INTRODUCTION
Cancer is considered as a term that encompasses more than 100 diseases, which are characterized in common by disordered cell growth being a major public health problem (1). Its causes are multifactorial, encompassing cultural, genetic, environmental, socioeconomic and lifestyle risk factors (alcohol consumption, smoking, unhealthy diet, physical inactivity) (2).
Until the time of diagnosis, approximately 84 % of cancer patients have unintentional weight loss (3). Among the factors associated with increased nutritional risk is the lack of early and effective detection of a patient’s nutritional risk (4), and the resulting complications, such as reduced tolerance to therapeutic measures, higher risk of mortality and increased hospital stay and higher associated costs (5,6).
In view of the poor prognosis that malnutrition can cause in patients diagnosed with cancer, it is extremely important to use an effective nutritional screening tool. Thus, the nutritional risk of these patients could be identified as early as possible, in order to improve their nutritional status and their quality of life through adequate and early nutritional intervention (7).
The NUTRISCORE nutritional screening tool was recently developed in Spain. The version used was in the English language, as validated in Portuguese language translation (8). This screening tool evaluates the nutritional risk of a cancer patient through involuntary weight loss in the previous three months, the reduction of food intake in the previous seven days, as well as the identification of the type of neoplasm and the antineoplastic treatment undergone by these patients (3). Among the advantages of applying the NUTRISCORE are its practicality, ease and speed of application, in addition to its good correlation with the patient’s subjective evaluation on the Subjective Global Assessment Produced by the Patient (ASG-PPP), considered as the gold standard for this group in Brazil (6,7).
To this writing, in Brazil, the NUTRISCORE has not been used with hospitalized cancer patients, therefore, the present study aims to analyze the NUTRISCORE tool, translated and adapted to the Brazilian population, as a predictive screening of longer hospitalization time as well as weight loss while in hospital.
METHODS
This is a prospective longitudinal study, which aimed to analyze the predictive value of NUTRISCORE in relation to greater weight loss and longer hospitalization of cancer patients. Thus, it is expected that patients at nutritional risk will have a longer hospital stay and greater weight loss during hospitalization.
In the first stage, the translation of the NUTRISCORE from the original version (English) to Portuguese was carried out following the methodology proposed by Beaton et al. (2000) (9), with adaptations, which consisted of six stages: initial translation, synthesis of translations, back-translation, pre-test and evaluation of the cultural adaptation process.
The initial translation comprised two translations of the original tool from English to Portuguese. These were carried out independently by two qualified professionals in the linguistic area, sworn translators, and assisted by an experienced professional in the thematic area (Nutrition). In the second stage, the professionals participating in the first stage reconciled the two translated versions, thus generating a single document. The back-translation stage took place with the translation of the document generated in Portuguese into English, through a translator who was also sworn, not having access to the original document, avoiding information bias. The fourth stage gathered, online, all the professionals involved in the previous stages to finalize the pre-final version of the tool, observing the semantic, idiomatic, cultural and conceptual equivalence between the original version and the Portuguese version.
A pre-test was carried out to verify the understanding of the content of the translated tool (observing doubts regarding the questionnaire). The translated tool was also given to health professionals, so that they could read the tool and make suggestions, aiming to improve understanding of the questionnaire. The last stage, finally, comprised the elaboration of the final version of the tool, taking into account the questions that had been raised in the fifth stage.
The second stage of the research was application of the NUTRISCORE tool to assess whether patients at nutritional risk would have greater weight loss and longer hospital stays. The stage of the research was carried out at the Hospital do Cancer de Pernambuco (HCP), located in the city of Recife - PE, with participating patients of both sexes, and over 20 years of age. Pregnant women, amputee patients, patients with edema, patients unable to walk, patients with Karnofsky Status (KPS) 10, in the terminal stage of the disease, transferred to the Intensive Care Unit (ICU) and with mental disorders (information obtained from medical records) were excluded from the study. The number of patients in the study took into account previous studies by the research group with cancer patients.
In order to associate the nutritional risk according to the NUTRISCORE results with the length of hospital stay and the weight loss of the patients, the nutritional screening of the patient was initially performed with the NUTRISCORE screening tool; later, the patients were classified as “at nutritional risk” for those who presented a score ≥ 5, and “no nutritional risk” for those who scored < 5. The nutritional screening was carried out within the first 48 hours of the patient’s hospitalization.
