INTRODUCTION
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by impaired social communication and repetitive behaviors and restricted interests (1). It is estimated that 1 % of the world population has ASD, and based on this projection, Brazil must have about 2 million individuals with autism, although there are no official data in the country (2).
The etiology of ASD includes a multifactorial inheritance associated with genetic, biological and environmental risk factors in an additive feature combination (3,4). Inflammation, immune dysfunction, and the interaction between these factors, have been linked to both the etiology and the severity of symptoms, being observed since the fetal phase and at different stages of the life cycle in individuals with autism (5-7).
Studies show that children and adolescents with ASD have a higher level of proinflammatory cytokines and an immune response characterized by a predominance of monocytes in the leukogram. This evidence indicates a chronic inflammatory state, particularly in those with greater behavioral impairment (4-9).
It is known that overweight is an independent factor associated with increased inflammatory activity and immune dysfunction (10-15). Overweight is a nutritional disorder found in high prevalence in children and adolescents with ASD when compared to those with typical development (10-16). In addition, studies have observed that these patients show greater enjoyment when eating and a lower capacity to respond to satiety (16), and tend to eat to deal with different emotional states of joy, anxiety, and stress (10,11).
One of the pathways of investigation of the immune system is the analysis of white blood cells, especially monocytes, through a hemogram, a low-cost and low-complexity blood test (6,8). However, few studies have assessed immune response through these cells in individuals with autism, especially in the presence of conditions that predispose them to increased inflammatory activity. The study objective was to investigate the association between nutritional status and monocyte count in children and adolescents with ASD. To our knowledge, this is the first study nutritional status and immune system in this group of patients.
METHODS
A cross-sectional study was carried out at the Neurodevelopment Center of the Faculty of Medicine of the Federal University of Pelotas, in the city of Pelotas, state of Rio Grande do Sul, Brazil. Patients diagnosed with ASD between 3 and 18 years, regularly monitored by a neuropediatrician and with no medical diagnosis of genetic syndrome, neuropathy or congenital heart disease were recruited from October 2018 to March 2020. The study patients had follow-up visits to the neuropediatric service, and had already been evaluated and diagnosed there. Follow-up visits occurred on average 3 times a year. The neuropediatric service is characterized as a specialized outpatient clinic of the Brazilian Unified Health System, a free public service of universal access in Brazil. The patients had not received previous nutritional counseling or assistance. Most patients were from the city of Pelotas and cities in the southern region of Brazil, since the service is a regional reference for neuropediatrics.
Ninety-seven patients were eligible and of these, all caregivers expressed interest in participating in the research; 22 patients failed to provide blood samples due to difficulty in drawing it, and another 7 did not complete the Children's Eating Behavior Questionnaire (CEBQ), representing a loss of 30 %. Additionally, presence of any allergy, neoplasia or infection at the time of collection of blood samples were considered losses in the present study, but no such cases were reported. A total of 68 patients were included in the present study.
The administration of the questionnaires and the performance of the anthropometric measurements were conducted by research dietitians previously trained for the study. The interviews were conducted with the presence of the patient's main caregiver, identified according to the time spent with the child or adolescent. In most cases, the child's caregiver was the mother (98 %).
The outcome studied was plasma monocyte count. For this purpose, a 5-mL blood sample was obtained by venipuncture in the morning, after fasting, at a certified clinical analysis laboratory. The hemogram analysis was performed by electrical impedance, using the Coulter principle, following the instructions established by the equipment manufacturer (Mindray®, China). The monocyte number was expressed per cubic millimeter (mm3). The leukogram was expressed as an absolute value of each type of leukocyte (neutrophil, monocyte, lymphocyte, and eosinophil) of blood and a relative value considering the total leukocyte count as a reference (100 %).
