Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
The European Journal of Psychiatry
versão impressa ISSN 0213-6163
Eur. J. Psychiat. vol.23 no.3 Zaragoza Jul./Set. 2009
Somatization and psychological awareness of ethnic minority clients in Western-European mental health care: A pilot study
Marrie H.J. Bekker, PhD; Roel Schepman, MSc
Faculty of Social and Behavioural Sciences. Department of Developmental, Clinical and Cross-Cultural Psychology. Tilburg University. Tilburg. The Netherlands
Somatization, expressing psychological distress through physical symptoms that cannot be attributed to medical illnesses1,2, is a core symptom of somatoform disorders3 and presents a significant problem to clinicians4,5. Prevalence rates range from 0.03%6 to 19.7%7. Immigrants, especially from less industrialized countries, are often assumed to express distress more through somatization, people from "Western" countries through psychological symptoms8-10. Such differences could seriously complicate Western health care for immigrants that usually focus on either physical or psychological health11. Moreover, medically unexplained somatic symptoms are often resistant to medical treatment, and somatizing clients' attitude towards psychosocial treatment can result in unfavourable therapy outcome12-14.
Most studies on somatization did not show significant differences between "Western" and "non-Western" clients2,7,15, but others did16,17, maybe due to varying ethnic groups. Moreover, most ethnic U.S.-minorities are Asian, Hispanic, or African-American, whereas those in Western Europe come from Mediterranean countries like Turkey and Morocco18. The present pilot-study provides a first comparative indication of somatization tendencies between native clients and those belonging to European minorities.
Also, we examined the relationship of somatization in these groups with psychological mindedness (PM) and autonomy-connectedness. PM, assumed to be lacking in somatizing clients19, is the motivation and ability to explore and understand psychological processes within one-self and others20, which seems relevant for successful psychological treatment21-23. We therefore expected higher PM-levels to be positively related to higher levels of attributing symptoms to psychological causes, and lower PM to more somatic attributions. In Western-Europe and North-America, becoming an autonomous individual might be more important for personal development (and treatment) than in more "collectivistic" cultures. Autonomy-connectedness, the need and capacity for self-reliance and independence, as well as for intimacy and functioning satisfactorily in intimate relationships24-26, has three components24,25,27: Self-awareness (SA; awareness of ones feelings, wishes and opinions), Sensitivity of Others (SO; sensitivity of others' needs and opinions, the ability of empathy, intimacy and separation), and Capacity for Managing New Situations (CMNS; the ability to feel at ease in new situations). We expected individuals with low SA to be less inclined explaining their symptoms psychologically. As Korean, more other-directed immigrants were found to have elevated somatization levels, and those more self-directed to psychologize more22, we expected that the higher one's SO would be, the more one might somatize. This expectation was also prompted by stigma: physical illnesses seem less stigmatizing than psychiatric illnesses, and SO might also include (sensitivity to) stigma2,28,29.
We tested all hypotheses in 2 patient samples (32 native Dutch, 24 ethnic minority Dutch; age 18-61) scheduled for standard intake procedures at an ambulatory mental health care institution in the South of the Netherlands. All clients presented predominantly with mood-, anxiety-, and adjustment disorders (additionally presented, e.g. somatoform, complaints were not recorded). Included in the ethnic minority group (mostly from Turkey or Morocco) were clients who, themselves and/or (one of) their parents, had not been born in the Netherlands and understood the Dutch language. They appeared lower-level educated than the native Dutch respondent; no other socio-demographic differences were found.
We measured somatization with the 13-item Symptom Interpretation Questionnaire (SIQ; subscales Psychological-, Somatic-, and Externalizing Attribution Style)30,31 and psychological mindedness with the 24-item Tilburg Psychological Mindedness Scale (TPMS-24; subscales: Lack of Monitoring and Insight; Avoidance of Feelings; and Positive Attitude towards Feelings)32. Autonomy-connectedness was assessed with the Autonomy-Connectedness Scale (ACS-30; subscales SA, SO, and CMNS definitions see before)24,25,27,33,34. Reliability of all scales was satisfactory, except for CMNS (ethnic minority sample), which we excluded from further analyses*.
