INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an emerging respiratory disease that is caused by a novel coronavirus (first: 2019-nCov, then: SARS-CoV-2) and was first detected at the end of 2019 in Wuhan, China (1). The spread of COVID-19 has reached pandemic proportions and then became a global health emergency. Considering an increasing risk of overwhelming healthcare infrastructures, it is of great importance to identify reliable demographic, clinical and laboratory indicators which are needed to evaluate the length of hospital stay (LOS) of the disease, thus enabling stratified management of patients and optimize allocation of limited medical resources.
As the global COVID-19 pandemic has progressed, the number of patients with long-term persistent multiorgan symptoms and complications beyond the initial period of acute infection and illness is noteworthy (2-4). This group of symptoms was called “long COVID” by the World Health Organization (WHO) (2-4). Reports of the prevalence of long COVID range from 6.2 % to 87 % of COVID-19 survivors (1,5). Detailed risk factor evaluation is essential for the characterization of this syndrome.
Malnutrition has been recognized as an independent risk factor of a long LOS, high hospital costs, high rate of hospital readmission and adverse clinical events in patients with various disease spectrums (6-8). Appropriate nutrition is an essential component of intensive care management of patients with COVID-19 (9). Several studies have demonstrated that nutritional status was associated with disease severity and prognosis in patients with COVID-19 (10-16). However, few studies have focused on the predicted value of nutritional parameters on LOS and especially on the risk of long COVID in these patients.
Nutritional assessment in COVID-19 patients should be practical, noninvasive, and easy to perform. The Controlling Nutritional Status (CONUT) score is an efficient nutritional assessment tool which is calculated from three peripheral blood parameters: serum albumin level, peripheral lymphocyte count, and total cholesterol concentration (17). Compared with other comprehensive nutritional cores, the CONUT score helps evaluate not only protein reserves and calorie depletion but also immune defenses, which is clinically meaningful for patients with COVID-19. Therefore, the primary goal of this study was to elucidate the value of CONUT score on predicting LOS and the risk of long COVID in patients with COVID-19 in Wuhan.
MATERIAL AND METHODS
STUDY POPULATION
We retrospectively reviewed and analyzed 162 patients diagnosed with laboratory-confirmed COVID-19 and admitted to two designated isolation medical centers (Tumor Center of the Union Hospital Affiliated to Tongji Medical College and Eastern Courtyard of Renmin Hospital Affiliated to Wuhan University) from February 15, 2020 to March 31, 2020. Clinical outcomes were followed up to June 30, 2022. The protocol was approved by the Research Ethics Committee of the Fujian Medical University Union Hospital (project identification code 2020KY208).
COVID-19 was diagnosed according to the Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection published by the National Health Commission on February 4, 2020 (1). Severe cases were defined as either: respiratory rate > 30/min, or oxygen saturation ≤ 93 %, or PaO2/FiO2 ratio ≤ 300 mmHg (18). Patients cured were discharged when respiratory symptoms improved significantly with no fever for at least three days, obvious absorption of inflammation in pulmonary imaging, and SARS-CoV-2 nucleic acid was negative for negative results for at least two consecutive tests (48 hours interval at least).
Exclusion criteria were as follows: six patients who died during their hospitalization (two patients died of massive cerebral hemorrhage, one patient died of unidentified hypertonic dehydration within 24 hours of admission, and three patients died of multisystem organ failure in Intensive Care Unit); one patient who lacked a serum albumin, peripheral lymphocyte count or total cholesterol measure; and four patients who were lost to follow-up. At last, a total of 151 patients were selected for final analysis.
EVALUATION OF CONUT SCORE
Baseline CONUT score was calculated from serum albumin levels, total cholesterol levels and total lymphocyte counts, which were measured on admission: serum albumin ≥ 3.5 g/dl = 0 points, 3.0-3.4 g/ dl = 2 points, 2.5-2.9 g/dl = 4 points and < 2.5 g/dl = 6 points; total cholesterol ≥ 180 mg/dl = 0 points, 140-179 mg/dl = 1 point, 100-139 mg/dl = 2 points and < 100 mg/dl = 3 points; and total lymphocyte count ≥ 1,600/ml = 0 points, 1,200-1,599/ml = 1 point, 800-1,199/ml = 2 points and < 800/ml = 3 points (18). CONUT scores range from 0 to 12. An individual with higher scores indicates worse nutritional status. Patients in the present study were also divided into three groups based on their CONUT score: low-CONUT (0-1, n = 50), mild-CONUT (2-4, n = 75), high-CONUT (≥ 5, n = 26).