The exposure was nutritional status, classified according to BMI-for-age in z-score, as proposed by the WHO in 2006 and 2007 (17). For anthropometric assessment, patients were weighed in light clothing on a digital scale (TRENTIN®, Brazil) with a capacity of 150 kg and a precision of 100 g. Height was obtained with a vertical stadiometer attached to the scale with 213 cm and a precision of 0.1 cm. The Anthro® and Anthro Plus® software were used to calculate the z-scores. The subjects were divided into two comparative groups, those without overweight were those with BMI ≤ +1 z-score, and those with over- weight were those with BMI > +1 z-score.
Eating behavior was assessed using the Children's Eating Behaviour Questionnaire (CEBQ) (18), translated and validated into Portuguese. This is a subjective scale that was answered by the caregivers. The scale has 35 questions divided into eight subscales, which are divided into two domains: I) behaviors that reflect “interest in food”, composed of the subscales: a) enjoyment of food, b) food responsiveness, c) desire to drink, and d) emotional overeating; and domain II) behaviors of ‘‘disinterest in food'', composed of the subscales: a) emotional undereating, b) satiety responsiveness, c) slowness in eating, and d) food fussiness. The questionnaires were answered using a 5-point Likert scale, according to the frequency with which they display each behavior. The instrument's score ranges from 1 to 5: never (1), rarely (2), sometimes (3), often (4), and always (5). Subsequently, the scores of the questions belonging to the same subscale were added up, obtaining the mean value and standard deviation (SD) for each one. This result was used dichotomously in the analyses (below the mean/equal to or higher than the mean).
The sociodemographic and clinical covariates used to describe the sample were: maternal education, obtained in complete years and categorized as elementary education (≤ 8 years of schooling) and secondary education (≥ 9 years of schooling); total family income collected in Brazilian real (R$), converted to US$ and categorized as < 209 and ≥ 209 US$; patient age calculated from the date of birth and categorized into the following ranges: ≤ 5, 6 to 10 and ≥ 11 years; patient sex (male or female), and ethnicity (white or black). Antipsychotic use was categorized into ‘Yes' or ‘No' for any antipsychotic. Sleeping hours per day was collected in hours and minutes and categorized into < 7 and ≥ 7 hours/day.
Data collected were double-entered in the EpiData® software (EpiData®, version 3.1; The EpiData Association, Odense, Denmark, 2003-2005). The two datasets entered were compared and any inconsistencies were solved by checking the paper questionnaire. Statistical analyses were carried out in the statistical package Stata® (Stata Statistical Software, version 13. College Station, TX, USA). The descriptive analyses are presented as mean, standard deviation for continuous variables, and as proportions for the categorical variables. The distribution of variables was evaluated using the Shapiro-Wilk test, since the main outcome followed a symmetrical distribution. The comparison between two categories was performed using Student's t-test, and three or more categories were performed using one-way ANOVA. The mean absolute value of the total and differential leukocyte count was stratified by age group and compared to the mean reference value according to the Brazilian Society of Clinical Analyses (19), using Student's t-test for one sample.
Linear regression was used to investigate the association between nutritional status and monocyte count. For that, a global significance test was performed and, when the value of F-test was significant, a second stage was carried out with the individual significance tests. Each eating behavior CEBQ subscales, sociodemographic and clinical as variates described above were potentially considered to be entered in the adjusted models. However, only the subscale “emotional overeating” was kept in the final regression model, since its β value was > 0.2 and p < 0.05. The adjusted R² value was used to predict monocyte count variability attributed to overweight, adjusted for “emotional overeating”. The level of statistical significance was set at p < 0.05.
The research project was approved by the Research Ethics Committee of the Faculty of Medicine of the Federal University of Pelotas, under protocol number 2.835.793. Informed consent was freely obtained after all clarifications provided, signed by the parents or guardians of the participants.
RESULTS
The mean age of participants was 8.6 ± 3.3 years, the majority were male (79 %) and white (76 %). Most mothers (61 %) had secondary or college education and a family income above US$ 209 (70 %). Most children and adolescents slept more than 7 hours a day (84 %) and used antipsychotic drugs (62 %), especially risperidone (57 %). Regarding the nutritional status, most were overweight (66 %). Mean monocyte count was statistically higher in overweight patients (522 ± 211/mm³) when compared to non-overweight patients (394 ± 142/mm³) (Table I).
