Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Anales de Psicología
versión On-line ISSN 1695-2294versión impresa ISSN 0212-9728
Anal. Psicol. vol.33 no.2 Murcia may. 2017
https://dx.doi.org/10.6018/analesps.33.2.236781
Family and Personal Predictors of Eating Disorders in Young People
Factores familiares y personales predictores de trastornos de conducta alimentaria en jóvenes
Angélica María Moreno Ruge and Constanza Londoño-Pérez
Universidad Católica de Colombia
ABSTRACT
This correlational descriptive study aimed to validate the predictive model of risk of developing eating behavior disorder in young people based on the measurement of variables such as eating behavior, body image dissatisfaction, body mass index, family functioning, and the use of criticism toward young people about their weight and the shape of their body, in young people and parents. The non-randomized sample of convenience included 208 participants, 104 of them were adolescents aged between 11 and 18 years, studying in different high schools, and 104 family members considered to be significant by the teenagers. EAT-26, ECA, Family APGAR, FEICS, and BMI were applied, all validated for the Colombian population. As a result of the multivariate analysis, it was found that the high risk of developing behavioral disorders in young people is related to high risk in their relatives; the article concludes that parents, in addition to playing a protective role, may represent a risk factor for the eating behavior of their children, given that children model their behavior on their parents from early childhood.
Key words: Eating behavior; body image; family; family relationships; young people.
RESUMEN
El presente estudio descriptivo correlacional tuvo como objetivo validar el modelo predictivo del riesgo de padecer trastorno de la conducta alimentaria en jóvenes a partir de la medición de variables conducta alimentaria, insatisfacción corporal, índice de masa corporal, funcionamiento familiar y el uso de críticas hacia el joven sobre el peso y forma de su cuerpo, en jóvenes y padres. La muestra no aleatorizada de conveniencia fue de 208 participantes, de los cuales 104 eran adolescentes entre 11 y 18 años, vinculados académicamente en una institución educativa de secundaria y 104 familiares que cada joven consideraba significativo. Se aplicó EAT-26, ECA, APGAR Familiar, FEICS y el IMC, instrumentos validados para población Colombiana. Producto de los análisis multivariantes realizados, se encontró que el alto riesgo de padecer trastornos de la conducta en los jóvenes se relaciona con alto riego en sus familiares y se concluye que los padres además de ejercer un rol protector pueden representar un riesgo en la conducta alimentaria de los hijos teniendo en cuenta que los hijos modelan el comportamiento de sus padres desde la primera infancia.
Palabras clave: Conducta alimentaria; imagen corporal; familia; relaciones familiares; jóvenes.
Introduction
Overall incidence rates of eating alimentary disorders (EATs) have been significantly increasing worldwide. This situation is not foreign to Latin America, since the study of adolescent health carried out by the Ministry of Health in Mexico detected 6211 cases of anorexia nervosa, of which 4235 were women, as well as 2787 cases of bulimia nervosa in the Medical Units of the Secretary of Health between January and July (World Health Organization [WHO], 2009; Pan American Health Organization [PAHO], 2012).
Although several studies in Colombia indicate that EBDs are not the most prevalent mental health problems, the same studies evidence their increasing impact on the population between 15 and 35 years of age (Ministerio de Protección Social, 2003; 2007). The Colombian National Study of Mental Health demonstrated that the average age of onset of EAT is 15 years, mainly in women, with a prevalence close to 70% in university students, with a higher proportion in women, but with a clear increase in male cases (Avellaneda, 2009; Cano et al., 2007; Espinosa, Fandiño, Giraldo & Martínez, 2007).
As in the case of a large number of mental health problems, EATs have a complex origin and course, but it has been demonstrated that factors such as race, socioeconomic level, height, sex, age (Espinosa, Fandiño, Giraldo & Martínez, 2007), occupation (Cano et al., 2007) and, presumably, eating behavior itself are associated with a predisposition and initiation of EBDs, which, in turn, are influenced by these disorders (Loubat, 2006). Personal and family factors have been extensively studied separately; however, the mutually potentiating effects of the factors involved have not yet been integrated into a predictive model. On the contrary, studies focus on the effects of one or another factor, without achieving a global perspective.
EBDs have been associated especially with body image dissatisfaction or existence of negative beliefs about one's body shape and the degree of suffering caused (Hernández & Londoño, 2013). This image may be inaccurate, since it is constructed from culture starting in childhood (Castrillón, Luna & Aguirre-Acevedo, 2007). Body image includes emotional, cognitive, and behavioral elements that determine conditions of acceptance, denial, and body transformation, due either to a poor image of one's own body, to the degree of acceptance of one's physical characteristics (Gempeler, 2007) or to the emotional suffering experienced (Bolaños & Jáuregui, 2010; González, Oudhof Van, Rodríguez & Unikel, 2010).
