Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.28 no.4 Zaragoza oct./dic. 2014
https://dx.doi.org/10.4321/S0213-61632014000400002
Lower risk of prostate cancer in schizophrenia – Fact or artifact?
Gilad Gal, PhD*; Hanan Munitz MBBS, MRCPsych**; Itzhak Levav, MD, MSci***
* School of Behavioral Sciences, Tel Aviv-Yaffo Academic College. Israel.
** Clalit Health Services, Tel-Aviv. Israel.
*** Department of Community Mental Health, Faculty of Social Welfare and Health Sciences, Haifa University, Haifa. Israel.
The study was funded by The Israel National Institute for Health Policy and Health Services Research (r14-2010).
ABSTRACT
Background and Objectives: Reduced risk for prostate cancer in persons diagnosed with schizophrenia has been reported repeatedly. While genetic factors and antipsychotic medications were imputed, a methodological hypothesis could be raised: given the reported disparities of health services with regard to service users with schizophrenia these persons may be screened less often compared to schizophrenia-free counterparts resulting in undetected prostate tumors. The study objective was to compare the rates of performance of the prostate specific antigen (PSA) screening test among persons diagnosed with schizophrenia to matched-comparison subjects.
Methods: A prospective historical epidemiological study which included service users with and without a diagnosis of schizophrenia (N = 52,131). Linkage was conducted between databases of the nation-wide psychiatric register and Israel’s largest health maintenance organization. Annual performance of PSA tests was recorded between the years 2002-2009.
Results: Service users with schizophrenia performed the PSA test 23% less than the comparison subjects. However, among service users who were diagnosed with prostate cancer only 44% performed the PSA test during the year prior to diagnosis.
Conclusions: In line with our hypothesis, lower rates of PSA screening tests were conducted among service users with schizophrenia. However, the relatively low rate of this test prior to prostate cancer diagnosis ought to be noted.
Key words: Schizophrenia; Prostate; Cancer; Screening; Health Services; Epidemiology.
Introduction
Several studies found a reduced risk for cancer in persons diagnosed with schizophrenia1-7. Among cancer sites the most robust finding was associated with prostate cancer. Torrey8, who reviewed five large epidemiological studies with a total of 98,951 individuals with schizophrenia, noted a combined estimated standardized incidence ratio (SIR) of 0.59 (0.49 - 0.76) for prostate cancer. Importantly, most studies were based on nation-wide registries in countries with national health insurances (Denmark, England, Finland, and Israel). A subsequent review by Catts et al confirmed these findings, SIR 0.59 (0.48-0.73)2.
Torrey8 raised several substantive hypo-theses to explain these lower rates: 1. Genetic mechanisms; 2. Anti-tumor action of psycho-tropic medications; and 3. Limited heterosexual activity with a subsequent decreased risk of sexual-transmitted infections. However, a methodological hypothesis cannot be excluded: given the disparities in the health care of persons with schizophrenia9-11, if service-users with schizophrenia are less often screened with prostate-specific antigen (PSA) tests compared to schizophrenia-free men the identification of prostate cancer may fall.
We had the rare opportunity to explore the latter hypothesis in a study of medical services provided to persons with schizophrenia in a country with a national health insurance. In Israel, primary medical services are either entirely gratis (e.g., visits to general practitioners, laboratory tests, including PSA) for all legal residents and citizens, or a minimal co-payment is required to access a specialist.
In this study, we merged data from the National Psychiatric Case Registry (PCR), that records all psychiatric admissions and discharges since 1950, with the database of Israel's largest health maintenance organization (HMO) that provided information on the PSA tests performed, and compared their rates of performance among persons with the diagnosis of schizophrenia to matched comparison subjects.
Objective: To study the rate of PSA screening tests performed by service users with schizophrenia compared to matched compa-rison subjects in a country with a national health insurance, using a prospective historical design.
Methods
The study was based on a prospective historical design where data on the participants were collected between the years 2002-2009. The study was approved by the IRB of Clalit Health Services (CHS).