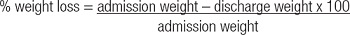
The length of hospital stay was stratified into < 7 days and ≥ 7 days. Weight loss, in turn, was calculated absolutely, in kilograms (kg) and in relative terms (%), here, to identify patients who had weight loss < 2 % and ≥ 2 % to later be associated with their NUTRISCORE results.
Absolute weight loss (kg): discharge weight (kg) – admission weight (kg)
Data were entered into the Epi-info program, version 6.04, and statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 28.0 program. Categorical variables were expressed in absolute values and percentages (n; %) and quantitative variables in mean and interquartile range. Fisher’s exact test was performed to compare proportions between variables, with significance set at p < 0.05.
This research was approved by the Research Ethics Committee of the Hospital Involving Human Beings of the Hospital do Câncer de Pernambuco, in accordance with Resolution 466/12 of the National Health Council (Certificate of Presentation of Ethical Appreciation [CAAE]: 40861520.0.0000.5205), and concerns only studies of those patients who met the eligibility criteria and signed the informed consent form.
RESULTS
The NUTRISCORE tool was independently translated by two sworn translators. An analysis of the different translations showed few divergences between them. Despite the differences seen the two translations, the interpretation of the tool is considered similar when replacing different terms when this does not affect the result obtained and, consequently, the usefulness of the tool, which is quite interesting in clinical practice.
In the translation synthesis stage, the translators agreed to analyze which terms would remain in the final version. As this document would be used by cancer patients at a later date, the final choice of terms was based on their frequency as found in other screening tools. The last stages of the first stage of the research (the back-translation and the pre-test) did not show any need to change the terms generated in the previous stages. Figure 1 has the NUTRISCORE tool in its final version, after its translation and cultural adaptation.

Figure 1. NUTRISCORE Nutritional Screening Tool translated and adapted for the Brazilian population, 2022.
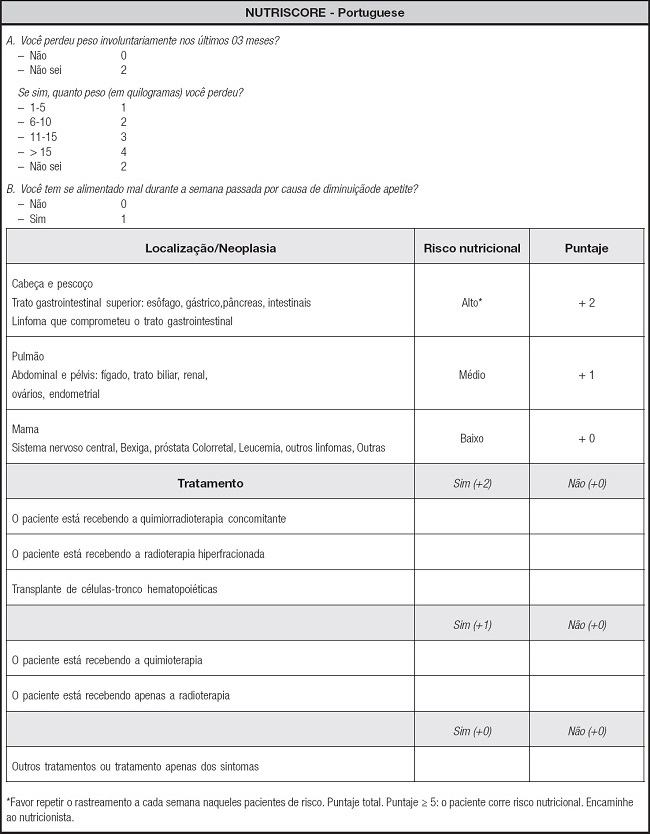
Figure 1 (cont). NUTRISCORE Nutritional Screening Tool translated and adapted for the Brazilian population, 2022.
The second stage of the research included 101 adult (61.4 %) and elderly (38.6 %) patients, 56 (55.4 %) males and 45 (44.6 %) females, with an average age of 51.62 ± 13.74 years. The prevalence of nutritional risk given by NUTRISCORE was 63.3 % in the studied patients.
