Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Gaceta Sanitaria
versão impressa ISSN 0213-9111
Gac Sanit vol.30 no.5 Barcelona Set./Out. 2016
https://dx.doi.org/10.1016/j.gaceta.2016.01.005
The use of clinical practice guidelines in primary care: professional mindlines and control mechanisms
El uso de guías de práctica clínica en atención primaria: entre el conocimiento tácito y los mecanismos de control
Joan Gené-Badiaa,b, Pedro Galloc, Jordi Caïsc, Emília Sánchezd, Carme Carrione,f, Liliana Arroyoc and Marta Aymeriche,g
a Department of Public Health, University of Barcelona, Barcelona, Spain
b CAPSE - Catalan Institute of Health, Barcelona, Spain
c Department of Sociology and Organizational Analysis, University of Barcelona, Barcelona, Spain
d Blanquerna School of Health Science, Ramon Llull University, Barcelona, Spain
e TransLab Research Group, Department of Medical Sciences, School of Medicine, University of Girona, Girona, Spain
f Agency for Healthcare Quality and Assessment of Catalonia (AQuAS), Barcelona, Spain
g Health Sciences Department, Universitat Oberta de Catalunya, Barcelona, Spain
This research has been financially supported by the Instituto de Salud Carlos III, Spanish Ministry of Economy and Competitiveness, grant no. PI11-01902.
ABSTRACT
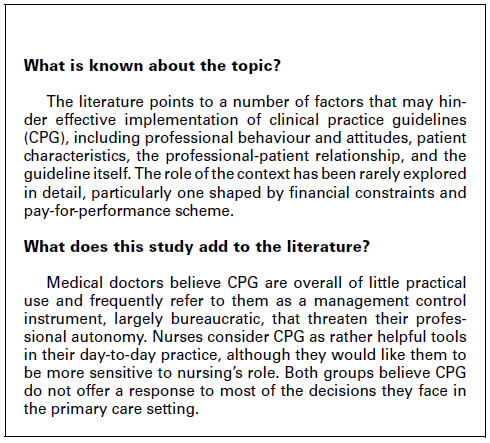
Objective: To identify the relevant barriers and enablers perceived by primary care professionals in implementing the recommendations of clinical practice guidelines (CPG).
Methods: Two focus groups were conducted with primary care physicians and nurses in Catalonia (Spain) between October and December 2012. Thirty-nine health professionals were selected based on their knowledge and daily use of CPG. Finally, eight general practitioners and eight nurses were included in the discussion groups. Participants were asked to share their views and beliefs on the accessibility of CPG, their knowledge and use of these documents, the content and format of CPG, dissemination strategy, training, professional-patient relationship, and the use of CPG by the management structure. We recorded and transcribed the content verbatim and analysed the data using qualitative analysis techniques.
Results: Physicians believed that, overall, CPG were of little practical use and frequently referred to them as a largely bureaucratic management control instrument that threatened their professional autonomy. In contrast, nurses believed that CPG were rather helpful tools in their day-to-day practice, although they would like them to be more sensitive to the current role of nurses. Both groups believed that CPG did not provide a response to most of the decisions they faced in the primary care setting.
Conclusions: Compliance with CPG recommendations would be improved if these documents were brief, non-compulsory, not cost-containment oriented, more based on nursing care models, sensitive to the specific needs of primary care patients, and integrated into the computer workstation.
Keywords: Primary health care. Qualitative research. Evidence-based medicine. Pay for performance.
RESUMEN
Objetivo: Identificar barreras y facilitadores percibidos por los profesionales de atención primaria en la aplicación de las recomendaciones de las guías de práctica clínica (GPC).
Método: Dos grupos focales con profesionales médicos y de enfermería (atención primaria) en Cataluña entre octubre y diciembre de 2012. Se seleccionaron 39 profesionales según su conocimiento y uso de las GPC. Finalmente se incluyeron ocho médicos/as de familia y ocho profesionales de enfermería. Se solicitó a los/las participantes compartir sus opiniones y creencias sobre accesibilidad, conocimiento y uso de las GPC, su contenido y formato, difusión, capacitación, relación profesional-paciente, y su utilización por parte de la estructura de gestión. Los contenidos fueron grabados, transcritos y analizados utilizando técnicas de análisis cualitativos.
Resultados: Los/las médicos/as creen que las GPC son en general de relativa utilidad práctica y con frecuencia se refieren a ellas como un instrumento de control burocrático que amenaza su autonomía profesional. Por el contrario, el grupo de enfermería consideró las GPC como herramientas bastante útiles en la práctica, aunque aún poco sensibles al papel actual de la enfermería. Ambos grupos creen que las GPC no ofrecen una respuesta a la mayor parte de las decisiones en el ámbito de la atención primaria.
Conclusiones: El cumplimiento de las GPC mejoraría con recomendaciones breves, no obligatorias, no orientadas a la contención de costes y sensibles a las necesidades específicas de los/las pacientes en atención primaria, integrándolas en la estación de trabajo clínica.
Palabras clave: Atención primaria. Investigación cualitativa. Medicina basada en la evidencia. Pago por resultados.
