Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Anales de Psicología
versão On-line ISSN 1695-2294versão impressa ISSN 0212-9728
Anal. Psicol. vol.29 no.3 Murcia Out. 2013
https://dx.doi.org/10.6018/analesps.29.3.145181
Emotional state of family members of adults with retinal degeneration
Estado emocional de familiares de adultos con degeneración retiniana
Helena Chacón-López, María D. López-Justicia, Carolina Fernández-Jiménez, Antonio Chacón-Medina and María T. Polo-Sánchez
Departamento de Psicología Evolutiva y de la Educación. Universidad de Granada
This study was supported by the program "Desarrollo personal y social de los afectados de retinosis pigmentosa" (Andalusian Health Council project 180/03/84).
ABSTRACT
Various studies have documented the emotional changes that accompany the loss of vision in people with retinal degeneration (such as Retinitis Pigmentosa), but the emotional state of family members who live with them has not been extensively studied. However it is known that chronic diseases have repercussions not only on the well-being and quality of life of those affected, but also on their families, possibly making them more susceptible to depression and/or anxiety. Results from 37 family members tested against a control group (38 people) partially supported our hypothesis and revealed that the family members showed higher levels of anxiety, especially the women, whereas partners showed higher scores in depression. The findings indicated that the family members should be receiving some kind of support to help them to resolve problems associated with the progression of the visual pathology.
Key words: Family, depression; anxiety; retinal regeneration; gender; adults.
RESUMEN
Distintos estudios han documentado los cambios emocionales que acompañan a la pérdida de visión en personas con degeneración retiniana (como la retinosis pigmentaria), pero el estado emocional de miembros de la familia que conviven con ellas, no ha sido muy estudiado. Sin embargo, es conocido que la presencia de enfermedades crónicas no sólo repercute en el bienestar y calidad de vida de los afectados, sino también en el de sus familiares, haciéndoles posiblemente más vulnerables a la depresión y o la ansiedad. Los resultados obtenidos de 37 miembros de familias de personas afectadas, frente a un grupo control (38 personas), apoya parcialmente nuestra hipótesis y revela que los primeros mostraban niveles más altos de ansiedad, principalmente las mujeres; mientras las parejas de afectados presentaban puntuaciones más altas en depresión. Los hallazgos indicaban que los miembros de familias de personas afectadas deberían recibir algún tipo de apoyo para ayudarles a resolver problemas asociados al avance de la patología visual.
Palabras clave: Familia; depresión; ansiedad, degeneración retiniana; género; adultos.
Introduction
Various studies have documented the emotional and functional changes that accompany loss of vision in people with degenerative retinal diseases, like Retinitis Pigmentosa (Hahm et al., 2008; Strougo, Badoux, & Duchanel, 1997). But, the emotional state of family members that live with them has not been widely studied, and the impact of low vision in general on the psychosocial adjustment of the family has not been analyzed (Bambara et al., 2009a). However, it is known that chronic diseases have repercussions not only on the well-being and quality of life of those affected, but also on their families (Agudelo, Casadiegos, & Sánchez, 2009; Knussen, Tolson, Swan, Stott, & Brogan, 2005; Olsen & Yorgason, 2009), possibly making them more susceptible to depression and/or anxiety. When a family is faced with a long-term disease or the disability of one of its members, an emotional impact is produced that affects the whole family. According to Rolland's systemic model (2000) the members of a system are interrelated in such a way that any change produced in one of the members will affect the others, which in turn will affect the first in a circular chain of influence. In this way, interaction becomes the central element creating a system, in which the fundamental aspect is, in the case of a disease, the interactions between the disease and the individual, family and other biopsychosocial systems.