DEFINITION OF LONG COVID
The long COVID was defined as “the continuation or development of new symptoms three months after the initial COVID-19 infection, with these symptoms lasting for at least two months with no other alternative diagnosis” by the WHO (3). The common symptoms defined as long COVID in this study include fatigue, dyspnea, insomnia, concentration or memory deficit, mood changes, chest and joint pains, palpitations, myalgia, smell and taste dysfunctions, cough, headache, rash or hair loss, persistent abdominal pain, and diarrhea (3).
DATA COLLECTION
We extracted demographic characteristics, clinical symptoms and signs, laboratory findings and medications from electronic medical records during hospitalization. Included patients were followed up for two years from three months after the onset of SARS-CoV-2 infection. Telephone interviews were conducted by uniformly trained investigators to complete the questionnaires to collect data on the long COVID symptoms.
STATISTICAL ANALYSES
Data normality was analyzed using the Kolmogorov-Smirnov test. Normally distributed continuous variables were presented as mean ± SD, and continuous variables with a skewed distribution were expressed as median and interquartile range (25th to 75th percentile). Categorical and ordinal variables were presented as numbers and percentages. Comparison among the groups was performed using one-way analysis of variance test, Kruskal-Wallis test or Chi-squared test as indicated. Spearman’s rank correlation coefficient and multivariate linear analysis was employed to assess the correlation between the variables and LOS. The association between different CONUT grade and long COVID was evaluated by Kaplan-Meier survival curves with log-rank test and Cox proportional hazard models after adjustment for potential confounding covariates. p values less than 0.05 (two-tailed) was considered as statistical significance. All data were analyzed using SPSS 22.0 for windows (SPSS Inc., Chicago, Illinois, United States).
RESULTS
BASELINE CHARACTERISTICS AND INTERGROUP COMPARISONS
Baseline characteristics stratified by CONUT score categories were shown in table I. The median (range) CONUT score was 2 (1-4) points. The high-CONUT group had significantly lower albumin, lymphocyte (LY), total cholesterol (TC), hemoglobin (Hb), low density lipoprotein cholesterol (LDL-c), and high density lipoprotein cholesterol (HDL-c) levels, and significantly higher fasting blood glucose (FBG), creatinine (Cre), brain natriuretic peptide (BNP), C-reactive protein (CRP) and high-sensitivity cardiac troponin I (hs-cTnI) levels than the low-CONUT group. The overall LOS was significantly longer in the high-CONUT group than in the low-CONUT group (Table I). Similar differences were observed between the mild-CONUT and low-CONUT group (Table I). Of the 151 patients, 111 (74 %) were severe cases. Severe cases were more prevalent in the high-CONUT and mild-CONUT group.
Table I. Baseline characteristics and intergroup comparisons.
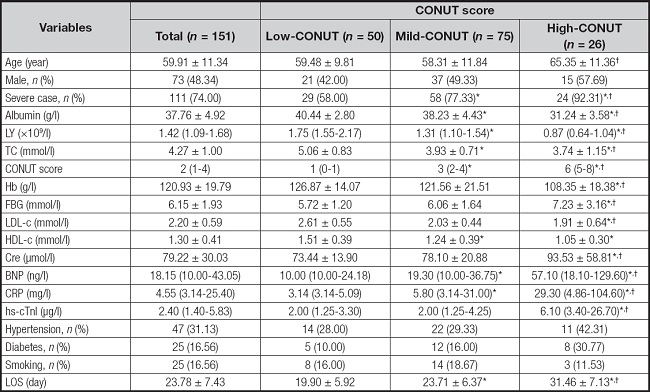
All values are presented as mean ± SD, median value (interquartile range) or n (%).