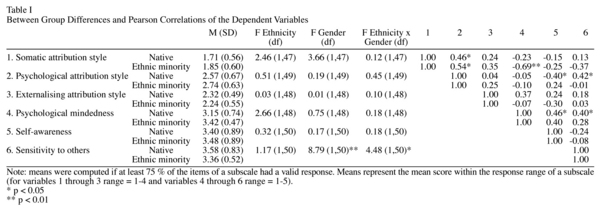
ANCOVA on all dependent variables, controlled for education and gender, did not reveal any between-group difference (see Table I). Women compared with men scored significantly higher on SO, and a significant gender x ethnicity interaction effect appeared; with higher SO in native than in ethnic minority women, and similar SO in men of both groups.
Correlational analyses, for both samples separately (Table I), revealed positive correlations between somatic- and psychological attribution for both the native and the ethnic minority sample; both were un-correlated with externalising. PM correlated negatively with somatic attribution (both samples), but only significantly for ethnic minority clients. In native clients psychological attribution correlated negatively with SA but positively with SO. For native clients, PM was positively correlated with SA and SO; these correlations were non-significant in the ethnic minority sample.
In short, ethnic minority clients did not use a somatic, psychological, or externalising attribution style more frequently, neither showed any differences on PM, SA, and SO. The assumption that ethnic minority clients attribute somatically more often, possess less introspective ability, and tend to be more led by the expectations of other people, had to be rejected.
For both the native and the ethnic minority sample, the use of somatic and psychological attribution styles were positively correlated, suggesting that for all clients somatic and psychological causes can both, simultaneously, explain the same symptoms. Maybe individuals do not differ that much in what causes they attribute but rather in their tendency to search for causes anyhow, regardless of their nature. Apparently, somatic and psychological attribution do not clearly represent two mutually exclusive categories of symptom presentation, supporting that somatization is dimensional rather than categorical35,36.
Women's higher SO than men's agrees completely with previous findings24,27 as does the surprising finding of higher SO in native compared to ethnic minority Dutch women34.
The remarkable correlational differences between both samples may indicate that PM, SA, and SO represent (partly) different concepts for native and ethnic minority Dutch clients. Further research with larger sample sizes should clarify these concepts' structural equivalence.
That the ethnic background of clients solely did not affect somatisation tendencies is also supported by other studies37,38 targeting other ethnic groups in other countries. Nevertheless, other cultural factors might influence somatisation, e.g. acculturation-related factors17,39.
Study limitations hampering the generalizability of results are the rather small sample sizes, the inclusion of Dutch-speaking participants only, a rather limited ethnicity measure, and lacking information recorded on secondary diagnoses. Future research should therefore use larger, more diverse samples, and more checks and measures.
We conclude that the relationship between ethnicity and somatization is not as straightforward as commonly assumed. The dualistic vision on separate somatic and psychological health persisting also in Western-European health appeared not at all reflect clients' perspective of health; they used somatic and psychological attribution styles without one excluding the other. A priori assumptions regarding illness-representations of ethnic minority clients, understandable from possible uncertainty of therapists40, should be avoided, e.g., by better training41.
