INTRODUCTION
Arterial stiffness is a progressive clinical condition with multiple causes and contributors, characterized by the accumulation of lipids and fibrous elements in the large arteries (1). It is related to cardiovascular diseases, which are the cause of premature deaths. The economic burden of atherothrombotic disease is high and expected to increase with increased survival and the aging population (2). A series of studies have shown that there is a close relationship between arterial stiffness and hypertension, and the development of arterial stiffness may precede that of hypertension (3). In addition, studies have shown that diabetes can also induce the development of arterial stiffness or further accelerate its progression (4).
Unhealthy diet may be an important risk factor for arterial stiffness (5). Studies have found that the Dietary Approaches to Stop Hypertension (DASH) diet and salt restricted have a good control effect on blood pressure, blood lipid, weight, metabolic status and blood glucose (6), which are related to arterial stiffness (3). However, there are few studies about the effect of low-sodium salt applied to DASH diet on arteriosclerosis in patients with hypertension and type 2 diabetes.
This eight-weeks, randomized, controlled, single-blind trial of older adults with hypertension complicated with type 2 diabetes examined the effects of low sodium salt applied to Chinese modified DASH (CM-DASH) diet on arterial stiffness. We hypothesized that low-sodium salt applied to CM-DASH diet would improve arterial stiffness under safe conditions.
MATERIALS AND METHODS
We recruited the participants by using the following eligibility criteria: a) age ≥ 50 and ≤ 75 years old; b) residence near the hospital, no withdrawal or plan to go out during July-October 2020, possibility of regular follow-up; 3) hypertensive patients with type 2 diabetes (the diagnostic criteria for hypertension are SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg [based on the Chinese Guidelines for the Prevention and Treatment of Hypertension 2018 Revised Edition] [7] and the diagnostic criteria for diabetes are FBS ≥ 7.0 mmol/l and/or PBS ≥ 11.1 mmol/l [based on the Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes, 2017 edition] [8]) who currently regularly take antihypertensive drugs/hypoglycemic drugs; d) to strictly abide by the daily meals provided by us in the course of the study; and d) all the subjects and their family members living together signed the informed consent. The exclusion criteria were: a) patients with malignant tumor, acute myocardial infarction, stroke within three months or other serious diseases, and expected survival time less than one year; b) increased cortisol disorder or aldosteronism; c) acute diseases such as upper respiratory tract infection, fever, severe diarrhea; d) deaf-mute, dementia, and serious depression or other mental disorders which prevent from communicate normally; e) inability to be followed up due to limited mobility or other reasons; f) renal dysfunction or chronic kidney disease at stage 4 or above; g) abnormal liver function, with alanine aminotransferase (ALT) or aspartate aminotransferase (AST) level greater than two times the upper limit of normal, or total bilirubin level greater than the upper limit of normal; h) abnormal blood potassium < 3.5 mmol/l or > 5.5 mmol/l, or current use of potassium-preserving diuretics; i) attending to participate in other clinical studies or current consumption of low-sodium diet; and j) other ineligible conditions as adjudicated by investigators.
This eight-weeks, randomized, controlled, single-blind trial of older adults with hypertension complicated with type 2 diabetes was conducted in Chongqing, China, during December, 2020. A total of 61 patients were enrolled and randomly allocated to a low sodium salt group (LSSG; n= 30) or a normal sodium salt group (NSSG; n= 31), using random number table method. In the coming eight-week period, patients in the LSSG or NSSG were asked to eat 5 g/day low-sodium salt (“Mushroom Chef” was developed by the Shanghai Institute of Ecological Health Sciences; name: solid compound seasoning, executive standard: Q/BAAM0009S, food production license number: SC10334042205441, main ingredients: potassium chloride [31 %], sodium chloride [52 %], carbohydrate [9.2 %], protein [4.4 %]) or normal-sodium salt (“Jingxin” was developed by Chongqing Salt Industry Group Co., Ltd.; name: pure salt, product standard: NY/T1040, sodium chloride content [99 %]) respectively, plus CM-DASH diets. We fully consider the price and availability of local ingredients, the eating preferences of the population and the taste of the food to design the CM-DASH diet daily recipes and CM-DASH diet requirements: (a) rice: whole grain (5:1) and (b) mainly white meat (poultry or fish) and (c) low-fat milk and (d) enough vegetables (mainly green leafy vegetables) and (e) fruits with low sugar content and (f) proper amount of nut food and (g) the daily amount of cooking oil (mainly vegetable oil) < 30 g, salt content < 5 g.