EATs transcend the individual level, although persistent patterns of impulsivity, tendency to hostility and selfdestruction can be found in them; it has been pointed out, however, that the most predictive factors of OCD in subjects with EBD are excessive order and arrangement of foods under rigid and controlled patterns (Bulika & Striegel, 2007; Rivarola & Penna, 2006; Roberts, 2006) and abusive drug use (Godart et al., 2013).
It should be noted that eating behavior includes feeding patterns that define the preparation, disposition and availability of food, determined largely by family and cultural practices (Contreras, 2007), as family, society, the State and religious beliefs establish the parameters of ingestion or the restriction of certain foods; conditions that define the appreciation and attitude towards them in terms of good-bad, healthy-harmful, convenient-not convenient, sacred-profane, ordinary-festive, feminine-masculine, and, even, childish-adult.
Although an individual's genetic diathesis, his or her personality traits and contexts for interaction are potentially precipitating factors for EBDs, family represents a significant factor in the construction of altered or hypervalent personalities that favor body distortion (Kalarchianb, Lilenfelda, Marcusb & Ringhamb, 2008). Authors like Dancygera, Fornaria, Sciontic, Sundaya and Wisotskya (2009) found that women with restrictive-type AN perceived the social world more positively than women with purgative AN, who were more sensitive to the deterioration in family relationships; however, it should not be forgotten that parents of persons with EBD often have a history of psychopathology and said condition can be repeated for generations.
The family is a space of socialization and exchange of thoughts and emotions for the individual; its functioning significantly influences the representation that individuals have of the world (Dancygera, Fornaria, Sciontic, Sundaya & Wisotskya, 2009) and of themselves. Food intake and dietary restrictions are not alien to the learning generated from the family. Bulika et al. (2010) have reported that food restrictions are potentially transferred from parents to children, especially when the mother has an eating disorder, which contributes to the development of eating disorders in children. This corroborates that the mother plays an important role in the construction of models for eating habits, which are transmitted through breeding patterns, and may represent both protective and risk factors regarding alimentation depending on her practices (García, Depetris & Rossini, 2013).
Greater contact with family seems to be a protective factor against developing an EBD, since there is a greater accompaniment in the process of food intake as well as in taking care of the food preparation (Kalarchianb, Lilenfelda, Marcusb & Ringhamb, 2008). However, if the accompaniment is characterized by dysfunction (Erola, Toprakc & Yazicib, 2007), including poor communication and abusive criticism of parents towards children who increase their external attributions, as well as impoverished control, it increases the probability of initiating an EBD (Espeleaga, Hannum, Lowa & Menoa, 2008).
Regarding family roles, the role of the mother and female caregivers is very important in the processes of modeling and reinforcement of eating patterns, since alimentation is usually taken care of by the person who plays the maternal role. And it is precisely women who more frequently express concern for their figure, body image, weight and attractiveness, conditions that do not favor the mental and physical health of their children (Araya & Atalah, 2002; Cash & Pruzinsky, 2002). However, given that individual family factors are studied in an isolated way and due to the lack of analysis of specific mental health issues of caregivers, it is relevant to analyze not only their global role but also the personal characteristics that can count as risk factors for themselves and as enhancing risk factors for EBD in children.
Therefore, although empirical findings help to explain EBDs, it is necessary to deepen our understanding of how thoughts, behaviors, and practices are generated within the family, which, in a certain moment, can put at risk the mental health of family members in such a way that a behavioral disorder might be developed. Although family and its accompaniment are believed to represent protection, this view ultimately ignores that it is the parents who create eating practices and influence the formation of body image and the degree of satisfaction with the same, while they exercise control over eating behaviors and the way children perceive their body image. Thus, the present study aimed to determine whether factors such as BMI of young people and satisfaction with their own body image are predictors of the risk of developing EBD in adolescents between 11 and 18 years of age.
Method
The present research presents a descriptive, correlational, cross-sectional study with multivariate analysis.
Participants
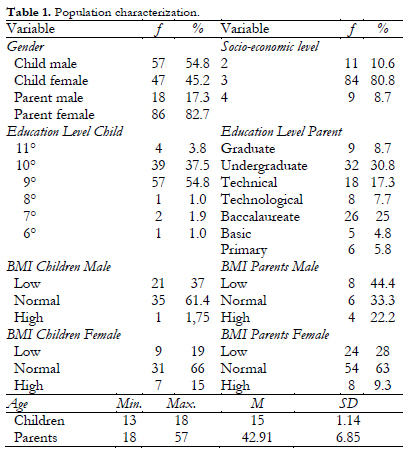
The selected sample of convenience consisted of 104 school-going adolescents of both sexes and 104 significant relatives (father, mother or a third caregiver). The age range of students was from 13 to 18 years, with a mean age of 15 years, and parental age was between 30 and 57 years, with a mean age of 43 years. The schooling level of the young participants ranged between 7 and 11 years of high school, while the education level of parents ranged from primary to postgraduate education. The inclusion criteria for the youth population were the following: adolescents between 11 and 18 years of age, enrolled in schools and living in Bogotá with one of their parents or a member of their family, mainly from socio-economic strata 3. Both adult and under-age participants signed a consent form and an informed assent form once the institutional authorization to carry out studies was obtained, after the approval of the study by the research committee of the institution where researchers were affiliated.