CONUT: Controlling Nutritional Status; LY: lymphocyte; TC: total cholesterol; Hb: hemoglobin; FBG: fasting blood glucose; LDL-c: low density lipoprotein cholesterol; HDL-c: high density lipoprotein cholesterol; Cre: creatinine; BNP: N-terminal pro-brain natriuretic peptide; CRP: C-reactive protein; hs-cTnI: high-sensitivity cardiac troponin I; LOS: length of hospital stay.
*p < 0.05 compared to low-CONUT group;
†p < 0.05 compared to mild-CONUT group.
SPEARMAN’S CORRELATION ANALYSIS
Spearman’s correlation analysis was explored to assess the correlation between variables and LOS. The results showed that CONUT scores were positively correlated with LOS (Table II). Besides, albumin, LY, Hb, HDL-c, BNP, CRP and hs-cTnI levels were also significantly correlated with LOS.
Table II. Spearman’s rank correlation coefficient between variables and LOS.
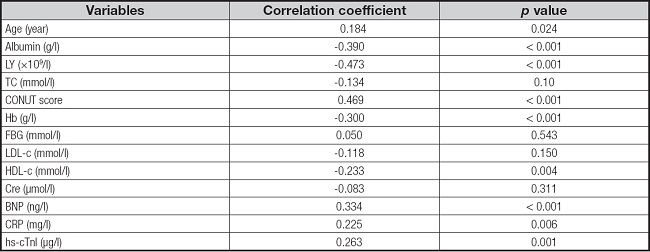
CONUT: Controlling Nutritional Status; LY: lymphocyte; TC: total cholesterol; Hb: hemoglobin; FBG: fasting blood glucose; LDL-c: low density lipoprotein cholesterol; HDL-c: high density lipoprotein cholesterol; Cre: creatinine; BNP: N-terminal pro-brain natriuretic peptide; CRP: C-reactive protein; hs-cTnI: high-sensitivity cardiac troponin I; LOS: length of hospital stay.
MULTIVARIATE LINEAR REGRESSION ANALYSIS
Multivariate linear regression analysis was performed to determine the independent parameters correlated with LOS. The result showed that CONUT score is the only independent determinant of LOS (Table III).
Table III. Multivariate linear regression analysis for the determinants of LOS.

CI: confidence interval; CONUT: Controlling Nutritional Status; LY: lymphocyte; TC: total cholesterol; Hb: hemoglobin; FBG: fasting blood glucose; LDL-c: low density lipoprotein cholesterol; HDL-c: high density lipoprotein cholesterol; Cre: creatinine; BNP: N-terminal pro-brain natriuretic peptide; CRP: C-reactive protein; hs-cTnI: high-sensitivity cardiac troponin I; LOS: length of hospital stay.
SURVIVAL ANALYSES
In total, 53 (35.10 %) patients with long COVID were identified during the two-year follow-up, and most cases (83.02 %) occurred in 4-10 months after the onset of COVID-19 infection. Cumulative incidence of long COVID categorized by CONUT grade was shown in figure 1. The cumulative incidence of long COVID was 14 % in the low-CONUT group compared to 38.67 % and 65.38 % in the mild-CONUT and high-CONUT group. Kaplan-Meier cumulative survival curves showed significant differences in the incidence of long COVID among patients with different CONUT group (Log-rank p < 0.01) (Fig. 1). Cox proportional hazards models were applied to evaluate the risk of long COVID according to CONUT grade. As shown in table IV, both crude and adjusted models showed significantly increased risk for development of long COVID in the high-CONUT group compared with that in the mild-CONUT and low-CONUT group.
Table IV. HRs and 95 % CI for long COVID according to CONUT grade in Cox proportional hazards models.
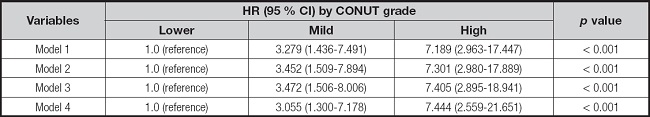
Model 1: non-adjusted model. Model 2: adjusted for age and sex. Model 3: further adjusted for severe case. Model 4: further adjusted for cardiac biomarkers including BNP, CRP, and hs-cTnI.