Table I. Absolute monocyte count according to sociodemographic characteristics, antipsychotic use and nutritional status of children and adolescents with autism spectrum disorder. Neurodevelopment Center, Pelotas, Brazil, 2018-2020 (n = 68).
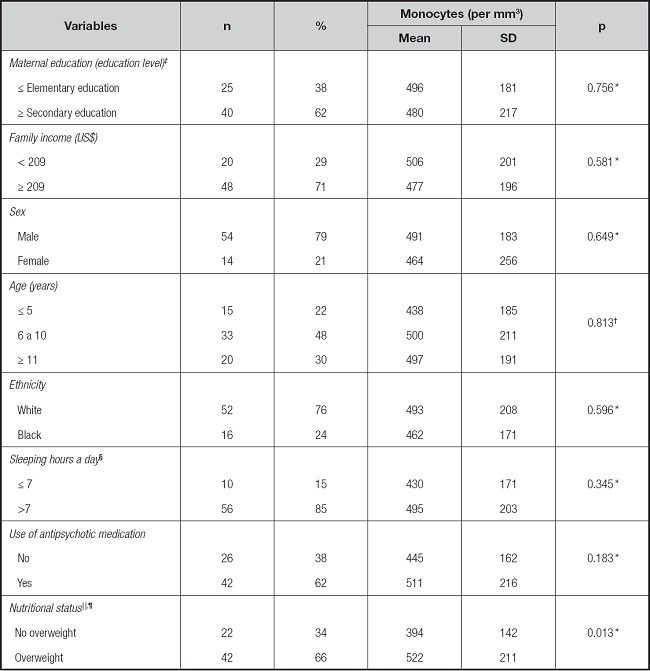
*p-value refers to Student's t-test.
†p-value refers to ANOVA test.
‡Variable with three missing data.
§Variable with two missing data.
||Z-score body mass index classification (BMI-Z) for age; absence: BMI-Z ≤ +1 Z-score; presence: BMI-Z > +1 Z-score.
¶Variable with four missing data.
Mean total leukocyte, neutrophil, monocyte, lymphocyte, and eosinophil counts (per mm³) were 8,857; 4,483; 485; 3,422 and 377, respectively, and did not differ statistically from those used as reference according to age and sex (19) (Table II).
Table II. Characteristics of the leukogram according to the age group category of children and adolescents with autism spectrum disorder. Neurodevelopment Center, Pelotas, Brazil, 2018-2020.
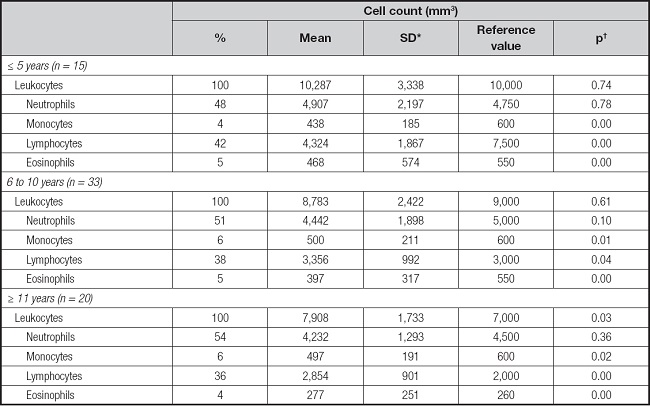
*Standard deviation..
†p-value refers to one-sample Student's t-test.