References
1. Aragones E, Labad A, Pinol JL, Lucena C, Alonso Y. Somatized depression in primary care attenders. J Psychosom Res 2005; 58: 145-151. [ Links ]
2. Keyes CL, Ryff CD. Somatization and mental health: a comparative study of the idiom of distress hypothesis. Soc Sci Med 2003; 57: 1833-1845. [ Links ]
3. APA. Diagnostic and statistical manual of mental disorders (fourth ed. TR). APA; 2000. [ Links ]
4. Avila LA. Somatization or psychosomatic symptoms? Psychosom 2006; 47: 163-166. [ Links ]
5. De Gucht V, Fishler B. Somatization: a critical review of conceptual and methodological issues. Psychosom 2002; 43: 1-9. [ Links ]
6. Escobar JI, Burnam MA, Karno M, Forsythe A, Golding JM. Somatization in the community. Arch Gen Psychiat 1987; 44: 713-718. [ Links ]
7. Gureje O, Simon GE, Ustun TB, Goldberg DP. Somatization in cross-cultural perspective: a World Health Organization study in primary care. Am J Psychiat 1997; 154: 989-995. [ Links ]
8. Bekker MJH, Frederiks E, editors. Psychotherapeuten over diversiteitsbewuste werkwijzen en knelpunten bij intake, diagnostiek en behandeling van allochtone vrouwen en mannen. Amersfoort: GGZ Kennisnet; 2005. [ Links ]
9. Kirmayer LJ. Cultural variations in the clinical presentation of depression and anxiety: implications for diagnosis and treatment. J Clin Psychiat 2001; 62: 22-28. [ Links ]
10. Bäärnhielm S, Ekblad S. Turkish migrant women encountering health care in Stockholm: a qualitiative study of somatization and illness meaning. Cult Med Psychiat 2000; 24: 431-452. [ Links ]
11. De Gucht V, Maes M. Explaining medically unexplained symptoms: toward a multidimensional, theory-based approach of somatization. J Psychosom Res 2006; 60: 349-352. [ Links ]
12. Timmer B, Bleichhardt G, Rief W. Importance of psychotherapy motivation in clients with somatization syndrome. Psychother Res 2006; 16: 348-356. [ Links ]
13. Allen LA, Escobar JI, Lehrer PM, Gara MA, Woolfolk RL. Psychosocial treatment for multiple unexplained physical symptoms: a review of the literature. Psychosom Med 2002; 64: 939-50. [ Links ]
14. Kolk AM, Schagen S, Hanewald GJ. Multiple medically unexplained physical symptoms and health care utilization: outcome of psychological intervention and patient-related predictors of change. J Psychosom Res 2004; 57: 379-389. [ Links ]
15. Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol 2003; 112: 437-447. [ Links ]
16. Aragona M, Tarsitani L, Colosimo F, Martinelli B, Raad H, Maisano B, et al. Somatization in primary care: a comparative study of immigrants from various ethnic groups in Rome, Italy. Int J Psychiat Med 2005; 35: 241-8. [ Links ]
17. Parker G, Chan B, Tully L, Eisenbruch M. Depression in the Chinese: the impact of acculturation. Psychol Med 2005; 35: 1-9. [ Links ]
18. Dieperink C, Van Dijk R, Wierdsma A. GGZ voor allochtonen. Maandblad Geestelijke Volksgezondheid 2002; 57: 87-97. [ Links ]
19. Schepman RJ. Somatisatie bij allochtone cliënten in de GGZ: mythe of feit? Metaforum 2006; 8: 8-14. [ Links ]
20. Beitel M, Ferrer E, Cecero JJ. Psychological mindedness and awareness of self and others. J Clin Psychol 2005; 61: 739-750. [ Links ]
21. Trudeau KJ, Reich R. Correlates of psychological mindedness. Pers Ind Diff 1995; 19: 699-704. [ Links ]
22. McCallum M, Piper WE, Ogrodniczuk JS, Joyce AS. Relationships among psychological mindedness, alexithymia and outcome of four forms of short-term psychotherapy. Psychol Psychother 2003; 76: 133-144. [ Links ]