Regarding the primary site of the tumor, several types of cancer were found. Gastrointestinal (GI) tumors were more frequent (31.6 %), followed by hematological tumors (22.7 %), gynecological cancers (18.8 %), breast (14.8 %), genitourinary system (7.9 %) and head and neck (3.9 %). With regard to the antineoplastic treatment used by the patients, there was a higher prevalence of chemotherapy alone (64.3 %), followed by chemotherapy together with radiotherapy (23.7 %). Some patients not undergoing treatment at the time were included. These had already finished the therapeutic radio/chemotherapy and were awaiting oncological surgery (12.8 %). Patients undergoing treatment with radiotherapy alone were not included.
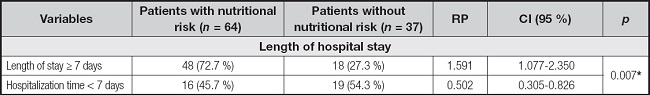
Tables I and II show the association between the presence and absence of nutritional risk identified by the NUTRISCORE tool and weight loss and length of stay in these cancer patients. As shown in table I, it is noted that the presence of nutritional risk was associated with greater in-hospital weight loss (loss ≥ 2 %), with a prevalence ratio of 1.970 (p = 0.001). The same behavior was seen between the longest hospital stay and patients at nutritional risk, with a prevalence ratio of 1.591 (p = 0.007), in table II.
Table I. Association between nutritional risk by the NUTRISCORE tool and the variable weight loss in cancer patients, 2022.

RP: prevalence ratio; CI: confidence interval.
*p ≤ 0.05.
DISCUSSION
The population profile of the present study was very similar to that of other studies with cancer patients, where a higher prevalence of adults and male patients were also present in their sample (10,11). With respect to age, other authors have reported that, in Brazil, both the incidence rate and the prevalence rate of all types of cancer are higher in the elderly population (12).
This is the first study to undergo a translation and cultural adaptation of a diagnostic tool in another language of the NUTRISCORE tool, and subsequently apply it as a predictor of longer hospital stay and greater weight loss during hospital stay. The use of this tool is extremely important to enable application of this nutritional screening with this public. This nutritional screening tool has been considered as simple, fast, and easy to apply and to interpret, which corroborates the finding of the first stage in the present research, where in the translation and cultural adaptation, adjustments related to terms that were difficult to interpret were not necessary or considered to be contradictory (6,7).
The NUTRISCORE assessment tool was recently developed in Spain to assess the nutritional risk of cancer patients. It correlates well with the ASG-PPP, which is considered as the gold standard for this group in Brazil (6,7). Several authors have already applied this tool to cancer patients, including comparison of prevalence of nutritional risk by different screenings, including NUTRISCORE, in outpatient cancer patients (7); relating to NUTRISCORE and ASG-PPP to the survival of patients with gastric cancer (13); and aiming to evaluate the concordance of NUTRISCORE with Malnutrition Universal Screening Tool (MUST), as well as to show its predictive value in relation to patient outcome in a hospital in Spain (14). However, none have observed the predictive value of NUTRISCORE in relation to weight loss and length of hospital stay.
The prevalence of nutritional risk identified by NUTRISCORE in the present study was 63.3 %, corroborating with another study also carried out in Brazil, when assessing the nutritional risk of cancer patients by ASG-PPP (rate of 65.1 %) (15), and also being very similar to the Brazilian Oncological Nutrition Survey, which identified nutritional risk in approximately 66.4 % of hospitalized cancer patients (16).
The early and assertive identification of patients who are at nutritional risk is a key factor in ensuring a satisfactory prognosis for cancer patients. Through this identification, it is possible to carry out an adequate nutritional intervention, to prevent risk or recover their nutritional status, minimizing the deleterious effects of antineoplastic treatments, in addition to reducing the length of hospital stay and associated costs (17-19).
Among the factors that are related to a higher nutritional risk in cancer patients are the metabolic alterations caused by the tumor itself (causing unintentional weight loss and reduced food consumption,) in addition to the location of the primary site of the tumor and the antineoplastic treatment used by patients (6,20,21). All these factors are evaluated by NUTRISCORE, which is very efficient in obtaining a correct/real nutritional risk result, thus facilitating nutritional intervention and, subsequently, improving the patient’s prognosis.