Identification of persons diagnosed with schizophrenia
We used the PCR to identify persons diagnosed with schizophrenia. The PCR is legally mandated to maintain a cumulative record of all psychiatric hospitalizations12-13. The PCR provided the subjects' diagnoses upon admission and discharge as well as socio-demographic information. Diagnoses are based on the ICD-10; those made prior to its introduction have been updated. A test of the agreement between research diagnoses and those recorded in the PCR found a satisfactory match14-15. The following inclusion criteria were applied: 1. Persons with last discharge diagnosis of schizophrenia (F20 - F29); and 2. Persons born before 1960 (age 40 and above at year 2000) and were alive by the year 2000.
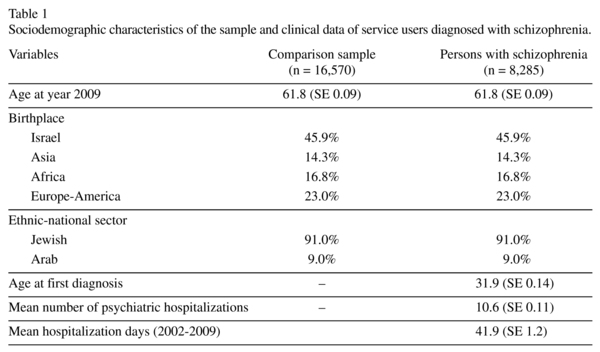
We identified 28,579 persons diagnosed with schizophrenia. Each one was identified based on his ID number. In addition to diagnoses, we gathered information on the year of first and last hospitalization, the number of hospitalizations, and the length of each hospital stay (Table 1). The latter was done annually between the years 2000-2009 to control for the possible artifact caused by periods when the person was not in the community.
General health services
Data from CHS, with 3.8 million insured persons, were collected from its electronic data base. The target population included subjects meeting the second inclusion criterion (above). A total of 1,040,000 subjects were identified. Information on the annual performance of PSA tests were gathered for the years 2002-2009, since CHS started to apply a central data base in 2002 only. In addition, medical diagnoses, including prostate cancer were recorded. Two measures were calculated based on the performance of PSA screening tests: a. sum of tests performed during the follow up period (2002-2009); b. since the performance of PSA tests is expected to rise in persons diagnosed with prostate cancer we have calculated an additional measure which accounts for the year of such diagnosis. The adjusted measure was based on the sum of tests performed during the follow up period before prostate cancer diagnosis was recorded. For example, if a person was diagnosed in 2006 the sum of PSA tests during the years 2002-2005 was calculated.
Linkage procedure and selection of a matched comparison group
The data extracted from the PCR and from the CHS databases were merged according to the personal ID numbers. The number of identified persons in both databases was 17,377.
To generate a matched comparison group (2:1 ratio) we defined an algorithm based on age (groups of three consecutive years), sex, birth place (Israel, Asia, Africa, Europe-America), socioeconomic status (high, mid, low), and ethnic-national sector (Jews and Arabs,). We omitted cases: 1. That had missing information on one of the matching variables; 2. That died before 2002; 3. That had an average yearly hospitalization period of 270 days or more. The matching procedure was tested and found satisfactory (Table 1). The data set included 17,377 service users with schizophrenia and 34,754 matched comparison subjects (n = 52,131).
Data analysis
The analysis was based on 8,285 men diagnosed with schizophrenia, and 16,570 matched comparison subjects. To account for the effects of matching, we applied the complex samples design of the SPSS 21.0 software (IBM Inc.) with case-control triads as cluster. Sum and adjusted sum of PSA tests were analyzed using general linear models (GLM), with the number of follow up years as a covariate. Rates of PSA tests (yes/no) and prostate cancer were analyzed using logistic regression models, reported in terms of odds ratios (OR) and 95% confidence intervals (95% CI).
Results
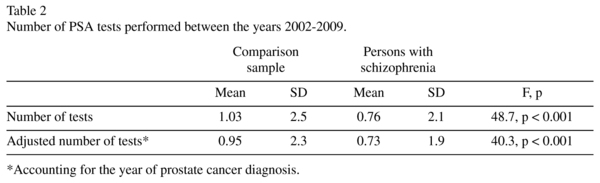
The PSA test was performed at least once during the follow up period (2002 - 9) among 26.2% of the service users with schizophrenia and 30.4% of their counterparts (OR = 0.83, 95% CI 0.78 - 0.88; p < 0.001). The performance of PSA tests during the follow up period was significantly lower among service-users with schizophrenia (mean 0.76) compared to their counterparts (mean 1.03) (F = 48.7, df = 1; 23,958, p < 0.001), reflec-ting a reduced performance of 26% (Table 2). Similar effects were observed when the length of stay of the psychiatric hospitalizations was controlled.