Regarding BMI, it was possible to identify that mothers and children of both sexes had normal weight as well as their fathers. It was found that both male and female children were in the normal range of BMI. This was the same for the mothers; however, a greater percentage of the fathers was below normal values in this indicator. In general, it was evident that the population had a lower tendency to have a high range of BMI.
Instruments
Abbreviated Eating Attitudes Test (EAT-26), which is designed to evaluate dietary behaviors; this instrument is used to identify symptoms and concerns characteristic of EBDs in non-clinical samples. In Colombia, the test was validated for the population between 9 and 17 years of age; reliability measured with Cronbach's alpha was 0.87, 95% CI (Castrillón, Luna & Aguirre-Acevedo, 2007).
Body Mass Index (BMI); this indicator was directly calculated for all participants using the same unit of analysis (a tape measure and scale); additionally, percentages were adjusted to the tables validated for Colombia by the Colombian Institute of Family Welfare (ICBF for its acronym in Spanish) and WHO guidelines.
Food Behavior Questionnaire (FBQ), which is an instrument used to diagnose EBD and to get information about the nutritional status of individuals. This instrument has a specificity of 74 to 80 %, sensitivity is between 90.5 and 94.5 %, with an existing correlation of 0.91, and the cut-off point is 23. It was designed by Ángel, Chavarro, García, Martínez and Vásquez (2000).
Body Shape Questionnaire (BSQ), which is an instrument designed to evaluate dissatisfaction with body image; it was validated for the Colombian population by Avendaño, Castallón, Luna and Pérez (2007). The questionnaire has a reliability of 0.96, with an internal consistency of 0.95; for the first factor, consistency is 0.95 and for the second, 0.92.
Family APGAR, a questionnaire initially developed by Smilkstein in 1978 to explore family functioning and validated for adolescents in Colombia by Avendano, Campo, Duarte and Forero (2006). The instrument has good performance and the internal consistency is satisfactory (0.793).
Family Emotional Involvement and Criticism Scale (FEICS), which was developed and validated by researchers of the Family Medicine Center and Psychiatric Unit at the University of Rochester (1991). The test has a Cronbach's alpha of 0.76 for emotional involvement and 0.82 for perceived criticism. In Colombia, it was validated by Restrepo et al. (2004).
Results
The results were analyzed using structural equations, which allowed to estimate predictive relationships among multiple variables and to include measurement errors in endogenous and exogenous variables.
When analyzing the level of risk of EBD, percentages are distributed in ranges of normal, low, and high risk. Both parents and children are in the normal range, representing a non-clinical population. The performance of each factor was different in parents and in children. Regarding a concern for weight gain (F1), the study found that 49% of the young people had a normal condition, while it was 70.2% in their parents. The percentage of clinical population for this factor is 12% in children and 1 % in parents. As for a concern for the amount of calories in food (F2), no clinical population was found in children, while 8.1% of the parents were in this range, with a high percentage. All of the children are in the normal range, while only 40.4% of the parents are in the same range; 51.6% of the parents are in the low-risk range, while 26.3% are in the high-risk range.
Regarding obsessive preoccupation with food (F3), it was observed that, although parents and children both had a clinical population, the percentages were low, 1.9% and 1%, respectively. Most of the studied population was within normal ranges. The percentages for risk levels were similar in parents and children, but there was a greater proportion in the low-risk range. For the factors of bulimia (F4) and social concern about weight gain (F5), no clinical population was found and the percentages were similar: in F4, 91.3% of the children and 94.2% of the parents were in the normal range, while 8.6% of the children and 5.8% of the parents were in the low-risk and high-risk ranges correspondingly. Both parents and children presented similar percentages of normality in F5. There was no clinical population; there were no high-risk percentages in parents and 5.8% was in the low-risk range, while in children the low-risk percentage was 4.8% and the high risk was 1.9% (Table 2).
