Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
The European Journal of Psychiatry
versão impressa ISSN 0213-6163
Eur. J. Psychiat. vol.24 no.3 Zaragoza Jul./Set. 2010
Cognitive deficits in hospitalized and never hospitalized remitted unipolar depressive patients
Marek Preiss*; Hana Kucerova**; Jiri Lukavsky***; Petr Sos*; Hana Stepankova*; Radka Cermakova*
* Prague Psychiatric Center
** The Faculty Hospital Brno, Brno
*** Academy of Sciences, Prague. CZECH REPUBLIC
Funding for this study was provided by MSMT 1M0517.
ABSTRACT
Background and Objectives: Little is known about the differences between patients managing depression on an outpatient basis as compared with hospitalized ones. This study investigated the performance of attention, executive function and verbal memory during remission from unipolar depressive episodes and compare patients with and without history of hospitalization.
Methods: The sample of participants who had undergone one or more hospitalizations (hospitalized, N = 46) as well as in a sample without hospitalization (never hospitalized, N = 46) and controls (N = 92) were used. The Auditory Verbal Learning Test (AVLT) and the Trail Making Test (TMT) were administrated to test this hypothesis.
Results and conclusion: The hospitalized sample had similar results in all four neuropsychological variables in comparison with the never hospitalized group, and both groups had some lower results in comparison with controls. In comparison with the controls, hospitalized sample had mean cognitive deficits of 34% (28-41%), the never hospitalized group had a mean of 20% (21-35%). Contrary to previous reports we have found no meaningful differences between the two patient groups.
Key words: Hospitalization; Major depressive episode; Remission; Cognitive function; Course of illness; Outcome.
Introduction
Major depression is a prevalent and disabling disorder with high rates of recurrence and chronicity1-2. Cognitive impairment is likely to be a key factor affecting the subject´s ability to function occupationally3-6. The "therapeutic" aspects of mental hospitalization are generally taken for granted, and are usually considered to comprise protection, separation from a potentially pathogenic environment, and positive contact between patients and staff7.
Kessing8, who studied patients with primary affective disorders who had undergone hospitalization for depression, mania or a recurrent episode, and with no further admissions or with 2 more additional admissions, found that cognitive impairment appears to increase with the increasing number of episodes a patient has experienced. On the other hand, patients with a history of more than one hospitalization did not show any differences compared to patients experiencing their first hospitalization on most of the neuropsychological tests and clinical variables9. We might think that impaired cognitive performance in hospitalized patients relates to the fact that people with more severe symptomathology are hospitalized. The patients with a history of hospitalization had worse results than those without such a history10-11. Neuropsychological assessment is an ideal strategy for obtaining collaborative data in a psychiatric population due to the presumed absence of self-report bias12. We assumed that remitted patients who were previously hospitalized would demonstrate worse impairment of attention, memory and executive function in comparison to those remitted patients who had never been hospitalized.
Material and Methods
Sample
The study was conducted with 92 unipolar depressive outpatients (42 men and 50 women; Table 1 and 2). All the patients met the criteria for formerly having major depressive disorder according to ICD-10. All patients were in a remitted state at the time of testing. Remission was defined as a period of at least 2 months during which the subject functioned well (subjectively according to the patient and objectively according to their psychiatrist) and the MADRS on the day of study < 12. Patients were divided into two groups: never hospitalized (N = 46) or hospitalized (N = 46). Controls were recruited from the general population and they were matched for age, gender and education with the test groups (Table 1).
Individuals with mental retardation (IQ < 70 according to subtest Information from WAIS-R, scale score 6 and lower), dementia, substance abuse/dependence, neurological disorders or clinical/laboratory indications of a severe organic disease, actual or prior bipolar I or II were not counted. Written consent was obtained and the study was approved by the Ethical Regional Committee for Medicine of Prague Psychiatric Center.
Methods
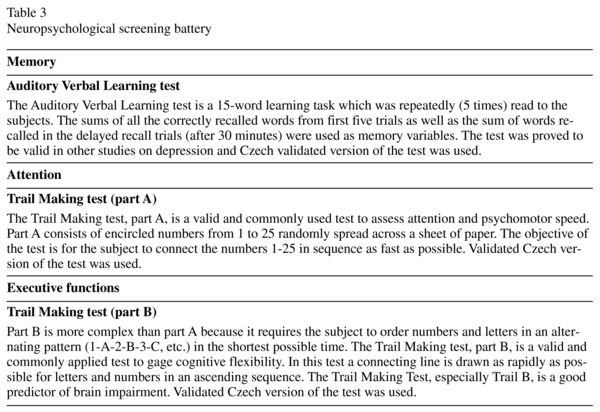
All subjects were given a battery of short neuropsychological tests (Table 3). Traditional neuropsychological criteria for cognitive impairment would identify those individuals who performed better than 1 SD below the healthy control mean as "unimpaired"13-14.
Results
As can be seen in Table 2, groups were well matched. The number of hospitalizations was rather small in the hospitalized group (M = 1.9, SD = 1.0; maximum 5 hospitalizations). On average, hospitalized patients had been hospitalized 4 years prior (M = 4.2, SD = 3.9). The mean duration of illness was 17.8 years in the hospitalized group and 12.3 in never hospitalized group. The average age of the first depressive episode was 29.4 resp. 29.6 years. The mean number of depressive episodes was subjectively 2.9 vs. 2.4 and according to medical records 2.5 vs. 1.8.