In the provision of help in situations of illness and disability, there is no doubt that the family constitutes one of the main agents of informal support, meaning the care and attention given altruistically to people with some degree of disability. In this sense, family members of adults with low vision often provide practical support (Barron, Foxall, von Dollen, Jones, & Shull, 1994; Cimarolli & Boerner, 2005; Reinhardt, 1996) and emotional support (Goodman & Shippy, 2002), frequently acting as an informal extension of medical care, without possessing sufficient training for this task, like those who help family members with difficulties of other types (Dreer, Berry, Elliot, & Rivera, 2007). The role of the family members depends on such diverse factors as the severity of the visual impairment, the impact of vision loss on everyday living, the existence of other comorbid health problems and type and level of help given (Bambara et al., 2009a). These factors can cause emotional tension, stress and mood changes (Ledermann, Bodenmann, Rudaz, & Bradbury, 2010; Olsen & Yorgason, 2009; Ostwald, 2009) since a conflict arises between the needs of the caregiver and those of the family member with visual impairment (Bambara et al., 2009a). For these reasons, a greater knowledge of the emotional state of the family members is required in order to detect possible difficulties, give them the help they need and foster the optimum well-being and adaptation of people with visual impairment as well as those they live with.
Although it has been established that the support provided by the family has an influence even on the positive results of the visual rehabilitation of its family members (Cimarolly & Boerner, 2005; Reinhardt, Boerner, & Horowitz, 2006), nevertheless it has been found that visual impairment is an important stress factor in the conjugal relationship, being related to a greater risk of separation and divorce (Bernbaum, Albert, & Duckro, 1993). In the case of spouses who are the caregivers of their partners with non-visual disabilities, their involvement is associated with their own physical, psychological and emotional well-being (Ledermann et al., 2010). They experience more depressive symptoms and greater anxiety than their partners (Franks, Lucas, Parris-Stephens, Rook, & Gonzalez, 2010; Strawbridge, Wallhagen, & Shema, 2007) and the stress they feel affects the quality of marital communication and the general quality of the marital relationship (Bowen, MacLehose, & Beaumont, 2011; Ledermann et al., 2010). In relation to gender differences, Strawbridge et al. (2007) concluded that the impact of husbands' vision impairment on wives was greater than the impacts-of wives' vision impairment on husbands.
Other studies have shown that a large population of people who act as caregivers of visually impaired adults experience significant physical, psychological and emotional distress and higher levels of burden, with women under greater risk of experiencing these symptoms (Bambara et al., 2009b; Olsen & Yorgason, 2009; Ostwald, 2009; Yee & Schulz, 2000). It has also been pointed out that there could be an emotional contagion, referring to a process by which the state of mind of people with visual difficulties can affect or extend to others, in this case family members that are in close contact with them (Bambara et al., 2009b; Bookwala & Schultz, 1996; Goodman & Shippy, 2002).
Retinitis Pigmentosa (RP) belongs to a group of degenerative retinal diseases characterized by a progressive loss of vision which frequently leads to blindness. With this disease a genetic alteration leads to photoreceptor degeneration (Fernández, 2007) and clinical features include involvement of both eyes, loss of peripheral or central vision, weakened vision at night or under poor lighting conditions, problems adapting to changes in lighting, and changes in color discrimination (Rundquist, 2004). It is estimated that the disease affects approximately 1 in every 3700-4000 people and is more common in men (65%) than in women (55%) (Fernández, 2007). Frequently many affected people have typical responses to the diagnosis such as symptoms of depression and anxiety (Hahm et al., 2008; Strougo, Badoux, & Duchanel, 1997), however, these reactions vary depending on their perception of the disease, their personal and social resources and the control they have over events that affect them (Wahl, Becker, Burmedi, & Schilling, 2004).
The loss of vision in people with RP is unpredictable and its progression entails a loss of the ability to carry out certain tasks, diminishing self-confidence and self-control of those affected and possibly leading them to perceive themselves in a negative manner (Kiser & Dagnelie, 2008). However, in this process there are social agents such as family members, whose support help in the adaptation to the loss of vision and improve the quality of life (Reinhardt, 2001). In this sense, Nemshick, Vernon, and Ludman (1986) point out that a very high percentage of people with RP considered that the support provided by family was significant, while others perceived it as overprotection and complained that their families did not understand their condition, or ignored or denied the problem; for this reason, they suggested that the families also receive help, since the consequences of RP affect them as well. What seems evident is that the family members should be aware of changes produced in people with RP (associated with the degenerative nature of the disease), as well as the abilities they retain. They should also avoid over-protective attitudes and know what to do, when and how so as not to interfere in their decisions (Cimarolli & Boerner, 2005; López-Justicia & Nieto, 2006; López-Justicia, Fernández- Castillo, Fernández, & Polo, 2011). This requires, on the one hand, encouraging communication between people with RP and their families, due to the importance of interpersonal relationships (Ledermann et al., 2010); and on the other hand, training the family members, strengthening their resources so that they can assume their role, improving their efficiency, reducing their vulnerability and facilitating their adaptation to the progression of the visual impairment of their family members. In order to achieve this objective the identification of family members at risk of suffering emotional problems, such as anxiety and/or depression, related to visual disease becomes a priority. This justifies the evaluation and subsequent psychological intervention, if required, with the aim of helping them to face the consequences of a chronic degenerative retinal disease such as RP.