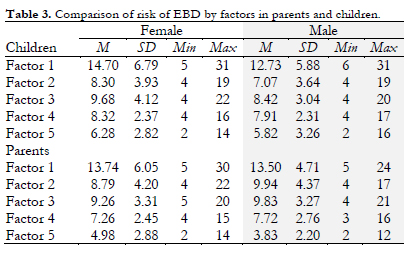
Regarding the comparison of the risk of EBD by gender, the study found that women were more concerned about weight gain (F1); this aspect was prominent in female children. As for the concern for the amount of calories in food (F2), male children had the lowest score, while fathers reported higher scores, followed by the mothers and female children. Regarding the obsessive preoccupation with food (F3), fathers were sensitive to it, followed by daughters and mothers, while male children were less affected by this factor.
With regard to bulimia (F4), the study evidenced that, on average, this factor was predominant in the youth population, with female children having the highest scores. As for the parents, on average, men had higher score in this factor. Similarly, it was found that young people were prone to become upset and feel more social concern about weight gain (F5). On average, female children had more incidence of this; regarding their parents, women had a higher average than men in this category.
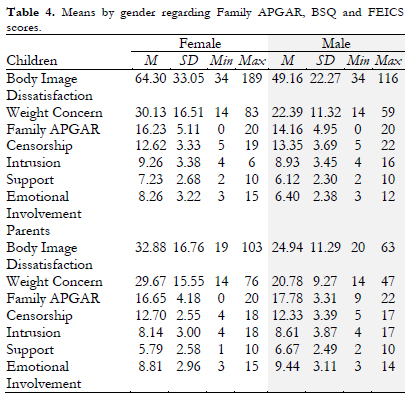
In addition to identifying the risk factors of EBD for the sample, other variables were also considered that could influence the development of behavioral disorders, one of them being the body image, which was evaluated using the BSQ. This test is subdivided into two factors: Body Image Dissatisfaction and Weight Concern. In general, the study population showed greater sensitivity to body image dissatisfaction. In both factors, young people obtained higher scores, with the female gender dominating each factor (Table 4).
In addition, several instruments were used to evaluate the family and their perception of the same. One of these instruments was the Family APGAR, which evidenced that children were less sensitive to perceiving family functioning; in contrast, parents scored higher in this regard, although there were no significant differences between the means of the whole sample analyzed.
Finally, family criticism was considered as another variable that can trigger EBD. This was analyzed using the FEICS scale, which examines four factors, namely, censorship, intrusion, support, and emotional involvement. The results demonstrated that censorship was the predominant aspect in the sample, and it was the male children who presented the highest score in this aspect, followed by female children, mothers, and fathers. Young people perceived more intrusion. This factor was the highest in female children, while parents also scored high on this. It stands out that female children acknowledged more support within the family; in contrast, mothers obtained lower average in this factor. Finally, fathers were more sensitive to emotional involvement, followed by mothers; young people scored low, being the male children who were less prone to this.
Predictive Model
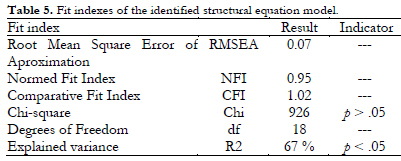
Figure 1 shows the predictive model of the risk of developing an eating behavior disorder, consisting of family and individual factors that reached an explained variance of 67%, considered optimal in this type of analysis. The relationships established in the fitted model indicate, on the one hand, that personal factors such as being female and BMI have an explained variance of satisfaction with body image of 37% and 23%, correspondingly, and that this, in turn, predicts the risk of developing an EBD with a relative explained variance of 59%. From this same group of personal factors, concern about weight gain had an explained variance of 35% and obsessive preoccupation with food presented an explained variance of 29%. On the other hand, family factors that contributed to explained variance were the risk of EBD in parents; more specifically, social concern for weight gain with an explained variance of 51%, concern for the amount of calories in food with an explained variance of 32%, obsessive preoccupation with food had an explained variance of 30%; finally, concern about weight gain presented an explained variance of 25% and bulimia had an explained variance of 22%.
Similarly, parental age contributed a negative explained variance of 41% to the risk of EBD; parental age had an explained variance of 28%. Regarding criticism and censorship of parents, the model indicates that factors such as intrusion, emotional involvement, and support had corresponding explained variances of 51%, 30%, and 30%, with a negative weight in the case of support. Although the educational level of parents does not contribute much to the model, it is included in order to maintain the fit of the prediction model.
Finally, although the relationship between the sex of the parents and the risk of EBD was considered important, this factor was excluded, since the group of parents was almost exclusively composed of women (86%). Regarding the indicators of fit of the predictive model, it was noted that the Chi-square was 926 with a p > .05 (non-significant), with 18 degrees of freedom (df), RMSEA was less than 0.10, NFI was greater than 0.8, and CFI was greater than 0.95; all of them indicators of an optimal level of fit and identification of the model (Table 5).
