Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Avances en Odontoestomatología
versión On-line ISSN 2340-3152versión impresa ISSN 0213-1285
Av Odontoestomatol vol.22 no.4 Madrid jul./ago. 2006
Stomathologycal lesions in HIV-1 reactive patients: comparison of proportion in two independent populations
Casariego Zulema*, Fonio S**, Micinquevich S***
* Profesora
Académica de Patología y Clínica Estomatológica y Farmacología y
Terapéutica Aplicada. Facultad de Odontología. Universidad La Plata. Profesora
de la Pontificia Universidad Católica Argentina. Facultad de Posgrado en
Ciencias de la Salud. Buenos Aires.
** Médica Residente de la
Unidad de Infectología. Hospital de Agudos, Juan A. Fernández. Buenos Aires.
Argentina.
*** Profesora Adjunta de
Patología y Clínica Estomatológica. Facultad de Odontología. Universidad
Nacional de La Plata.
SUMMARY
Prevalence of
stomathologycal lesions notably changed after highly active antiretroviral
therapy (HAART). This event is testify by international scientific literature.
Purpose of this study is to diagnose and to register by statistic analysis HIV
oral manifestations comparing in two independent populations.
Study Design:
Stomathologycal lesions were diagnosticated in HIV/AIDS patients by the same
oral specialist. They were attended in our Service during two observation
periodes (OP): 1988-1996 and 1997-2004, 12th hours/week and 6 hours/week
respectively. Confirmation of clinic diagnoses was made by citology,
histopathology, immunohistochemistry and PCR, according to each pathogenesis.
Both times periodes were compare for each pathology by "Comparison
Method per Proportions" (independent munsters) with a signification level:
p<0.05. Data were processed with EPIDAT, version 3 (YUNTA OF GALICIA-
OPS/OMS).
Results:
OP1=2873 pathologies, OP2=520. Comparison in both OPs was: statistical
signification p<0.05: Eritematous and Pseudomembranous Candidiasis (EC),PSC),
Hairy leukoplakia (HL), Recidivant aphtous ulcers (RAU), Angular Cheilitis (ACH),
Papilloma Human Virus (HPV), Herpes Virus (HV), and Non-Hodking Limphoma (NHL).
Withow statistic significance: Acute necrotizing gingivitis (ANUG) and Kaposi
Sarkoma. (KS). In the second OP, RAU, HPV and HSV shawed significantly statistic
differences, specially RAU with 44,2% of prevalence.
Conclusions: 1)
Our results could confirm declining prevalence of most of oral manifestations of
HIV infection in HAART era. 2) We stand out the significance of RAU, HPV and HSV
prevalences in the last period of time.
Key words: Stomatological lesions, comparison of proportion.
Introduction
During the last years highly active antiretroviral therapy (HAART) have produce very important consequences on viral decrease replication in HIV-1 infected and ill patients. HIV RNA levels (viral load), morbidity and mortality scores achieved significantly improvements (1,2). From the beginning of infection many oral mucosa manifestations had been detected as on annexes oral cavity organs as well. All of them were considered as infection predictors (3-7). Now a day, the landscape is changed according to the international bibliography (8,9). On patients from those countries where they receive cost- free antiretroviral medication, the incidence and prevalence of oral lesions have considerably diminish (10,11). Since 1996 new studies of orall lesions prevalence were performed according to the evolution and expectation of this pandemia.
Our objectives for this presentation were: to diagnose and to register from an statistic point of view the prevalence of oral lesions on HIV-1 patients comparing two different populations in two periods of time: pre and post HAART.
Material and Methods
There were analyzed two periods of time: 1988-1996, with 2873 registered lesions and 1997-2004 with 520. The first ones were diagnosed by the same consultant according the "First Simposium of AIDS investigation in Latin America and Caribe (OSM) Río de Janeiro, Brasil, 1988 and, the second one, according to "EC Clearing House Criteria on Oral Problems related to HIV infection" 1993.
Data were analyzed comparing two observations periods for each pathology applying the statistical study using the comparison method per proportions for independent samples with a signification level p<0.05. Data were processed with EPIDAT, version 3.0. Xunta de Galicia OPS/OMS.
Results were tabulated and studied for both periods of time. EC erithematous candidiasis, PSC pseudomembranous candidiasis, HL, hairy leukoplakia, RAU, recurrent aphthous ulcers, ANUG, acute necrotizing gingivitis, KS, Kaposi sarcoma, HPV Human Papilloma Virus, HSV Herpes virus and NHL, Non Hodking Lymphoma were confirmed by clinic diagnoses, cytology, culture, histopathology, immune histochemistry and PCR for viral types. Clinic observation was made by the same observer during 12 hours/week, first period and 6 hour/week, the second one.
Results
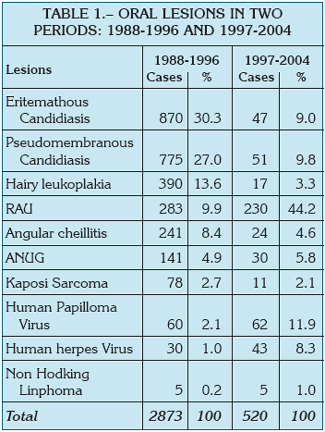
During the first observational period 2873 0ral lesions were diagnosed (319.2 (per year), while in second period 520 were identified (65 per year) (table 1).