According to Beck's cognitive theory of depression (1987), the main alteration produced in people with depression is considered to be related to information processing. The risk factor that makes one susceptible to depression is the possession of a series of maladaptive schemes, with a negative content of loss and failure. These are normally acquired in infancy, although they may remain latent and become activated when the person experiences stressful situations or specific environmental incidents. The content of these schemes is composed of the "cognitive triad", which includes a negative vision of oneself, of the world and of the future, and which, acting on information processing, leads to a distorted vision of reality, which in turn causes the depressed person to be convinced that things are as negative as he/she perceives them to be.
On the other hand, anxiety is the apprehensive anticipation of future harm or misfortune, accompanied by a feeling of dysphoria or somatic symptoms of tension. The object of the anticipated harm could be internal or external (López-Ibor & Valdés, 2002). When alluding to anxiety, one must differentiate between anxiety as a state and anxiety as a trait (Spielberger, Gorsuch, & Lushene, 2002). The former refers to a temporary emotional state or condition, characterized by subjective feelings of tension, apprehension and hyperactivity of the autonomic nervous system; while anxiety as a trait denotes a stable propensity to anxiety, or a tendency to perceive situations as threatening, which increases the state of anxiety. High scores in anxiety predict emotional problems that accompany certain pathologies and are normally associated, among other features, with depression (Sánchez, Aparicio, & Dresch, 2006).
Negative psychological states such as anxiety and depression appear to be associated with RP, as the studies by Hahm et al. (2008), Nemshick et al. (1986) and Strougo et al. (1997), have highlighted. Other authors have pointed out the possible existence of an emotional contagion between people with visual difficulties that may affect or extend to family members that are in close contact with them (Bambara et al., 2009b). But we have been unable to find any studies that confirm the presence of depression and/or anxiety (as a temporary emotional state or as a stable propensity to anxiety) in the family members who live with adults who have RP and who have residual vision, compared with a group of adults without visual difficulties, who had no contact with anyone who has this disease. It has been highlighted, however, that visual impairment is an important factor in the conjugal relationship and a relationship was found between depression of a visually impaired person and depression of his/her spouse (Strawbridge et al., 2007). Hence the first hypothesis of this study is that family members who live with people with a degenerative retinal disease, such as RP will also present these emotional alterations, and that the partners of these people will show a more negative emotional state than the other family members.
It has also been highlighted that women who live with people with visual difficulties are at greater risk of enduring greater pressure and experiencing negative emotional states (Bambara et al., 2009b; Strawbridge et al., 2007). For this reason we also aimed to determine if there were differences associated with gender in the emotional state of family members. Therefore, the second hypothesis of the study is that women who live with family members with visual impairment will show higher levels of anxiety (as a temporary emotional state or as a stable propensity to anxiety) and/or depression.
Method
Participants
A total of 75 people participated divided into two groups: a first group formed by 37 family members of people with RP (average age 43.89, DT = 12.458) (partner, son/daughter, father/mother, brother/sister and brother or sister in law); and a second control group composed of 38 people (average age 41.03, DT = 10.146) (partner, boyfriend/girlfriend and brother/sister) who had no contact or relationship with anyone with this disease. Table 1 shows the demographic characteristics of the participants (gender, age, level of studies, relationship, employed/unemployed and mean years since diagnosis), although it should be noted that the number of participants in the different types of familiars is not equal in both groups.
All of the people with RP (family of the participants) had residual vision, although they showed a restriction of the Visual Field (VF). They satisfied the inclusion criteria of being diagnosed at least 3 years before the study (to avoid the greatest crisis or stress period that occurs during or immediately following diagnosis), having residual vision and not having any other disease or disability.