Discussion and Conclusions
The predictive model of the risk of EBD in adolescents was based on individual factors such as dissatisfaction with body image, which was predicted by being female and BMI, as well as on family factors such as the risk of EBD in the mother (or father), parental age and high use of censorship and criticism as ways of communication with their children, low perceived support and high intrusion, together with the educational level of parents, which, although does not directly predict the risk, does adjust other variables of the parents that have potentiating effect on the risk of EBD in the young people of the sample.
Being a woman and having a high BMI affect satisfaction with body image in young people and adults, who are immersed in a society that is focused on beauty, the cult of the body and youth. Due to widely diffused patterns in different means of communication that transcend the limits of family, the relationship between parents and children is mediated by the concepts they have of what is the acceptable form of the body and what type of eating behavior can lead to achieving it.
Women are the protagonists of fashion and, therefore, attention is focused on them. In addition, the importance given to physical attractiveness to establish affective and interpersonal relationships means that, in relationships, the projected image must be satisfactory for the group in which one seeks to be recognized, even at the expense of one's own mental health; this might even cause that young adults start to obsessively worry about the food they eat and how it influences unwanted weight gain (Elizathe, Murawski & Rutsztein, 2009). At the same time, these obsessive concerns facilitate the emergence of weight control strategies such as the use of laxatives, induced vomiting, and dietary restriction. This need to lose weight in order to achieve the desired body is internalized by young people and, even if they have normal weight, will always seek to lose even more (Pérez & Romero, 2008), especially since the parameters used to judge their body image are constructed based on a number of factors, such as cognition, emotions, social referents, family, and cultural demands (Cash & Pruzinsky, 2002; Fawaz & Soto, 2012).
Participating children consumed, on average, three meals a day with a mid-morning snack that included junk food. In contrast, their parents consumed only two meals a day, a mid-morning snack and sometimes an afternoon snack; they usually did not have breakfast, which they explained with lack of time due to work schedules. The adolescents relied on the accompaniment and control of their parents, while parents self-regulated themselves. This shows that eating behavior requires supervision, which, however, gets lost over the years due to various changes in the family roles, to the activities performed, and even to access to economic resources. This lack of external control affects food intake in terms of quantity, quality, and frequency. For Haines, Gillman, Rifas-Shiman, Field and Austin (2010), family support during food intake is a protective factor that decreases the incidence of eating disorders in young people.
On the other hand, the family component determines the risk of mental health problems in young people, because it represents a figure of authority that does not recognize the fact of being vulnerable to EBD, in such a way that the welfare of children can be put at risk. Given that family serves as the basis for the construction of eating habits and practices, it is possible to understand that if parents have important alterations in their eating behavior, these will be transmitted to children through modeling, which constitutes a prominent risk, especially if parents are unaware of their own risk. In addition, if children do not have healthy eating patterns as an orienting guide, they will model with high precision not only unfavorable eating patterns, but also codes for the construction of their body image and acceptance of the same (Ángel, Gómez & León, 2012).
Taking into account that family is an entity with links that become important during adolescence due to the constant conflicts that young people face, it was found that, for them, both family functioning and support are indispensable when it comes to mitigate the risk of EBD. Factors such as intrusion, censorship and criticism of parents and the little support received are elements that can cause estrangement in the family and thus perpetuate the risk of eating disorders; this explains why these disorders are silent and families do not easily detect them in early stages. If, on the contrary, young people receive support and acceptance despite their physical state, their degree of body satisfaction will not likely to be altered and their patterns of change will likely to be supervised and carried out with responsibility, in order not only to achieve the ideal of beauty, but also to optimize the habits of a healthy life. Haines, Gillman, Rifas-Shiman, Field and Austin (2010) stated that the accompaniment of the family in eating activities not only serves as a protective factor against EBDs, but also enhances the cohesion and quality of family life.
Another important aspect when considering the incidence of family in the development of EBDs was parental age, a condition that revealed that younger parental age is associated with a greater risk for children to present alterations in eating behavior. This may be an explanation for why parents had more risk factors than their children. The literature has been consistent in reporting that from adolescence to adulthood one is susceptible to developing an EBD (Alves, Arroyo, Basabe & Hernández, 2012; López, Molano & Piñeros, 2010). Finally, it is necessary to mention that in order to find the best and most fitted model, parental educational level was also included, although this does not directly predict the risk of EBD. It was not relevant in explaining EBDs, but it did help to modulate other variables such as personal risk of EBD, including the acceptance of cosmetic plastic surgeries to transform a body part that causes dissatisfaction (Alejo et al., 2013; Cabarcas & Londoño, 2014). Similar results were found by Cruz, Iñárritu and Morán (2009) who reported that the variables of educational level and occupation in parents did not result in any statistically significant association.