Comparison of prevalences were registered as: RAU (44.2%)), HPV 11.9% and HSV 8.3% in the second period with statistical significant differences (p<0.05) (table 2).
This results can be observed more evidently on graphic data (1).

Discussion
Participants of the "5th Workshop on Oral Health and Disease in AIDS" from 6 to 10 July 2004, Phuket, Tayland (13) accepted to analyze the recovering and improvement of oral lesions associated with HIV/AIDS and to develop further meetings where might be discuss different subjects about Health Oral Conditions in relationship with HIV infection. With this purpose we have observed that the impact of antiretroviral drug combination treatments and investigations about HIV/AIDS pathogenesis since 1995 have contributed in the diminution of the incidence and prevalence of oral diseases (11, 16, 17). We can say that this is not the case of Zimbabwean (18) within 18.6% of KS and 3.8% of Crancun Oris (that its not registered in our land), or South India (19) that have published from 300 patients, ANUG 47% and PSC 33%, or Nigeria were it is a great score of social stigma and discrimination, where do not exist a Public Health support on HIV infection and were it is observed also, that not exist an appropriated management for salivary gland lymphoepithelial lesions, commonly observed in children.
It´s interesting that in spite of the HAART new era, there are some prospective studies that have shown really no benefit in short –term viral outcomes. The emergence of drug resistant viral variants presents a significant challenge to effective antiretroviral intervention. The themes that arise are patient adherence to medications, something that is a profoundly strong determinant of outcomes, both virology and clinical outcomes. Resistant associated mutations after multiple treatment failures, drug resistant viruses become more routine and widespread (21,22). Perhaps of this reason oral pathology has not decrease to 0% and we can yet observe patients with lesions that we believed they have been disappeared but they return in acute and morbid processes.
On the contrary, we have found that recurrent aphthous ulcers or major ulcers (RAU) and Human Papilloma Virus associated lesions in oral mucosa present highly statistic scores, specially the first ones.
Knowing the physio-pathogenesis of RAU (23) and the coincidence between our last results with the last publications from the two mentioned viral infections (24-28) in patients under HAART we ask ourselves if are we in a way of a new investigation field.
Conclussions
1. Introduction of new highly active antiretroviral therapy have given, as result, in our studied population, a significantly statistic reduction of lesions associated with HIV infection, in the analyzed period of time under HAART.
2. We point out as exception the high prevalence in HAART era of Recurrent Aphthous Ulcers (RAU) and with lower value but, with a statistic significantly difference, oral lesions caused by HPV and HSV as well.
3. We consider there are necessary further investigations to understand and recognized the most representative oral lesions associated with HIV/AIDS in the future.
![]() Correspondence
Correspondence
Prof. Dra. Zulema Casariego
Bartolomé Mitre, 1371- 4M-
1036 Buenos Aires. Argentina
T/FAX: 0054-11-4-3720444
Correo electrónico: patología@folp.unlp.edu.ar
Acepted for publication: July 2005.
References
1. Richman Douglas. Progress and Challenges in HIV Therapy. The Art of HIV, 2002-Dec. [ Links ]
2. Flexner Charles W. Perspectives. Update on HIV Pharmacology and Therapy Drug monitoring International AIDS Society-USA-Topics in HIV meedicine. 2001 July; 9(3):4-7. [ Links ]
3. Green TL; Beckstead JH; Lozada-Nur F, Silverman S Jr; Hansen LS. Histopathologic spectrum of Oral kaposis sarcoma. Oral Surg Oral Med Oral Pathol 1984;58:306-14. [ Links ]
4. Greenspan D, Greenspan J, Pindborg JJ, et al. Oral manifestations of infections diseases. In: AIDS and the Dental Team, Copenhagen Munksgaard 1986; pp 35-61. [ Links ]
5. Barr CE, Torosian JP: Oral manifestations in patients with AIDS or AIDS-related complex. Lancet 1986;2:288. [ Links ]
6. Ficarra G, Lozada –Nur F, Grenspan D, Hansen LS, Green TL. Síndrome de Inmunodeficiencia acquisita (AIDS): lesión del cavo orale. (Acquire immunodeficiency síndrome (AIDS): lesions in the mouth). Mondo Odontoestomatol 1986; 28:17-26. [ Links ]