Procedure
The present study was part of a broader study in which the participants were people with RP and whose aim was, among others, to determine their emotional state and that of the family members they lived with.
For the selection of the sample of family members, a meeting was organized with people with RP to explain the objectives of the study and activities to be carried out. Having communicated their willingness to participate voluntarily in the research, the sample was selected from those with RP (members of two Associations) who retained residual vision and showed no other problems. Subsequently, they were asked to provide the name of one or two family members (husband, wife, son, daughter, father, mother, brother, sister) without visual disabilities who lived with them and who would voluntarily participate in the study. A sample of thirty-seven people that satisfied the inclusion criteria was selected. Subsequently, each family member (without RP, ruled out by clinical evaluation) was assessed by one researcher (author of the present paper), a specialist in Psychology.
For the purpose of selecting a control group, 80 senior psychology students who were participating in a practicum program in RP were contacted. Each one received instructions to voluntarily evaluate two adult, distributed homogeneously by age, social characteristics and gender, who did not show visual deficiencies and had not been in contact with people with this problem. The students were trained and supervised in the administering of the tests and any results that were not clear were discarded. Thirty-eight people satisfying the inclusion criteria were randomly selected.
All of the participants in the study completed a personal information form, the STAI anxiety test and, subsequently, the Beck Depression Inventory. Once these were all corrected and analyzed, the participants were informed of the results. None of them objected to the publication of the results. This research study was approved by the Institutional Review Board of the University of Granada in 2009.
Instruments
To obtain information on the demographic characteristics a personal information form was designed. In the case of family members of people with RP, additional items were added referring to relationship and years since diagnosis of their family members with RP.
The participants' level of anxiety was assessed using the State-Trait Anxiety Inventory (STAI) (Spielberger et al., 2002), the objective of which is to evaluate temporary states of anxiety in adolescents and adults. It consists of two separate scales that measure the independent concepts of state (A-S) and trait (A-T). Each consists of 20 items with 4 alternative answers ranging from 0 to 3. The range in each one of the scales is the same, from 0 to 60.
The version of STAI used in the present study has a rate of internal consistency situated between .84 and .87 for A-T and between .90 and .93 for A-S (Spielberger et al., 2002). The values of reliability, calculated by the split-half procedure, are .86 on A-T and .94 on A-S (Spielberger et al., 2002).
To evaluate depression the Beck Depression Inventory was used (Beck, Rush, Shaw, & Emery, 1979). This is a self-applicable instrument, validated for the Spanish population (Vázquez & Sanz, 1997) to quantify symptoms of depression in normal and clinical populations. The BDI has an average reliability (alpha coefficient) of .86 and .74 (Beck, Steer, & Garbin, 1988). The version used in this study was the abbreviated one of 13 items, there being a high correlation (.96) between both forms (Beck et al., 1979). In this version one must choose a sentence from four alternatives, listed in order of seriousness. Each item is assessed with different options of answers from 0 to 3, giving a total possible score of 39 points. The following scores were taken into account: 0-4 Absence of Depression, 5-7 Mild Depression, 8-15 Moderate Depression and >15 Serious Depression (Joffre, Martínez, García, & Sánchez, 2007).
Results
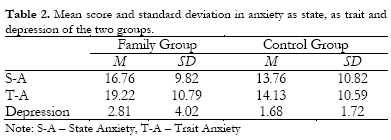
The average scores corresponding to the dependent variables (anxiety as state and as trait, and depression) observed in the two groups (family members and control group) are included in Table 2.
The scores for anxiety (as state and as trait) of the two groups were compared by applying MANOVA, ensuring the fulfillment of the assumptions of this technique (M of Box = 7.83, p > .05). Since this assumption was not fulfilled for the depression variable, it was decided that a non-parametric test be used in this case (U Mann-Whitney).
The results of MANOVA indicated that there were significant differences between the groups (F2, 72 = 94.4; p < .05), showing that they differed in the measure of anxiety as a trait [F1,73= 4.23;p < .05]. The family group scored higher on the scale, with significant differences compared with the control group on the measurement of anxiety as a trait (p < .05). No differences were found in the measures of anxiety as a state [F1,73 = 1.57; p > .05], or in the measures of depression on the non-parametric test applied [U= 617; p = .351].