Before the intervention, the data on patients' demographic and socioeconomic status were gathered via an in-person interview. Anthropometry data (weight, body mass index [BMI], waist-hip rate [WHR]), blood pressure (systolic blood pressure [SBP], diastolic blood pressure [DBP]) and blood sugar (fasting blood sugar [FBS], and postprandial blood sugar [PBS]) were measured before and after intervention. Fasting venous blood samples were collected before, at week 4 and after the intervention from all enrolled participates to assess lipid profile, liver function damage and renal function damage indices. In addition, 24-hour urine samples were also collected before, at week 4 and after the intervention to assess potassium and sodium excretion.
Brachial-ankle pulse wave velocity (baPWV) is a frequently-used method to measure arteriosclerosis by analyzing the arterial waves of the arm and tibialis, which has the advantages of simple method and good repeatability (9). The ankle-brachial index (ABI) is a non-invasive tool for the assessment of vascular status, which consists of the ratio between the systolic blood pressure of the lower extremity, specifically the ankle, and the upper extremity (10). The baPWV and ABI were measured with Omron Atherosclerosis Detection Device HBP-8000 before and after the intervention. Before the measurement, the subjects were asked not to smoke and rest for more than five minutes.
Total cholesterol (TC), triglyceride (TG), high-density lipoproteins-cholesterol (HDL-C) and low-density lipoprotein-cholesterol (LDL-C) were used to calculate atherosclerosis related indices:
Atherogenic index of plasma (AIP) = log (TG [mmol/l]/HDL-C [mmol/l]).
Castelli risk index-I (CRI-I) = TC (mmol/l)/HDL-C (mmol/l)
Castelli risk index-II (CRI-II) = LDL-C (mmol/l)/HDL-C (mmol/l)
TG to HDL-C ratio = TG (mmol/l)/HDL-C (mmol/l)
The Shapiro-Wilk test was used to test the normal distribution. Quantitative data are shown as mean ± SD if normally distributed and as median and inter-quartile ranges (25thand 75thpercentile) if non-normally distributed. Qualitative data are expressed as a frequency. An independent-samples t-test was used to compare the difference between groups and paired t test was used for changes within group. Quantitative non-normally distributed data (baseline fasting blood glucose [FBG]) were compared using an independent-samples Mann-Whitney U test and correlated-samples Wilcoxon test. Categorical variables were compared using Pearson's Chi-squared test. ANOVA for repeated measurement was used for changes in urine test. SPSS24.0 statistical software was used for statistical analysis. All trials were bilateral, and p< 0.05 was considered statistically significant.
RESULTS
A total of 61 participants were enrolled in this study, and 59 patients (69.03 ± 4.12 years, 25 male) completed the entire study (two subjects in the NSSG withdrew from the study because of worsening of pre-existing disease or work conflict). There was no significant difference in baseline characteristics except that the postprandial blood glucose in LSSG was higher than that in NSSG (Table I).
Table I. Baseline characteristics of patients*.
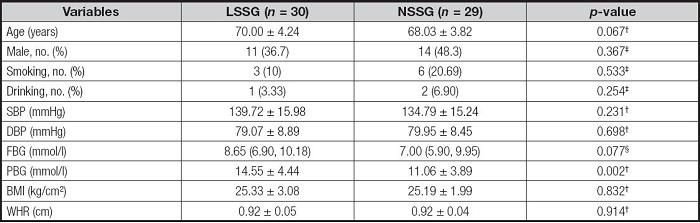
LSSG: low sodium salt group; NSSG: normal sodium salt group; SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood sugar; BMI: body mass index; WHR: waist-hip rate.
*Values are expressed as mean ± SD, median (first quartile, third quartile) or number, frequency (%).
†Independent samples t-test.
c ‡Chi-squared test.
§Independent samples Mann-Whitney U test.