7. Murray PA, Winkler JR, Sadowsky L, et al. Microbiology of HIV-associated gingivitis & periodontitis IN: Robertson PB, Greenspan J, Eds Oral manifestations of AIDS. Mass SG Publishing 1988; 107-17. [ Links ]
8. Cruz GD, Lamster IB, Begg MD, Phelan JA, Gorman JM, el-Sadr W. The accurate diagnosis of oral lesions in human immunodeficiency virus infection. Impact on medical staging. Arch Otolaryngol Head Neck Surg 1996 Jan; 122(1): 68-73. [ Links ]
9. Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ Jr. Chaging prevalence of oral manifestations of human immuno-deficiency virus in the era of protease inhibitor therapy. Lauren –Patton@Dentistry.UNC.EDU. [ Links ]
10. Eyeson JD, Tenant-Flowers M, Cooper DJ, Johnson NW, Warnakulasuriya KA. Oral manifestations of an HOV poasitive cohort in the era of highly active anti-retroviral therapy (HAART) in South London. J Oral Pathol Med 2002 Mar; 31(3):169-74 [ Links ]
11. Ramirez-Amador V, Esquivel-Pedraza L, Sierra-Madero J, Anaya-Saavedra G, Gonzalez-Ramirez I, Ponce-de Leon S.: The Changing Clinical Spectrum of human immunodeficiency Virus (HIV) Related Oral lesions in 1.000 Consecutive Patients: A 12 –Year Study in a referral center in mexico. Medicine(Baltimore) 2003 Jan; 82(1):39-50. [ Links ]
12. Casariego Zulema, Ben Graciela. Manifestaciones bucales de la infección por VIH en Argentina: estudio de 1889 casos. Medicina Oral, 1998 Nov-Dec; 3(5):271-76 [ Links ]
13. The Phuket Declaration on Oral Health in HIV/AIDS 2004: Oral Diseases 2005;11:1-2 [ Links ]
14. Sradthdee SA, Craib KSP, Hogg RS, OShaughnessy MV, Montaner JSG, Schechter MT. Long term non- progression in HIV-infection. A cautionary note. Lancet 1995;346:1372 [ Links ]
15. Miró JM, Martínez Chamorro E, Peña JM. Restauración inmunológica y tratamiento antirretroviral de gran actividad (TARGA) En: Avances en el manejo del paciente infectado por HIV. Podzamczer D. Ed. team Pharma, madrid 1999; 152-70. [ Links ]
16. Shiboski CH, Wilson CM, Greenspan D, Hilton J, Greenspan JS, Moscicki AB; Adolescent medicine HIV/AIDS Research network. J Adolesc Health 2001,Sep; 289 (3Suppl):109-14. [ Links ]
17. Mocrofot A, Vella S, Benfield TL, et al. Surveillancepatterns of mortality across Europe in patients infected with HIV-1. Euro-SIDA Study Group. Lancet 1998;352:1725-30. [ Links ]
18. Chidzonga MM. HIV/AIDS orofacial lesions in 156 Zimbabwenan patients at referral oral and maxillofacial surgical clinics. Oral Dis 2003 Nov; 9(6):317-22. [ Links ]
19. Ranganathan K, Reddy BV, Kumarasamy N, Solomon S, Viswanathan R, Johson NW. Oral lesions and conditions associated with human immunodeficiency virus infection in 3000 souith Indian patients. Oral Dis 2000 May; 6(3): 152-7. [ Links ]
20. Owotade FJ, Fatusi OA, Adebiyi KE, Ajike SO, Folayan MO. Clinical experience with parotid gland enlargement in HIV infection: a repoprt of five cases in Nigeria. Contemp Dent Pract. 2005 feb 115;6(1):36-45. [ Links ]
21. Simon Viviana A.: Hiv-1 drug ressistance testing IAPAC Monthly. 2001 Aug; 7(8):235-37. [ Links ]
22. Sherer Renslow: limitations and uncertancities of resistance testing: a review of "negative"trials. IAPAC Monthly. 2001 Aug;7(8):237-41. [ Links ]
23. Casariego ZJ, Herrero T, Pombo T. Estudio Inmunohistoquímico de úlceras Aftosas Recidivantes (RAU) en dos subpoblaciones: pacientes RAU+(VIH-), RAU+ (VIH+), versus RAU/VIH+ y población control RAU-/VIH-AVANCES en Odontoest. 2001 Oct;17(8):399-418. [ Links ]
24. Leigh JE, Shetty K, Fidel PL jr. Oral opportunistic infections in HIV-positive individuals: review and role of mucosal immunity. AUIDS Patrient care STDS 2004 Aug;18(8):443-56. [ Links ]
25. Doherty R, Tanskanen E, Churchill MJ, deacon NJ. Interaction between human immunodeficiency virus and human papillomavirus. VIII international Conference on AIDS, Amsterdan 1992 July. [ Links ]
26. King MD, Reznik DA, ODanils CM, Larsen NM, Osterholt D, Blumberg HM. Human papillomavirus –associated oral warts among human immunodeficiency-virus serpositive patients in the era og highly active antiretroviral therapy: an emerging infection. [ Links ]
27. Grenspan D, Canchola AJ, Mac Phail LA, Cheikh B, Greenspan JS. Effect opg highly active antiretroviral therapy on frequency of oral warts. Lancet 2001;357:1411-2. [ Links ]
28. Stone SF, Price P, Brochier J, French MA. Plasma bioavailable interleukin-6 is elevated in human immunedeficiency virus-infected patients who experience herpesvirus-associated immune restoration disease after start of highly active antiretroviral therapy. J Infect Dis 2001;184: 1073-7. [ Links ]











 texto en
texto en