Based on the present study, it is possible to conclude that the behavior of parents plays an important role in the mental health of the family. The modeling role that parents play for their children allows similar patterns of behavior to be imitated; thus, if parents have some risk of developing eating disorders, it is possible that this is preserved in their children. Given that it is parents who provide and prepare food, it is necessary that their attention will not be focused on exacerbations that are proper to beauty and fashion; although it is important to have food control in terms of quality and components, this must be motivated by health, rather than by responding to patterns of beauty that are highly accepted but little adapted to the anatomical characteristics of Colombians.
One of the main limitations for the study was the sample. Although admission to schools did not represent greater complications and, therefore, students were a captive population, access to parents generated a number of difficulties, since the percentage of attendance to different scheduled and mandatory activities was generally low. On the other hand, the instruments employed represent another important limitation. In the case of EAT-26, its objective is to evaluate the presence of anorexia and bulimia and, considering that there is a greater proportion of the population with an eating disorder not otherwise specified (EDNOS), these subjects would be underdiagnosed; therefore, it is necessary to implement evaluative mechanisms that consider the diagnostic criteria of EDNOS.
References
1. Alejo, I., Londoño, C., Cabarcas, K., Arenas, A., Cortés, A., González, S., et al. (2013). Ansiedad, depresión, afrontamiento y TCA como predictores de cirugías plásticas cosméticas. Suma Psicológica, 20(2), 251-61. doi: http://dx.doi.org/10.14349/sumapsi2013.1471. [ Links ]
2. Alves, D., Arroyo, M., Basabe, N., & Hernández, N. (2012). Del miedo a la obesidad a la obsesión por la delgadez; actitudes y dieta. Nutrición Hospitalaria, 27(4), 1148-55. doi: http://dx.doi.org/10.3305/nh.2012.27.4.5829. [ Links ]
3. Ángel, L. A., Chavarro, K., García, J., Martínez, L. M., & Vásquez, R. R. (2000). Comportamiento alimentario. Validez y fiabilidad de una encuesta. Revista Colombiana de Psiquiatría, 29(1), 29-48. doi: 10.14349/sumapsi2013.1471. [ Links ]
4. Ángel, L., Gómez, M. T., & León, A. (2012). Relación entre las actitudes, comportamiento alimentario e imagen corporal de los padres con las de sus hijos, niños entre los 8 y 11 años en estrato medio en Bogotá. (Thesis). Bogotá: Universidad de la Sabana. [ Links ]
5. Araya, M., & Atalah, E. (2002). Factores que determinan la selección de alimentos en familias de sectores populares. Revista Chilena de Nutrición, 29(3), 308-15. Available at: http://dx.doi.org/10.4067/S0717-75182002000300006. [ Links ]
6. Avellaneda, S. (2009). Determinación de la prevalencia de trastornos de la conducta alimentaria en estudiantes de la Pontificia Universidad Javeriana. (Thesis). Bogotá: Pontificia Universidad Javeriana. [ Links ]
7. Avendaño, C. A., Campo, A. A., Duarte, Z. J.; & Forero, L. M. (2006). Consistencia interna y análisis de factores de la escala APGAR para evaluar el funcionamiento familiar en estudiantes de básica secundaria. Revista Colombiana de Psiquiatría, 35(1), 23-9. Available at: http://www.tandfonline.com/doi/abs/10.1080/00207590042000065. [ Links ]
8. Avendaño, P. G., Castrillón, M. D., Luna, M. I., & Pérez, A. A. (2007). Validación del Body Shape Questionnaire (Cuestionario de la Figura Corporal) BSQ para la población Colombiana. Revista Acta de Colombia, 10(1), 15-23. Available at: http://www.researchgate.net/publication/28172426_Validacin_del_body_shape_questionnaire_(cuestionario_de_la_figura_corporal)_BSQ_para_la_poblacin_colombiana. [ Links ]
9. Bolaños, R. P., & Jáuregui, L. I. (2010). Body image and quality of life in a Spanish Population. International Journal of General Medicine, 4, 63-72. doi: http://dx.doi.org/10.2147/IJGM. [ Links ]
10. Bulika, C. M., Hamera, R. M., Hollea, A. V., Reba-Harrelsona, L., Reichborn-Kjennerudc, T. & Torgersenc, L. (2010). Patterns of maternal feeding and child eating associated with eating disorders in the Norwegian Mother and Child Cohort Study (MoBa). Eating Behaviors, 11(1), 54-61. doi: 10.1016/j.eatbeh.2009.09.004. [ Links ]