As compared to baseline, LSSG showed significant reduction in ABI (-0.09 ± 0.11, p< 0.001), baPWV (-133.07 ± 265.99 cm/s, p= 0.010), TG to HDL-C ratio (-0.47 ± 1.06, p= 0.021) and AIP (-0.13 ± 0.26, p= 0.012) at week 8. NSSG only showed significant reduction in ABI (-0.06 ± 0.12, p= 0.01) at week 8. The changes of AIP and TG to HDL-C ratio in the LSSG were significantly higher than those in the NSSG (p= 0.008, p= 0.0013) (Table II).
Table II. Effect in arteriosclerosis tests, atherosclerosis-related indices, anthropometry, blood pressure and blood glucose*.
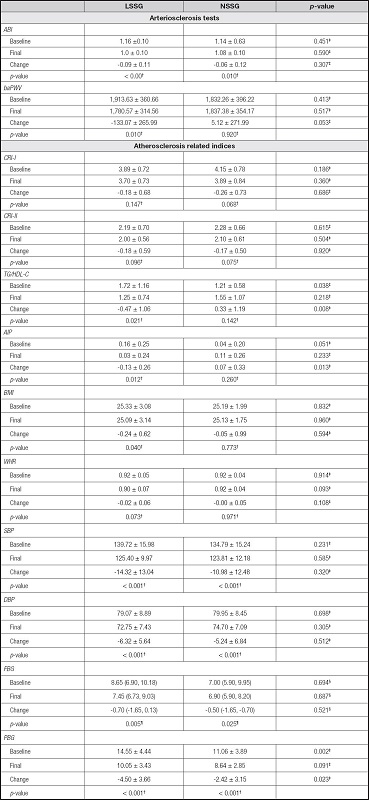
LSSG: low sodium salt group; NSSG: normal sodium salt group; ABI: ankle-brachial index; baPWV: brachial-ankle pulse wave velocity; CRI-I: TC (mmol/l)/HDL-C (mmol/l); CRI-II: LDL-C (mmol/l)/HDL-C (mmol/l); TG to HDL-C ratio: TG (mmol/l)/HDL-C (mmol/l); AIP: log (TG [mmol/l]/HDL-C [mmol/l]); BMI: body mass index; WHR: waist-hip rate; SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood sugar.
*Values are expressed as mean ± SD or median (first quartile, third quartile).
†Paired samples t-test.
‡Independent samples t-test.
§Independent samples Mann-Whitney U test.
¶Correlated samples Wilcoxon test. p < 0.05..
As compared to baseline, LSSG showed significant reduction in BMI (-0.24 ± 0.62, p= 0.040), SBP (-14.32 ± 13.04, p< 0.001), DBP (-6.32 ± 5.64, p< 0.001), FBG (-0.75 ± 1.54, p= 0.013) and PBG (-4.50 ± 3.66, p< 0.001) at week 8. NSSG showed significant reduction in SBP (-10.98 ± 12.48, p< 0.001), DBP (-5.24 ± 6.84, p< 0.001), FBG (-0.69 ± 1.62, p= 0.030) and PBG (-2.42 ± 3.15, p< 0.001) at week 8. The changes of PBG in the LSSG were significantly higher than those in the NSSG (p= 0.023) (Table II).
As compared to baseline, LSSG showed significant reduction in sodium and sodium/potassium at week 4 (both p< 0.001) and at week 8 (p= 0.015, p< 0.001). While NSSG only showed significant reduction in sodium at week 4 (p= 0.015) (Table III). ALT, AST, BUA, BU and SCR of both groups were within the reference range at baseline, at week 4 and at week 8 (Table IV).
Table III. Effect in 24-hour urinary excretion*.
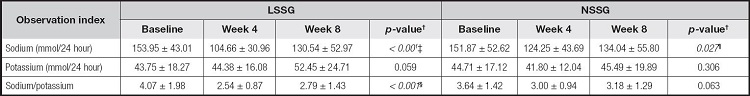
LSSG: low sodium salt group; NSSG: normal sodium salt group. Statistically significant forp < 0.05. Bold is statistically significant.
*Values are expressed as mean ± SD.
†ANOVA for repeated measurement.