The CEBQ subscales for enjoyment of food, food responsiveness, desire to drink, emotional overeating, emotional undereating, satiety responsiveness, slowness in eating and food fussiness showed a mean (95 % CI) of 3.5 (3.16-3.83); 3.07 (2.71-3.43); 3.07 (2.71-3.43); 2.73 (2.44-3.02); 2.57 (2.26-2.88); 2.70 (2.52-2.87); 2.48 (2.31-2.66); and 2.89 (2.78-3.0), respectively. The association between monocyte counts (per mm3) and CEBQ scores found that monocyte counts were statistically significantly higher in patients with above average scores on the subscales of food responsiveness (552 ± 232 vs. 420 ± 137) and emotional overeating (581 ± 247 vs. 452 ± 126) subscales, compared to those with below-the-mean scores on these two subscales. As for emotional undereating (538 ± 218 vs. 430 ± 161) and slowness in eating (536 ± 214 vs. 428 ± 165) the monocyte count was higher among patients with below-the-mean scores compared to above-the-mean patients (Table III).
Table III. Absolute monocyte count according to the score in the subdomains of the CEBQ scale in children and adolescents with autism spectrum disorder. Neurodevelopment Center, Pelotas, Brazil, 2018-2020 (n = 68).
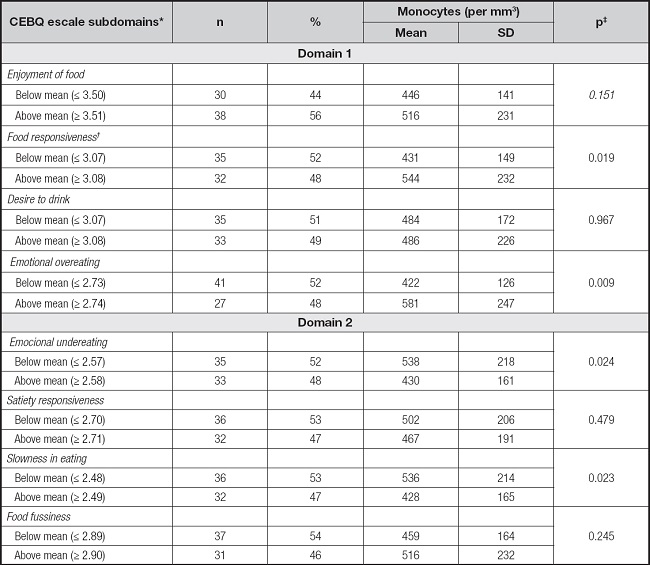
*Children's Eating Behaviour Questionnaire.
†Variable with one missing data.
‡p-value refers to Student's t-test.
In the unadjusted linear regression, monocyte count was higher in overweight patients (B: 64.0; 95 % CI, 13.9 to 114.1; β: 0.30, p = 0.01), compared to non-overweight. This result was kept significant even after adjustment for the subscale of emotional overeating (B: 37.0; 95 % CI, 17.1 to 91.3; β: 0.29; p = 0.02) (Table IV). The variability of the monocyte count attributed to overweight was 14 %, after adjustment for higher emotional overeating (Table IV).
Table IV. Linear regression of the monocyte counts and nutritional status of children and adolescents with autism spectrum disorder. Neurodevelopment Center, Pelotas, Brazil, 2018-2020 (n = 64).
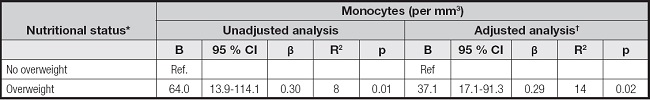
*Variable with four missing data;.
†Adjusted for the subdomain “emotional overating” of the Children's Eating Behaviour Questionnaire. B: linear regression constant; CI: confidence interval; β: linear regression coefficient; R2: adjusted R-square; p-value
DISCUSSION
This study observed that children and adolescents with ASD have an increase in the number of monocytes associated with nutritional status. In these patients, overweight significantly explained the increase in the number of monocytes. Understanding this relationship is essential, since modifiable risk factors, such as diet and overweight, can be controlled and even mitigate the monocyte-mediated inflammatory response in patients with ASD. Furthermore, the presence of overweight explained 14% of the variability in the number of monocytes (Fig. 1). Other studies have also found a higher number of monocytes in neurotypical overweight children, demonstrating the relationship between a low-grade inflammatory state and overweight (11,20-21). To our knowledge, this is the first study to describe the impact of overweight on higher monocyte count in individuals with ASD.