11. Bulika, C., & Striegel, R. (2007). Risk Factors for Eating Disorders. American Psychologist, 62(3), 181-98. doi: 10.1037/0003-066X.62.3.181. [ Links ]
12. Cabarcas, K., & Londoño, C. (2014). Afrontamiento, optimismo/pesimismo, imagen corporal y riesgo de TCA como predictores psicosociales de la aceptación de cirugías plásticas cosméticas. Psicología y Salud, 24(4), 199-219. Available at: http://revistas.uv.mx/index.php/psicysalud/article/view/925. [ Links ]
13. Cano, A., Castaño, J., Corredor, D., García, A., González, M., Lucero, K., et al. (2007). Factores de riesgo para trastornos de la alimentación en los alumnos de la Universidad de Manizales. MedUNAB, 10(3), 187-94. Available at: file:///C:/Users/clondo%C3%B1o/Downloads/215-379-1-SM.pdf. [ Links ]
14. Cardozo, R., Guevara, H., Meertens, L., Narváez, R., Ochoa, O., Ordóñez, M. F., et al. (2011). Trastornos de conducta alimentaria en estudiantes de primer Año de Medicina. Vitae, 47, 1-10. doi: 10.1016/S0193-953X(05)70218-5. [ Links ]
15. Cash, T., & Pruzinsky, T. (Eds.). (2002). Body image. A handbook of theory research and clinicalpractice. New York-London: Guilford Press. [ Links ]
16. Castrillón, D., Luna, I., & Aguirre-Acevedo, D. (2007). Validación del Abbreviated Eating Attitudes Test (escala abreviada y modificada de las actitudes alimentarias) EAT-26-M para la población colombiana. In A. Ferrer, Y. Gómez (Eds.), Evaluación e intervención en niños y adolescentes: investigacióny conceptualización (pp. 93-116). Medellín (Colombia): La Carreta Editores. [ Links ]
17. Contreras, J. (2007). Alimentación y religión. Humanidades Médicas, 16, 1-22. Available at: http://www.fundacionmhm.org/tema0716/articulo.pdf. [ Links ]
18. Cruz, V., Iñárritu, M. C., & Morán, I. (2009). Prevalencia de factores y conductas de riesgo asociados a trastornos de la alimentación en universitarios. Revista Médica de México, 72(2), 68-72. doi: 10.3305/nh.2014.30.4.7689. [ Links ]
19. Dancygera, I., Fornaria, V., Sciontic, L., Sunda S., & Wisotskya, W. (2009). Do daughters with eating disorders agree with their parents' perception of family functioning? Comprehensive Psychiatry, 10(1), 22-28. doi: http://dx.doi.org/10.1016/j.comppsych.2004.07.024. [ Links ]
20. Elizathe, L., Murawski, B., & Rutsztein, G. (2009). Hábitos alimentarios e insatisfacción con la imagen corporal. Un estudio comparativo entre mujeres y varones estudiantes de escuelas secundarias. Anuario de investigaciones, 16, 65-72. Available at: www.scielo.org.ar/pdf/anuinv/v16/v16a06.pdf. [ Links ]
21. Erola, A., Toprakc, G., & Yazicib, F. (2007). Family functioning of patients with an eating disorder compared with that of patients with obsessive compulsive disorder. Comprehensive Psychiatry, 48(1), 47-50. doi: 10.1016/j.comppsych.2006.05.004. [ Links ]
22. Espelagea, D. E., Hannum, J. W., Lowa, K. D., & Menoa, C. A. (2008). Familial and individual variables as predictors of dieting concerns and binge eating in college females. Eating Behaviors, 9(1), 91-101. doi: 10.1016/j.eatbeh.2007.06.002. [ Links ]
23. Espinosa, R., Fandiño, A., Giraldo, S., & Martínez, C. (2007). Factores asociados con los trastornos de la conducta alimentaria en estudiantes universitarios en Cali, Colombia. Colombia Médica, 28(4), 344-51. Available at: http://colombiamedica.univalle.edu.co/index.php/comedica/article/view/518/965. [ Links ]
24. Fawaz, J., & Soto, P. (2012). Mujer, trabajo y familia. Tensiones, rupturas y continuidades en sectores rurales de Chile central. La Ventana, 35(07), 218-54. Available at: http://148.202.18.157/sitios/publicacionesite/pperiod/laventan/ventana35/juliafawaz.pdf. [ Links ]
25. García, R., Depetris, E., & Rossini, G. (2013). Consumo de alimentos fuera del hogar en Argentina. Relevancia de la composición demográfica y tipología de los hogares. Población y Salud en Mesoamérica, 10(2). Available at: http://ccp.ucr.ac.cr/revista/. [ Links ]
26. Gempeler, R. J. (2007). La corporalidad funcional como meta terapéutica en el trabajo cognoscitivo-comportamental de los trastornos de la imagen corporal en los TCA: Una reconceptualización. Revista Colombiana de Psiquiatría, 36(3), 451-59. Available at: http://www.redalyc.org/articulo.oa?id=80636305. [ Links ]
