hypertension and T2D.
SHORTCOMINGS
There are still some limitations in this study. It is a phase-I clinical trial designed to observe the efficacy and safety of different sodium levels of salt on BP control based on the DASH diet. Firstly, the sodium content of the salts used in the tests did not vary much, making it difficult to make a significant difference in short-term effects. This can only be achieved by extending follow-up or using salt with lower sodium content. Secondly, due to the half-opened trial, confounding factors had an impact on the results during the period of home medical care. Because of patients' inability to fully follow the trial's dietary requirements, the effect of the intervention may be underestimated.