23. Kitayama S, Markus HR, Matsomoto H, Norasakkunkit V. Individual and collective processes in the construction of the self: self-enhancement in the US and self-criticism in Japan. J Pers Social Psychol 1997; 72: 1245-1267. [ Links ]
24. Bekker MJH, Van Assen MALM. A short form of the Autonomy scale: Properties of the Autonomy-Connectedness Scale. J Pers Assessm 2006; 86: 51-60. [ Links ]
25. Bekker MJH. The development of an Autonomy scale based on recent insight into gender identity. Eur J Pers 1993; 7: 177-194. [ Links ]
26. Hmel BA, Pincus AL. The meaning of autonomy, on and beyond the interpersonal circomplex. J Pers 2002; 70: 277-308. [ Links ]
27. Bekker MJH, Van Assen MALM. Autonomy-connectedness and gender. Sex Roles 2008; 59: 532-544. [ Links ]
28. Kirmayer LJ, Looper KJ. Abnormal illness behaviour: physiological, psychological and social dimensions of coping with distress. Curr Opin Psychiat 2006; 19: 54-60. [ Links ]
29. Raguram R, Weiss MG, Channabasavanna SM, Devirs GM. Stigma, depression, and somatisation in South India. Am J Psychiat 1996; 153: 1043-1049. [ Links ]
30. Robbins JM, Kirmayer LJ. Attributions of common somatic symptoms. Psychol Med 1991; 21: 1029-1045. [ Links ]
31. Gijsbers-Van Wijk E, Kolk A. Psychometric evaluation of symptom perception measures. Pers Ind Diff 1996; 20: 55-70. [ Links ]
32. Denollet J, Nyklícek I. Psychological mindedness: a forgotten emotion-focused coping style? In: Nyklícek I, Temoshok LR, Vingerhoets AJJM, editors. Emotional expresssion and health: Advances in theory, assessment and clinical applications. London: Brunner-Routledge; 2004. p. 185-203. [ Links ]
33. Bekker MJH, Hens G, Nijssen A. Stress prevention training: Sex differences in types of stressors, coping, and training effects. Stress Health 2001; 17: 207-218. [ Links ]
34. Bekker MJH, Arends-Tóth J. Autonomy-connectedness, acculturation, and independence-interdependence among various cultural groups in a multicultural society. Under review. 2008. [ Links ]
35. Katon W, Lin E, Von Korff M, Russo J, Lipscomb P, Bush T. Somatization: a spectrum of severity. Am J Psychiat 1991; 148: 33-40. [ Links ]
36. Kirmayer LJ, Robbins JM, Paris J. Somatoform disorders: personality and the social matrix of somatic distress. J Abnorm Psychol 1994; 103: 125-136. [ Links ]
37. Miranda J, Siddique J, Belin TR, Kohn-Wood P. Depression prevalence in disadvantaged young black women. African and Carribean immigrants compared to US-born African Americans. Soc Psychiat Psychiatric Epidem 2005; 40: 253-258. [ Links ]
38. Piccinelli M, Simon GE. Gender and cross-cultural differences in somatic symptoms associated with emotional distress. An international study in primary care. Psychol Med 1997; 27: 433-444. [ Links ]
39. Ritsner M, Ponizovsky A, Kurs R, Modai I. Somatization in an immigrant population in Israel: a community survey of prevalence, risk factors, and help-seeking behavior. Am J Psychiat 2000; 157: 385-392. [ Links ]
40. Perron NJ, Hudelson P. How do junior doctors working in a multicultural context make sense of somatisation? Swiss Med Weekly 2005; 135: 475-579. [ Links ]
41. Farsimadam F, Draghi-Lorenz R, Ellis J. Process and outcome of therapy in ethnically similar and dissimilar therapeutic dyads. Psychother Res 2007; 17: 567-575. [ Links ]
![]() Correspondence:
Correspondence:
Marrie H.J. Bekker, PhD
Department of Clinical Psychology
Tilburg University
P.O. Box 90153
5000 LE Tilburg
The Netherlands
Tel: 00-31-(0)13-4662366/2167
Fax: 00-31-(0)13-4662370
E-mail: m.h.j.bekker@uvt.nl