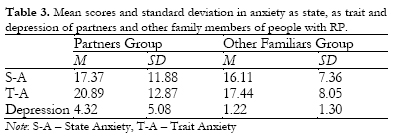
The differences within the group of family members of people with RP (partners and other family members) were studied using a non-parametric U Mann-Whitney test. Significant differences were found associated with partners on the depression variable (U = 94.000; p = .019), on which the partners obtained higher scores, while no differences were found in the measures of anxiety as a state or as a trait (Table 3 shows mean scores and SD of partners and other family members)
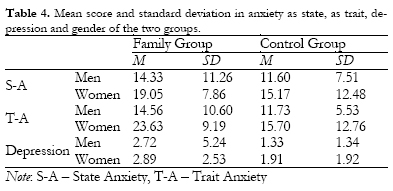
With the aim of testing our second hypothesis, another MANOVA was applied to determine differences associated with gender between the groups (family members and control group). The results indicated that there were significant differences between the groups and gender (F3,71 = 59.4; p < .05), showing that they differed in the measurements of anxiety as trait [F1,73 = 5.97; p < .05]. The average scores corresponding to the dependent variables (anxiety as state and as trait, and depression) and gender observed in the two groups are included in Table 4.
The differences within the groups were also studied using a non-parametric U Mann-Whitney test (due to the small size of the sample) finding significant differences associated with gender in the group of family members on the variable anxiety as trait (U = 83.50; p = .007), on which the women obtained higher scores, while in the control group these differences were not found (U = 156.500; p = .637) (Table 4 shows mean scores and SD)
Discussion
In the present study, we evaluated primarily depression and anxiety (as a state and a trait) in a group of family members of people with RP against another of individuals without association to people with visual impairment. The results showed that anxiety as a trait is greater in family members of people with RP. Their anxiety levels indicate that they are prone to suffering from anxiety, meaning that their tendency to perceive situations as threatening increases their state of anxiety. This could be due to a feeling of threat or anticipation of damage, which is understandable given the degenerative nature of RP. These results follow the same lines of former studies, or Rolland's model (2000), suggesting that a chronic, progressive disease like RP could have a negative effect not only on family atmosphere and the well-being of those who suffer from the disease, but also on those who live with them (Agudelo et al., 2009; Knussen et al., 2005; Olsen & Yorgason, 2009).
With respect to anxiety as a state, we should point out that although a significant difference was not found; nevertheless if we consider the mean scores, we observe that the scores for the group of family members are notably higher than those of the control group. A larger sample size would probably confirm this, although it could also be that the time passed since the diagnosis was made (at least 3 years before the evaluation) has affected the results.
With regard to depression in the family members of people with RP, when the type of relationship (partner or other family member) was investigated, we found significant differences in the partners group indicating that they obtained higher scores than other family members. Although it should be noted that the level of depression was in the limit range of mild depression. Prior work has focused exclusively on the emotional state experienced by people with RP in which they have found depressive symptoms (Hahm et al., 2008; Strougo et al., 1997). However, there are no studies centred on family members of adults with RP, which prevents us from comparing our results. Nevertheless, our data coincide with those found in previous studies carried out on people with visual impairment or other difficulties (Franks et al., 2010; Strawbridge et al., 2007) and may confirm that there is an emotional contagion between couples on this variable (Bambara et al., 2009b; Bookwala & Schultz, 1997; Goodman & Shippy, 2002).
The data obtained partially confirm our first hypothesis, which predicted that family members would show emotional alterations such as anxiety and/or depression. We stress that they partially confirm our hypothesis since we found differences in the anxiety as trait variable when we studied the two groups (family group and control group), whereas only the depression variable was confirmed when we studied a group of partners of people with RP against other family members.
We also found differences associated with gender when we studied the two groups (family group and control group), on verifying that women who live with people with RP show greater levels of anxiety as a trait, data which also partially confirms our second hypothesis and that coincides with those found in previous studies (Bambara et al., 2009b; Olsen & Yorgason, 2009; Ostwald, 2009; Yee & Schulz, 2000). In general, women are known to tend to express their emotions more frequently than men, particularly feelings of depression, sadness, anxiety or fear and important changes in their mood (Olsen & Yorgason, 2009; Ostwald, 2009; Smith, Nolen-Hoeksema, Fredrickson, & Loftus, 2003). The results of our study seem to follow this tendency, but they do not allow us to completely support these conclusions, due to differences in the sample. In our study, not only wives of people with RP participated, but also other family members (16). Nonetheless, the number of couples was greater (21) and among these there were more wives (12) than husbands (9).