27. Godart, N., Legleye, S., Huas, C., Cotél, S., Choquet, M., Falissard, B., et al. (2013). Epidemiology of anorexia nervosa in a French community-based sample of 39,542 adolescents. Open Journal of Epidemiology, 3, 53-61. doi: http://dx.doi.org/10.4236/ojepi.2013.32009. [ Links ]
28. González, A. N., Oudhof Van. B. H. Rodríguez. A. B., & Unikel. S. C. (2010). Desarrollo y validación de una escala para medir imagen corporal en mujeres jóvenes. Salud Mental, 33 (4), 325-332. Recuperado de http://www.scielo.org.mx/scielo.php?pid-S0185-33252010000400004&script-sci_arttext. [ Links ]
29. Haines, J., Gillman, M. W., Rifas-Shiman, S., Field, A. E., & Austin, S. B. (2010). Family dinner and disordered eating behaviors in a large cohort of adolescents. Eating Disorders, 18(1), 10-24. doi: 10.1080/10640260903439516. [ Links ]
30. Hernández, L., & Londoño, C. (2013). Percepción de la figura, índice de masa corporal, afrontamiento, depresión y riesgo de padecer trastorno de conducta alimentaria en jóvenes universitarios. Anales de Psicología, 29(3), 748-61. Available at: http://dx.doi.org/10.6018/analesps.29.3.175711. [ Links ]
31. Kalarchianb, M., Lilenfelda, L., Marcusb, M., & Ringhamb, R. (2008). A family history study of binge-eating disorder. Comprehensive Psychiatry, 49(3), 247-54. doi: 10.1016/j.comppsych.2007.10.001. [ Links ]
32. López, C., Molano, J., & Piñeros, S., (2010). Factores de riesgo de los trastornos de la conducta alimentaria en jóvenes escolarizados en Cundinamarca (Colombia). Revista Colombiana de Psiquiatría, 39(2), 313-28. doi: 10.1016/S0034-7450(14)60253-5. [ Links ]
33. Loubat, O. M. (2006). Conductas alimentarias: Un factor de riesgo en la adolescencia, resultados preliminares en base a grupos focales con adolescentes y profesores. Terapia Psicológica, 24(1), 31-7. doi: 10.4067/S0718-48082011000100009. [ Links ]
34. Ministerio de Protección Social. (2003). Un panorama nacional de la salud y enfermedad mental en Colombia: Estudio Nacional de Salud Mental. Bogotá. Available at: http://onsm.ces.edu.co/uploads/files/1243030_EstudioNacionalSM2003.pdf. [ Links ]
35. Ministerio de Protección Social. (2007). Encuesta Nacional de Salud Indicadores básicos de salud. Bogotá. Available at: http://www.minsalud.gov.co/Documentos%20y%20Publicaciones/ENCUESTA%20NACIONAL.pdf. [ Links ]
36. Pan American Health Organization. (2012). Día Mundial de la salud Mental. Available at: http://www.paho.org/arg/index.php?option=com_content&view=ar-ticle&id=1047&Itemid=325. [ Links ]
37. Pérez, S., & Romero, G. (2008). Imagen corporal en mujeres rurales de la Sierra Juárez y la costa de Oaxaca: una aproximación nutrio-antropológica. Estudios sociales (Hermosillo, Son.), 16(32), 79-111. doi:10.3989/ris.2005.i40.193. [ Links ]
38. Restrepo, N., Hernández, N., Cardona, L., Arango, D., González, G., Puerta, A., et al. (2004). Validación de la escala de envolvimiento emocional y criticismo familiar (FEICS) en la población clínica psiquiátrica colombiana. Revista Colombiana de Psiquiatría, 33(2), 143-62. Available at: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0034-74502004000200002. [ Links ]
39. Rivarola, M., & Penna, F. (2006). Los factores socioculturales y su relación con los trastornos de la conducta alimentaria e imagen corporal. Revista Intercontinental de Piscología y Educación, 8(2), 61-77. Available at: http://redalyc.uaemex.mx/src/inicio/ArtPdfRed.jsp?iCve=80280205. [ Links ]
40. Roberts, M. (2006). Disordered Eating and Obsessive-Compulsive Symptoms in a Sub-clinical Student Population. New Zealand Journal of Psychology, 35(1), 45-54. Available at: http://www.psychology.org.nz/wp-content/uploads/NZJP-Vol351-2006-6-Roberts.pdf. [ Links ]
41. World Health Organization. (2009). Gender and Mental Health. Geneva: Organización Mundial de la Salud. Available at: http://www.Who.int/gender/henderandhealth.html. [ Links ]
![]() Correspondence:
Correspondence:
Constanza Londoño Pérez.
Universidad Católica de Colombia. (Colombia).
E-mail: clondono@ucatolica.edu.co
Article received: 08-09-2015;
Revised: 03-02-2016;
Accepted: 20-02-2016