Figure 1. Relation between overweight in children and adolescents, and ASD and monocyte count. Neurodevelopment Center, Pelotas, Brazil (2018-2020). Note: In a sample of 68 patients (3 to 18-year-olds) the presence of overweight resulted in a 14 % increase in monocyte count.
Monocytes are a type of leukocyte, originating in the bone marrow, found in blood and tissues, which are part of the innate and adaptive immune response, directly regulating the production of inflammatory cytokines such as interleukins 1 and 6 (IL-1, IL-6) and the tumor necrosis factor α (TNF-α) (22,23). The increase in monocytes contributes to the phagocytosis of materials foreign to the body and to the production of cytokines that recruit other inflammatory cells (6,24).
The increase in the monocyte count plays a central role in the underlying inflammatory response to various diseases and health problems, relating to a chronically established process (11). Previous studies indicates a higher monocyte count in children and adolescents with ASD compared to neurotypical ones, in addition, the increase of these cells was associated with greater behavioral impairment in autism (6,25,26).
Studies have shown that the eating behavior of individuals with ASD can be exacerbated, compared to that of neurotypical children, especially taking into account that compulsion is the most frequent comorbidities (10,16,27). In addition, the amplitude of the severity of symptoms on the ASD is a relevant determinant of behavior, including eating behavior (9). A priori emotional overeating may reflect the impairment in behavior, mediated by the inflammatory process established since the early stages of development in ASD. However, it may be related to inadequate eating habits, formed by a set of genetic and environmental influences, and to the eating behavior acquired since the first years of life (5,6,26,27).
Children and adolescents with ASD have the habit of frequently ingesting sugary drinks (28), in addition to eating more quickly, tending to prefer unhealthy meals, as observed in studies that described the high frequency of foods such as processed meats, snacks and cookies (28). Thus, a greater difficulty in dealing with their emotional state combined with a diet high in calories and insufficient in micronutrients are factors strongly associated with overweight in these individuals (10,16,28,29).
A chronic low-grade inflammatory state, resulting from the systemic increase in adipokines, is also found in overweight individuals (12,14). The increase in white adipose tissue produces adipokines that, when reaching other tissues, recruit and stimulate the activation of immune system cells, including monocytes (20,24). These migrate to the adipose tissue, where they mature into macrophages, exacerbating the production and secretion of inflammatory cytokines such as TNF-α and IL-6 (12,24).
The combination of increased adiposity, greater emotional overeating, and increased inflammatory response are aspects that greatly compromise the health of those patients in the short and long term (10,11,16). Especially when considering that low-grade inflammation is the underlying condition related to several diseases, such as diabetes, non-alcoholic fatty liver disease and cancer (12).
In the present study, the general profile of white blood cells was stratified by age and it was similar to that of the reference population (19), and despite the significant increase in monocytes, no monocytosis was observed (≥ 1000 cells/mm³) (Table I). The lymphocytes count showed a statistically significant relationship with age, where the number of these cells was lower in the highest age categories (data not shown). This result was attributed to a physiological phenomenon due to the maturation of immune cells according to age (30).
The study's strengths include its internal validity through the methodological rigor for patient selection, the application of standardized instruments, a trained team and the use of a biological marker of the immune response. These aspects are relevant for comparing the results with population groups similar to those in the present study. The present study has some limitations that should be considered when interpreting the results, such as the lack of information about the severity of the ASD symptoms and the loss of patients due to the difficulty in collecting blood. The external validation of results is limited to population groups similar to that of the present study. Finally, the potential bias of caregivers' interpretation by their children or adolescents should be considered, even though they are the best source of information for data collection.