The findings suggest that the effects of the RP on the familiars may not be as negative as in other degenerative diseases, or that these are milder and difficult to detect. Even so, we think the implications of this study are of interest to professionals in the field of health who work with people with degenerative retinal diseases, people with RP and their families.
The outcomes of this study lead us to conclude that it would be beneficial for family members to receive some kind of support, to help them to cope with the consequences of this pathology. It would be especially important to work on the impact of the loss that RP involves with family members and especially with the partners and the women, giving them guidance so that they understand what their actions should be, know what abilities the person still has and endeavour to ensure that he/she continues to use them, at the same time avoiding overprotective behaviour. It would also be advisable to provide realistic information and demonstrations of the characteristics and progression of the disease, participation in group discussions, or analysis of their actions with affected family members. The aim is that they know what to do, how and when to intervene, without interfering in their autonomy and independence (Cimarolli & Boerner, 2005; Lopez-Justicia & Nieto, 2006; Lopez-Justicia et al., 2011). In this sense, it would be advisable that associations and professionals dedicated to this topic, work together to propose activities and make them accessible to the family members of people with this pathology. It is also recommended that family members read or compile information about the problem, speak with other family members in the same situation and discuss it with professionals, because of the significant relationship between social support, principally from the partner, and health (Martos & Muñoz, 2011). These proposals will benefit both people with RP and their families, given the fundamental role that the latter play in the rehabilitation process (Cimarolly & Boerner, 2005; Reinhardt, Boerner, & Horowitz, 2006) and adaptation to the new situation, since it has been highlighted that the help they give is associated with a better adaptation to the problem.
Our study has several limitations. In the first place, depression was diagnosed through a self-reporting questionnaire rather than using conventional criteria. It should be noted that, despite not being designed for the diagnosis of depression, this questionnaire has proven to be a good screening method (Vázquez & Sanz, 1997). Another disadvantage lies in the fact that we have used the abbreviated version, and it is known that as the number of items is reduced, so is reliability. Nevertheless, we should point out that a high correlation (.96) was confirmed between both versions (Beck et al., 1979). Secondly, the participants were evaluated only once, which prevents us from determining whether anxiety as a trait persists, which would lead us to suspect that it could be a personality trait.
We would like to point out that the size of the sample is small, and the number of participants in the different types of family members is not equal in both groups, which implies a limitation in the generalization of results. Although in contrast, only family members of people with one degenerative retinal disease participated. Furthermore, the sample was intentional in nature, due to the fact that the only participants were volunteer family members of people with RP belonging to two associations of people with RP. But we should point out the difficulties that finding a large enough simple of these pathologies entails, due to the reservations of family members to participate. However, we have attempted to balance the groups with respect to the socio-demographic characteristics of age, relationship, occupation and gender to ensure greater comparability.
Author's note.
We thank Karen J. McMullin for translating parts of the original manuscript into English.