We identified a total of 523 service users diagnosed with prostate cancer. The rate of prostate cancer diagnosis was lower among service-users with schizophrenia (1.5%) compared to their matched counterparts (2.4%); odds ratio 0.61 (95% CI 0.50 - 0.75; p < 0.001). The adjusted PSA performance measure accounting for prostate cancer diagnosis was significantly lower among service-users with schizophrenia (mean 0.73) compared to their matched counterparts (mean 0.95) (F = 40.3, df = 1; 23,824, p < 0.001), reflecting a reduced performance of 23% (Table 2).
Among service users diagnosed with prostate cancer, 329 were diagnosed during the years 2003-2010. The PSA test during the year prior to cancer diagnosis (2002-9) was performed in 44% of these cases, with slight variation between those with schizophrenia (39.7%) and comparison subjects (46.4%) (p = 0.3).
Discussion
The current study compared the performance of PSA test in a large sample of adult service users with schizophrenia and matched comparison subjects. We found 23% (adjusted) decreased performance of PSA tests among service users diagnosed with schizophrenia compared to their matched counterparts. In line with previous reports1-8 we found that the risk of prostate cancer among service users with schizophrenia was lower than matched comparison subjects (in about 61%). According to our hypothesis, the lower rate of PSA tests could suggest that this negative association may reflect more an issue of method than an issue of substance. Since service-based disparities were noted repeatedly in the literature9-11, as well as in our data (Gal et al., submitted), it is possible that the lower rate of PSA tests among service users diagnosed with schizophrenia result in less biopsies, and the consequent lower rate of cancer diagnosis.
This interpretation should be carefully weighted given the relatively lower rate of performance of PSA test preceding the cancer diagnosis. According to our data, 44% of the persons with confirmed cancer diagnosis had a PSA test during the year previous to it, suggesting that for slightly more than half of the service users an alternative screening method (e.g., digital rectal examination (DRE)) was applied. This notion could be supported by the reservations raised regarding the PSA as a screening test16-18, which is recommended currently by some but not all professional organizations16,19.
The major limitation of this study is the reliance on the PSA test as the sole screening procedure for the identification of prostate cancer. Our findings would have been fully confirmed if we had data on the performance of DREs, and, especially biopsies, but such information was not available to us. Indeed, results of prostatic biopsies are considered a gold standard, but biopsies are ordered generally when the results of a PSA test or DRE are found positive. Note, however, that the lower performance of PSA screening tests among the service users with schizophrenia in our study would have resulted in an equally lower rate of biopsies. Among the US general population, 65% of the persons with high PSA levels are referred for biopsy20.
In conclusion, given the disparities prevailing in the health services provided to service users with schizophrenia, the lower rate of PSA tests might lead to lesser performance of biopsies which may be manifested in the underestimation of prostate cancer in this population group.
Acknowledgements
The data used in this report were made available by Inna Pugachova MPH, from the PCR, and Shachar Merling from CHS.