CI: confidence interval; CONUT: Controlling Nutritional Status; HR: hazard ratio; BNP: N-terminal pro-brain natriuretic peptide; CRP: C-reactive protein; hs-cTnI: high-sensitivity cardiac troponin I.
DISCUSSION
In this pilot study of COVID-19 patients, the value of CONUT score for predicting hospital stay length and the risk of long COVID based on the review of the electronic medical record and follow-up were assessed. It was revealed that higher CONUT score is an independent predictor of prolonged hospital stay and the development of long COVID in patients with COVID-19. These findings underscore the importance of a rapid evaluation tool to determine the nutritional status of patients with COVID-19 and identify the need for more aggressive management through hospitalization or intensive care in those with malnutrition.
Clinical studies have found that the incidence of malnutrition is high in patients with COVID-19, especially in elderly patients (19). The CONUT score was an objective screening tool for identifying undernutrition in a hospital population (17). In the present study, we found 67 % of patients with COVID-19 were at CONUT score ≥ 2 and 17 % were at CONUT score ≥ 5. This result may be partly attributed to the fact that components that made up CONUT score were consumed by the acute inflammatory response to SARS-CoV-2 infection. Besides, SARS-CoV-2 can attack the mucosal epithelium and cause gastrointestinal symptoms, which will further impair the nutritional status of the patients (20). This result was consistent with previous studies and revealed that patients with COVID-19 were at risk of undernutrition.
Although the nutritional status of the host has not been considered as a conventional risk factor to the disease progression of viral infectious diseases, the immune response has often been shown to be weakened by inadequate nutrition in many viral pandemics (20,21). The LOS is an important parameter to reflect the clinical outcome of COVID-19. Most importantly, shortening the time of hospitalization plays a critical role on timely supply of medical resources for COVID-19 patients considering the enormous burden placed by COVID-19 pandemic. In the present study, a significant positive correlation was found between CONUT scores and LOS. This correlation was still significant after adjusting for potential confounders in multivariate linear regression model. This result may be attributed to the reason that CONUT score provides information about both energy stores and the severity of inflammation in the body, which is associated with LOS (22). This finding is in accordance with a previous study by Bengelloun et al. and strengthens the potential role of CONUT score for identifying those at high-risk of prolonged hospital stay in patients with COVID-19 (13).
Reports of long COVID are rising but little is known about prevalence, risk factors or whether it is possible to predict a protracted course early in the disease. Here we examined symptoms 27 months after an acute SARS-CoV-2 infection, and demonstrated that 35.1 % of hospitalized patients were still troubled with at least one long COVID symptom after three months after discharge. This result is in accordance with a previous study by Huang et al. in a Wuhan cohort (23). Another key finding of the present study was that CONUT score predicts the risk of developing long COVID in the future. Kaplan-Meier survival curves, based on the CONUT grade, showed early and persistent separation during two-year follow-up. Cox proportional hazards analysis confirmed the results observed in Kaplan-Meier survival curves after adjustment for potential confounding factors. The association of patient symptoms along with blood markers of protein disarrangement and inflammation suggests ongoing alterations in the metabolism and inflammatory state which maintains a vicious circle implicated in the persistence of long COVID. This result highlighted the clinical importance of CONUT score for predicting the risk of long COVID in patients with COVID-19.
The limitations of this study should be considered when interpreting our results. First, the retrospective design with a relatively small sample size does not allow the establishment of clear causality and the results are prone to selection bias. These findings will require further replication, validation, and qualification in large, longitudinal population cohorts. Second, these raw data may just reflect local conditions and are unadjusted for other risk factors such as lifestyle habits and physical activity, which might significantly affect the nutritional conditions of patients.
In conclusion, higher CONUT score predicts longer LOS and the risk of long COVID in patients with COVID-19. If these findings can be substantiated in larger studies, the CONUT score might be useful for risk stratification in COVID-19 patients and help to develop new nutritional treatment strategies for long COVID.