References
1. Agudelo, D. M., Casadiegos, C. P., & Sánchez, D. L. (2009). Relación entre esquemas maladaptativos tempranos y características de ansiedad y depresión en estudiantes universitarios. (Relationship between early maladaptive schemes and anxiety and depression features in University students). Universitas Psychologica, 8(1), 87-104. [ Links ]
2. Bambara, J. K., Wadley, V., Owsley, C., Martin, R. C., Porter, C., & Dreer, L.E. (2009a). Family functioning and low vision: A systematic review. Journal of Visual Impairment and Blindness, 103(3), 137-149. [ Links ]
3. Bambara, J. K., Owsley, C., Wadley, V., Martin, R., Porter, C., & Dreer, L. E. (2009b). Family caregiver social problem solving abilities among persons with low vision. Investigative Ophthalmology & Vision Sciences, 50(4), 1585-1592. [ Links ]
4. Barron, C., Foxall, M., von Dollen, K., Jones, P., & Shull, K. (1994). Marital status, social support, and loneliness in visually impaired elderly people. Journal of Advanced Nursing, 19, 272-280. [ Links ]
5. Beck, A. T. (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy: An International Quarterly, 1, 5-37. [ Links ]
6. Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. New York: Guilford Press. [ Links ]
7. Beck, A. T., Steer, R. A., & Garbin, M. C. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8, 77-100. [ Links ]
8. Bernbaum, M., Albert, S. G., & Duckro, P.N. (1993). Personal and family stress in individuals with diabetes and vision loss. Journal of Clinical Psychology, 49, 670-677. [ Links ]
9. Bookwala, J., & Schulz, R. (1996). Spousal similarity in spousal well-being: The cardiovascular health study. Psychology and Aging, 11, 582-590. [ Links ]
10. Bowen, C., MacLehose, A., & Beaumont, J. G. (2011). Advanced multiple sclerosis and the psychosocial impact on families. Psychology & Health, 26, 113-127. [ Links ]
11. Cimarolli, V., & Boerner, K. (2005). Social support and well-being in adults who are visually impaired. Journal of Visual Impairment and Blindness, 99(9), 521-534. [ Links ]
12. Dreer, L. E., Berry, J., Elliot, T., & Rivera, P. (2007). Characteristics of family caregivers of persons with spinal cord injury at risk of depression. Rehabilitation Psychology. 52, 351-357. [ Links ]
13. Fernández, E. (2007). Retinosis pigmentaria: Preguntas y respuestas. (Retinitis Pigmentosa: Questions and answers). Elche: Cátedra Bidons Egara. [ Links ]
14. Franks, M. M., Lucas, T., Parris-Stephens, M. A., Rook, K. S., & Gonzalez, R. (2010). Diabetes distress and depressive symptoms: A dyadic investigation of older patients and their spouses. Family Relations, 59(5), 599-610. [ Links ]
15. Goodman, C. R., & Shippy, R. A. (2002). Is it contagious? Affect similarity among spouses. Aging & Mental Health, 6, 266-274. [ Links ]
16. Hahm, B., Shin, Y., Shim, E., Jeon, H., Seo, J., Cheng, H., & Yu, H. (2008). Depression and the vision-related quality of life in patients with Retinitis Pigmentosa. British Journal Ophthalmology, 92, 650-654. [ Links ]
17. Joffre, V. M., Martínez, G., García, G., & Sánchez, L. (2007). Depresión en estudiantes de medicina. Resultados de la aplicación del inventario de depresión de Beck en su versión de 13 ítems. (Depression in medical students. Results of the application of the Beck Depression Inventory in its version of 13 items). Revista Argentina de Clínica Neuropsiquiátrica, 14(1), 86-93. [ Links ]
18. Kiser, A., & Dagnelie, G. (2008). Reported effects of non-traditional treatments and complementary and alternative medicine by Retinitis Pigmentosa patients. Clinical and Experimental Optometry, 91(2), 166-176. [ Links ]
19. Knussen, C., Tolson, D., Swan, I. R. C., Stott, D. J., & Brogan, C. A. (2005). Stress proliferation in caregivers: The relationships between caregiving stressors and deterioration in family relationships. Psychology & Health, 20(2), 207-221. [ Links ]
20. Ledermann, T., Bodenmann, G., Rudaz, M., & Bradbury, T. N. (2010). Stress, communication, and marital quality in couples. Family Relations, 59(2), 195-206. [ Links ]
21. López-Ibor, J. J., & Valdés, M. (2002). DSM-IV-TR. Manual diagnóstico y estadístico de los trastornos mentales. (DSM-IV Diagnostic and Statistical Manual of Mental Disorders). Barcelona: Masson. [ Links ]