Conflict of interest
Co-author Hanan Munitz is employed by Clalit Health Services. All other authors declare that they have no conflicts of interest
References
1. Barak Y, Achiron A, Mandel M, Mirecki I, Aizenberg D. Reduced cancer incidence among patients with schizophrenia. Cancer. 2005; 104 (12): 2817-21. [ Links ]
2. Catts VS, Catts SV, O'Toole BI, Frost ADJ. Cancer incidence in patients with schizophrenia and their first-degree relatives: A meta-analysis. Acta Psychiatr Scand. 2008; 117 (5): 323-326. [ Links ]
3. Chou FH, Tsai KY, Su CY, Lee CC. The incidence and relative risk factors for developing cancer among patients with schizophrenia: A nine-year follow-up study. Schizophr Res. 2011; 129 (2-3): 97-103. [ Links ]
4. Cohen M, Dembling B, Schorling J. The association between schizophrenia and cancer: A population-based mortality study. Schizophr Res. 2002; 57 (2-3): 139-46. [ Links ]
5. Grinshpoon A, Barchana M, Ponizovsky A, Lipshitz I, Nahon D, Tal O, et al. Cancer in schizophrenia: Is the risk higher or lower? Schizophr Res. 2005; 73 (2-3): 333-41. [ Links ]
6. Levav I, Lipshitz I, Novikov I, Pugachova I, Kohn R, Barchana M, et al. Cancer risk among parents and siblings of patients with schizophrenia. Br J Psychiatry. 2007; 190: 156-61. [ Links ]
7. Lin CY, Lane HY, Chen TT, Wu YH, Wu CY, Wu VY. Inverse association between cancer risks and age in schizophrenic patients: A 12-year nationwide cohort study. Cancer Sci. 2013; 104 (3): 383-90. [ Links ]
8. Torrey EF. Prostate cancer and schizophrenia. Urology. 2006; 68 (6): 1280-3. [ Links ]
9. Björkenstam E, Ljung R, Burström B, Mittendorfer-Rutz E, Hallqvist J, Weitoft GR. Quality of medical care and excess mortality in psychiatric patients-a nationwide register-based study in Sweden. BMJ Open. 2012. [ Links ]
10. Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Med Care. 2002; 40 (2): 129-36. [ Links ]
11. Wu SI, Chen SC, Juang JJ, Fang CK, Liu SI, Sun FJ, et al. Diagnostic procedures, revascularization, and inpatient mortality after acute myocardial infarction in patients with schizophrenia and bipolar disorder. Psychosom Med. 2013; 75 (1): 52-9. [ Links ]
12. Lichtenberg P, Kaplan Z, Grinshpoon A, Feldman D, Nahon D. The goals and limitations of Israel's psychiatric case register. Psychiatr Serv. 1999; 50 (8):1043-8. [ Links ]
13. Mental Health in Israel, 2008. Department of Information and Evaluation Ministry of Health (2004). Mental Health in Israel. Statistical Annual. Jerusalem. http://www.old.health.gov.il/download/forms/mentalReport2008.pdf. Accessed August 25, 2013. [ Links ]
14. Rabinowitz J, Slyuzberg M, Ritsner M, Mark M, Popper M, Ginath Y. Changes in diagnosis in a 9-year national longitudinal sample. Compr Psychiatry. 1994; 35 (5): 361-5. [ Links ]
15. Weiser M, Kanyas K, Malaspina D, Harvey PD, Glick I, Goetz D, et al. Sensitivity of ICD-10 diagnosis of psychotic disorders in the Israeli National Hospitalization Registry compared with RDC diagnoses based on SADS-L. Compr Psychiatry. 2005; 46 (1): 38-42. [ Links ]
16. Barry MJ. Clinical practice. Prostate-specific-antigen testing for early diagnosis of prostate cancer. N Engl J Med. 2001; 344 (18): 1373-7. [ Links ]
17. Chou R, Croswell, JM, Dana T, Bougatsos C, Blazina I, Fu R, et al. Screening for prostate cancer: A review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2011; 155 (11): 762-71. [ Links ]
18. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or = 4.0 ng per milliliter. N Eng J Med. 2004; 350 (22): 2239-46. [ Links ]
19. Mandelson MT, Wagner EH, Thompson RS. PSA screening: A public health dilemma. Annu Rev Public Health. 1995; 16: 283-306. [ Links ]
20. Thompson IM, Ankerst DP, Chi C, Lucia MS, Goodman PJ, Crowley JJ, et al. Operating characteristics of prostate-specific antigen in men with an initial PSA level of 3.0 ng/ml or lower. JAMA. 2005; 294 (1): 66-70. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Gilad Gal
School of Behavioral Sciences
Tel Aviv-Yaffo Academic Collage
Rabenu Yeruham st
Tel Aviv. Israel
Tel.: 972-3-6802519
Fax: 972-3-6802526
E-mail: giladgal@mta.ac.il
Received: 31 August 2014
Revised: 2 October 2014
Accepted: 3 October 2014