‡Baselinevs week 4(p < 0.001); baselinevs week 8 (p= 0.015); week 4vs week 8(p = 0.006).
§Baselinevs week 4(p < 0.001); baselinevs week 8(p < 0.001); week 4vs week 8(p = 0.244).
¶Baselinevs week 4(p = 0.015); baselinevs week 8(p = 0.091); week 4vs week 8(p = 0.310). p < 0.05.
DISCUSSION
Arteriosclerosis, hypertension and diabetes are risk factors for cardiovascular disease, and arteriosclerosis may be associated with increased blood pressure in the elderly (11), due to the change of artery buffer function, leading to increased blood pressure (12). Normal arterial stiffness was defined as baPWV < 1,400 cm/s, borderline arterial stiffness was defined as 1,400 ≤ baPWV < 1,800 cm/s, and elevated arterial stiffness was defined as baPWV ≥ 1,800 cm/s (13). The 2013 European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) guidelines for the management of arterial hypertension concluded that an increase in baPWV by 1 m/s was associated with increases in 12 %, 13 %, and 6 % in total cardiovascular events, cardiovascular mortality, and all-cause mortality (14). Professor Wu found that the rate of stroke, the rates of major cardiovascular events and death were lower with the salt substitute than with regular salt (15). Although we found no significant difference between the two groups in decrease of both baPWV and ABI, intragroup comparison showed LSSG significantly reduced in baPWV and ABI. Based on the ESH/ESC guidelines, we believe that long-term use of low-sodium formulations and CM-DASH diets can improve arteriosclerosis and reduce the risk of cardiovascular disease. Studies have shown that the DASH diet may be related to reduced PWV, and in salt-sensitive participants, the low-sodium DASH diet reduced vascular stiffness more than DASH did (16). In a prospective cohort study, daily dietary Na intake and Na:K levels were significantly positively correlated with increased baPWV levels (17). Na may reduce arterial compliance by inducing transforming growth factor (TGF)-β (18), and increase the bioavailability of antioxidant nitric oxide (NO) by decreasing the atherosclerotic process (19). Potassium can improve arterial stiffness by inhibiting free radical formation in vascular endothelial cells and macrophages, vascular smooth muscle cell proliferation, platelet aggregation and arterial thrombosis (20). In addition, DASH diet is rich in anti-inflammatory factors (including unsaturated fatty acids, vitamin C, magnesium, and dietary fiber), which can reduce the expression of serum inflammatory factors IL-6 and C-reactive protein (CRP), thereby delaying and improving atherosclerosis (21).
Lipid metabolism disorder is the most important pathological basis of atherosclerosis. Dyslipidemia can cause vascular endothelial cell dysfunction, which leads to thickening and stiffening of the intima and hypertrophy of the vascular wall, and finally formation of lipid streaks and progression to atherosclerotic plaques (22). Currently, a series of DASH diet intervention trials have found significant reductions in TC, LDL-C, HDL-C, and apolipoprotein a1 in the DASH diet group compared with the control group (23,24), but there are few studies on the atherosclerosis-related indices which are mainly based on whether lipoprotein ratios can be used as potential biomarkers for the early diagnosis of cardiovascular disease (25). In our study, LSSG showed significant reductions in TG/HDL-C ratio and AIP. This indicated that eight weeks of low-sodium salt and CM-DASH diet can improve atherosclerosis by improving lipid metabolism.
Twenty-four-hour urinary excretion showed that both the LSSG and NSSG had the lowest sodium intake at week 4, with a slight increase at week 8, which may indicate better adherence to the CM-DASH diet and low-sodium formulation in the first four weeks than in the last four weeks. A meta-analysis study shows that the participants have low compliance with the DASH dietary pattern, which may be related to the price of ingredients, dietary preference of the population, food availability and dietary taste (26-28). Although localized the DASH diet, we still recommend low-fat milk, whole wheat bread and other foods that are not accepted by Chinese residents in consideration of the balance of nutrients. In addition, although we recommend avoiding condiments like soy sauce and watercress, some patients said they still use condiments.
The low-sodium salt applied to CM-DASH diet can improve arteriosclerosis and reduce the risk of cardiovascular disease. Further research with an extended follow-up is needed.