22. López-Justicia, M. D., & Nieto, I. (2006). Self-concept of Spanish young adults with RP. Journal of Visual Impairment and Blindness, 100(6), 366-370. [ Links ]
23. López-Justicia, M. D., Fernández- Castillo, A., Fernández, C., & Polo, T. (2011). Age, educational level and gender in self-concept of people with Retinitis Pigmentosa. Anales de Psicología, 27(2), 292-297. [ Links ]
24. Martos, M. J., & Muñoz, C. (2011). Apoyo funcional vs. disfuncional en una muestra de pacientes crónicos. Su incidencia sobre la salud y el cumplimiento terapéutico. Anales de Psicología, 27(1), 47-57. [ Links ]
25. Nemshick, L.A., Vernon, McC., & Ludman, F. (1986). The impact of retinitis pigmentosa on young adults: Psychological, educational, vocational and social considerations. Journal of Visual Impairment and Blindness, 89, 859-862. [ Links ]
26. Olsen, S., & Yorgason, J. B. (2009). Older adults with diabetes and osteoarthritis and their spouses: Effects of activity limitations, marital happiness, and social contacts on partners' daily mood. Family Relations, 58(4), 460-474. [ Links ]
27. Ostwald, S. K. (2009). Who is caring for the caregiver? Promoting spousal caregiver's health. Family and Community Health, 32(1), 5-14. [ Links ]
28. Reinhardt, J. P. (1996). The importance of friendship and family support in adaptation to chronic vision impairment. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51, 268-278. [ Links ]
29. Reinhardt, J. P. (2001). Effects of positive and negative support received and provided on adaptation to chronic visual impairment. Applied Developmental Science, 5, 76-85. [ Links ]
30. Reinhardt, J. P., Boerner, K., & Horowitz, A. (2006). Good to have but bad to use: Differential impact of perceived and received support on well-being. Journal of Social and Personal Relationships, 23(1), 117-129. [ Links ]
31. Rolland, J. (2000). Familias, enfermedad y discapacidad. Una propuesta desde la terapia sistémica. (Family, illness and disability. A proposal from the perspective of systemic therapy). Barcelona: Gedisa. [ Links ]
32. Rundquist, J. (2004). Low vision rehabilitation of Retinitis Pigmentosa. Journal of Visual Impairment and Blindness, 98, 718-724. [ Links ]
33. Sánchez, M. P., Aparicio M. E., & Dresch, V. (2006). Ansiedad, autoestima y satisfacción autopercibida como predictores de la salud: diferencias entre hombres y mujeres. (Anxiety, self-esteem and self-perceived satisfaction as predictors of health: Differences between men and women). Psicothema, 18(3), 584-590. [ Links ]
34. Smith, E., Nolen-Hoeksema, S., Fredrickson, B., & Loftus, G. (2003). Introducción a la Psicología. (Introduction to Psychology) Madrid: Thomson. [ Links ]
35. Spielberger, C. D., Gorsuch, R. L., & Lushene, R. E. (2002). Manual STAI. Cuestionario Ansiedad Estado-Rasgo. (State-Trait Anxiety Inventory Handbook. State-Trait Anxiety Questionnaire). Madrid: TEA Ediciones. [ Links ]
36. Strawbridge, W. J., Wallhagen, M. I., & Shema, S. J. (2007). Impact of spouse vision impairment on partner health and well-being: A longitudinal analysis of couples. Journal of Gerontology: Social Sciences, 62B(5), 315-322. [ Links ]
37. Strougo, Z., Badoux, A., & Duchanel, D. (1997). Problèmes psycho-affectifs associés à la rétinopathie pigmentaire. (Psychological and affective problems associated with Retinitis Pigmentosa). Journal Français D'Ophtalmologie, 20, 111-116. [ Links ]
38. Vázquez, C., & Sanz, J. (1997). Fiabilidad y valores normativos de la versión española del Inventario de Depresión de Beck. (Reliability and normative values of the Spanish version of the Beck Depression Inventory). Clínical Salud, 8, 403-422. [ Links ]
39. Wahl, H. W., Becker, S., Burmedi, D., & Schilling, O. (2004). The role of primary and secondary control in adaptation to age-related vision loss: A study of older adults with macular degeneration. Psychology and Aging, 19(1), 235-239. [ Links ]
40. Yee, J., & Schulz, R. (2000). Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist, 40, 147-164. [ Links ]
![]() Correspondence:
Correspondence:
Helena Chacón-López
Facultad de Ciencias de la Educación
Departamento de Psicología Evolutiva y de la Educación
Universidad de Granada
Campus Universitario de La Cartuja, s/n
18071, Granada (Spain)
E-mail: helenachacon@ugr.es
Article received: 24-1-2012
Reviewed: 8-10-2012
Accepted: 22-10-2012