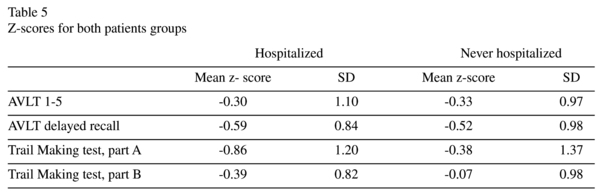
Performance of both groups is presented in Table 4. Mean z-scores of patients and controls are seen in Table 5. In comparison with the controls, all mean z-scores for the depressive groups are lower. The hospitalized sample had cognitive deficits in the AVLT Trial (28%), in AVLT delayed recall (35%), in the Trail Making Test, part A (41%), and in Trail Making test, part B (30%). The never hospitalized sample demonstrated signs of cognitive deficit in the AVLT Trial (33%), in the AVLT delayed recall (35%), in the Trail Making Test, part A (22%), and in the Trail Making test, part B (21%). In total, 34% of the hospitalized sample had cognitive deficits, and 20% of the never hospitalized sample presented the same deficiencies (p = 0.134).
Discussion
The hospitalized sample did not have worse results in any from 4 neuropsychological tests compared to the never hospitalized sample. The only statistically significant difference in comparison with controls was in the Trail Making test, part A, with worse performance found in the hospitalized sample and in AVLT delayed recall for both depressive samples.
Both depressive samples had significantly higher levels of subjective depressiveness according to the BDI-II in comparison with controls. These results may suggest that certain residual depressive symptomatology may affect performance in neuropsychological tests. This may be true despite the fact that no relationship between neuropsychological tests and BDI-II/MADRS was proven, besides the correlation between the MADRS and TMT-B scores (r = -0.33, p = 0.001).
In our data, we did not find a relationship between the number of hospitalizations and the subjectively reported depressive episo-des as well as cognitive performance for separate groups, but for the whole sample of depressive patients this link was found (r = -0.27, p = 0.008 and -0.33, p = 0.003). Some negative effects of repeated depressive episodes were found in one of the four neuropsychological measures. These findings are and have been considered controversial in older studies15. Other studies and papers have also failed to find differences between first and recurrent episodes16.
The performance of both depressive groups is below the mean scores of the controls, but does not exceed 66% in the hospitalized sample and 80% in the never hospitalized sample, -1 SD below the mean of controls. Level of cognitive deficits varied in hospitalized sample from 28-41% and in never hospitalized from 21-35%. According to Gauss curve, in this range should be about 15.86% patients.
References
1. Ayuso-Mateos JL, Vázquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, et al. Depressive disorders in Europe: Prevalence figures from the ODIN group. Brit J Psychiat 2001; 179: 308-316. [ Links ]
2. Marvel CHL, Paradiso S. Cognitive and neurological impairment in mood disorders. Psychiatric Clinics of North America 2004; 27: 19-36. [ Links ]
3. Hirchsfeld RMA. Long-term nature of depression. Depress Anxiety 1998; 7: 1-4. [ Links ]
4. Ormel J, Oldehinkel AJ, Nolen WA, Volleberg W. Psychosocial disability before, during, and after a major depressive episode. Arch Gen Psychiat 2004; 61: 387-392. [ Links ]
5. Basso MR, Bornstein RA. Neuropsychological deficits in psychotic versus nonpsychotic unipolar depression. Neuropsychology 1999;13:69-75. [ Links ]
6. Thase ME. Defining remission in patients treated with antidepressants. J Clin Psychiat 1999; 60: 3-6. [ Links ]
7. Zaslove MO, Ungerleider T, Fuller M. How psychiatric hospitalization helps: Patient views v.s. staff views. J Nerv Ment Dis 1966; 142: 568-576. [ Links ]
8. Kessing LV. Cognitive impairment in the euthymic phase of affective disorder. Psychol Med 1998; 28: 1027-1038. [ Links ]
9. Harvey PO, Bastard G, Pochon JB, Levy R, Allinaire JF, Dubois B, et al. Executive functions and updating of the contents of working memory in unipolar depression. J Psychiat Res 2004; 38: 567-576. [ Links ]
10. Elliott R, Sahakian BJ, McKay AP, Herrod JJ, Robbins TW, Paykel ES. Neuropsychological Impairments in Unipolar Depression: The Influence of Perceived Failure on Subsequent Performance. Psychol Med 1996; 26: 975-989. [ Links ]
11. Purcell R, Maruff P, Kurios M, Pantelis C. Neuropsychological function in young patients with unipolar major depression. Psychol Med 1997; 27: 1277-1285. [ Links ]
12. Fleming SF, Blasey Ch, Schatzberg AF. Neuropsychological correlates of psychotic features in major depressive disorders: A review and meta-analysis. Psychiat Res 2004; 38: 27-35. [ Links ]
13. Bryson GJ. Differential rate of neuropsychological dysfunction in psychiatric disorders: Comparison between the Halstead-Reitan and Luria-Nebraska batteries. Percept Mot Skills 1993; 76: 305-306. [ Links ]
14. Ballard C, Stephens S, Kenny RA, Tovee KM, O´Brien J. Profile of Neuropsychological Deficits in Older Stroke Survivors without Dementia. Dement Geriatr Cogn Disord 2003; 16: 52-56. [ Links ]
15. Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression. Possible implications for functional neuropathology. Brit J Psychiat 2001; 178: 200-206. [ Links ]
16. Oldenhinkel AJ, Berg MD, Bouhuys AL, Ormel J. Do depressive episodes leads to accumulation of vulnerability in the elderly? Depress Anxiety 2003;18: 67-75. [ Links ]
 Correspondence:
Correspondence:
Marek Preiss
Prague Psychiatric Center
Ustavni 91, Praha 8-Bohnice, 181 03, Czech Republic
Tel.: 420 266 003 338
Fax: 420 266 003 366
E-mail: preiss@pcp.lf3.cuni.cz
Received: 20 April 2009
Revised: 4 January 2010
Accepted: 9 February 2010