The analysis of the reduction in food consumption identified by NUTRISCORE is essential, as this is a variable directly related to malnutrition. Changes in the gastrointestinal tract that hinder the consumption, digestion and absorption of nutrients are the main causes of this reduction, with symptoms such as diarrhea, nausea and vomiting, changes considered to be quite common among cancer patients (22,23). These patients may even have their nutritional status worsened when hospitalized, due to the high frequency of needing to fast for exams and/or procedures (10).
In relation to the type of tumor, authors report greater impairment in the nutritional status of patients with tumors located in the gastrointestinal tract, liver, head and neck and lung (24), corroborating the NUTRISCORE tool, which classifies these tumors as high or medium risk in relation to nutritional risk. The highest prevalence of gastrointestinal tract tumors (TGI) was also observed in the present study, and researches show that early nutritional intervention is essential in patients with GI and head and neck tumors, since most patients have dysphagia and/or obstruction of food passage, with these changes being major aggravating factors in the nutritional status (25,26).
With regard to antineoplastic treatment, the tool considers chemotherapy associated with radiotherapy, hyperfractionated radiotherapy, stem cell transplantation, followed by chemotherapy or radiotherapy alone to represent the greatest risks. As a large part of the patients in the studied sample were receiving chemotherapy as a current treatment, and were also affected by TGI cancers, this characteristic as recorded in the sample may have contributed to the high rate of nutritional risk among the patients studied.
The present study shows the risk of greater weight loss (PR = 1.970; p = 0.001*) and longer hospital stay (PR = 1.591; p = 0.007*) among patients at nutritional risk according to the NUTRISCORE tool. It can be seen that this tool proved to be a good predictor of longer hospital stays and greater weight loss among the patients studied. This result may be justified by the variables present in the screening.
A retrospective study conducted in Korea compared the ASG-PPP with the NUTRISCORE in relation to the outcomes shown by patients with gastric cancer. They observed that patients with higher scores in the NUTRISCORE had presented greater weight loss and lower frequency of meal consumption; in addition, it was considered that mortality was 3.84 times higher in patients whose NUTRISCORE score was ≥ 7, compared to those who obtained scores ≤ 4 in their screening (13). A limitation of this study was its retrospective model, in addition to having the screening carried out using data obtained from the patients’ medical records. However, this finding corroborates the present research, where more negative outcomes were observed in patients with higher nutritional risk due to NUTRISCORE tool.
Weight loss during hospitalization has multifactorial causes, such as fasting for procedures and exams, side effects of the tumor itself and antineoplastic treatment, including nausea, vomiting, reduced appetite, mouth and throat lesions, diarrhea and abdominal discomfort (27,28). However, there are hormonal changes that occur in the female body, especially in women undergoing chemotherapy, due to menopause and changes in the basal metabolic rate that stimulate weight gain by mobilizing brown adipose tissue (29).
When involuntary, the weight reduction seen in cancer patients facilitates the onset of cancer cachexia (30) and increases the difficulty of responding to antineoplastic treatment, in addition to being a predictor of longer hospital stays and increasing comorbidity and mortality rates among these patients (22). This highlights the importance of predicting the group of patients who are at risk of losing weight during their hospitalization and to avoid the common complications. Studies have also shown that longer hospital stays lead to greater weight loss among patients, showing that there is a direct correlation between longer prolonged hospital stay and weight loss (r = 0.470; p ≤ 0.001) (31).
Some limitations were seen in this research, such as candidate losses during collection, as some patients evolved to the ICU and others died. In addition to this factor, the research collection took place in the midst of a COVID-19 pandemic, and many patients were also contaminated by this disease and had to be excluded from the research forcing the research to be subsequently interrupted. However, despite all the limitations, important data were found in relation to the proposed objective.
According to the data obtained in this study, it can be concluded that the NUTRISCORE nutritional screening tool represents a good association of risk with greater weight loss as well as with longer hospital stay of cancer patients. Regarding the types of tumors involved, TGI-types were the most frequent. Chemotherapy was the most used treatment among patients. Thus, despite all the limitations seen, it was possible to observe the association between the studied tool and the analyzed outcomes. The authors suggest further studies using NUTRISCORE with hospitalized cancer patients, with the aim of later analyzing the possibility of using this instrument with a more widespread base.