Introduction
Clinical practice guidelines (CPG) are defined as a set of recommendations based on scientific evidence and designed to assist both healthcare professionals and users in selecting the most suitable diagnostic and/or therapeutic options to address a specific clinical condition. Although the implementation of CPG has not been fully proven to improve health outcomes,1 health professionals generally accept that clinical care must be evidence-based and understand that CPG are among the best means available to translate scientific evidence into clinical practice.2,3 Despite the fact that family doctors believe in evidence-based practice, current health care assessments indicate variability in clinical decisions with a low level of adherence to CPG recommendations.4-6
Many factors have been identified that could influence CPG implementation. These factors could act as either a barrier or an enabler in areas such as professional behaviour and attitudes, patient characteristics, the professional-patient relationship, the organizational context, the guideline itself, and the wider environmental factors.1,6-10 A recent systematic review has revealed there are few rigorous studies that assess the effectiveness of a CPG implementation strategy, concluding that multifaceted interventions seem to be more effective than isolated ones.1
In Catalonia, Spain, CPG have been frequently used as a management tool for quality and efficiency improvement in primary care services. Despite the relative absence of published reports on their impact, CPG are extensively used as the bases for service contracts between the public regional purchaser of health services (CatSalut) and health care providers in the region. CatSalut lays out guidance for the management and prevention of the main chronic and acute conditions, for preventive care for the healthy population and for drug prescriptions. Primary care providers transfer the responsibility of achieving target objectives to family doctors and nurses through pay-for-performance schemes.11,12 There are economic incentives for general practitioners who prescribe drugs based on a very restrictive list. An accurate assessment of family practitioners' performance is conducted using a scoreboard of quality indicators. Data is extracted from audits of electronic registries and drug prescription practices.13-15 Originally, target objectives were related to quality of care indicators, but under pressure due to financial crises, a more cost-containment-based approach has been adopted.16,17 Indeed, drug prescription targets were formerly linked to adherence to a recommended list of drug products. However, today, primary care teams have a ceiling in their annual prescription budget. We have moved from a "soft management" type of care strategy to a rather "hard management" approach.18
To date, few studies have reported on barriers to and enablers of the use of CPG in Catalonia, and they are concerned largely with aspects that relate mainly to the CPG itself, such as adequate alignment with Health Plan for Catalan priorities, methodological rigor in their development, CPG accessibility, and user friendliness.19,20 There is thus a need to explore further the importance of these and other barriers and enablers in a context of considerable financial constraint, in which professionals remain under a pay-for-performance scheme. The Catalan context is suited to this purpose, and the hope is that the results of this research will provide tailored recommendations for policy measures and suitable management changes. In brief, this paper aims to identify relevant barriers to and enablers of CPG implementation as they are perceived by primary care doctors and nurses in Catalonia, Spain.
Methods
We carried out two discussion groups with sixteen medical doctors and nurses in the primary care field in Catalonia.21-23 The discussion groups were conducted in Barcelona in October 2012 and in November 2012. Thirty-nine professionals were selected based on their knowledge and use of CPG on a daily bases. It is worth pointing out that we aimed at regular nursing and medical staff, with no particular specialised training on CPG, coming from both rural and urban areas, and randomly selected from a primary care staff database owned by the IDIAP Jordi Gol Institute (a reference public institute devoted to research in primary care in Spain). Potential participants received a formal letter of invitation from the project leader explaining the purpose and methods of the study. Participation was confirmed by e-mail and telephone calls. Finally, eight family doctors and eight nurses accepted participation and were included in the discussion groups. All participants signed a written informed consent letter to take part in the study.
This study was financed by the Spanish Ministry of Science and Innovation and no ethical approval was necessary since it does not involve any human experimentation or the use of biological samples of human origin.
Information gathered from a previous systematic literature review on barriers to and enablers of the use of CPG was used to help draft a semi-structured interview protocol, which was used in both discussion groups.24 The interview protocols consisted of a series of open-ended questions. Participants were asked to discuss their views, perceptions and beliefs on a number of key dimensions in the use of CPG in their daily practice. These dimensions include accessibility of knowledge and use of CPG, content and format of the guidelines, guideline dissemination strategy, the importance of training, the professional-patient relationship, and the use of CPG by the management structure in the organization. The ultimate aim was to gather and process key informants views on barriers and facilitators for CPG in their context.
A highly experienced focus group manager in the health care area conducted the two discussion sessions assisted by two observers who took field notes. The manager piloted the sessions, ensuring that all relevant topics were covered. No group interviews lasted more than two hours, including coffee breaks.
All the information retrieved was audio and video recorded and then transcribed verbatim in full. Participants validated the final versions of transcripts before the analysis was performed. For the analysis, qualitative data were managed and processed using Atlas.ti 7.0. Content analysis was done by one coder with a double-check codification. The starting point was a code list based on the abovementioned literature review, which contained 164 codes organized into six categories and nineteen families.24 Thirty-six additional new codes were created based on data processing, following the grounded theory approach.
Results
Table 1 summarizes the most frequent views on relevant dimensions of CPG as expressed by family doctors and nurses in the discussion groups. These views refer to the available CPG, that is, those that are used in their day-to-day practice. In short, medical doctors believe that CPG are, overall, of moderate practical use and commonly refer to them as a control instrument from the management structure that poses a threat to their autonomy, as well as a bureaucratic burden on their professional practice. However, nurses consider CPG as more helpful tools in their day-to-day practice. Both groups agree that CPG must count on professional leaders in their dissemination and should be readily available in their workstation. Nurses value the integration of CPG into clinical records, displaying reminders with the list of procedures to be performed and box-checked. Family doctors prefer easy access to the full content of CPG, using them as a support mechanism in their clinical decision-making. Both groups agree that CPG cover only a minimal part of the clinical decisions to be made in real practice. Nurses feel that CPG give insufficient coverage to nursing care diagnosis and procedures, while family doctors complain that CPG do not respond to the specific characteristics of their more complex patients. The scientific basis of the available CPG was not under debate, although doctors criticise their emphasis on cost containment. Nurses believe CPG overall benefit the patient's health, but family doctors, somewhat more critical, criticise the lack of assessment mechanisms and tend to rely on professional consensus as a means for decision-making under certain circumstances. Finally, both groups find necessary to assess the impact of CPG in their context.
Table 1. Nurses' and family doctors' views on relevant dimensions of clinical practice guidelines. 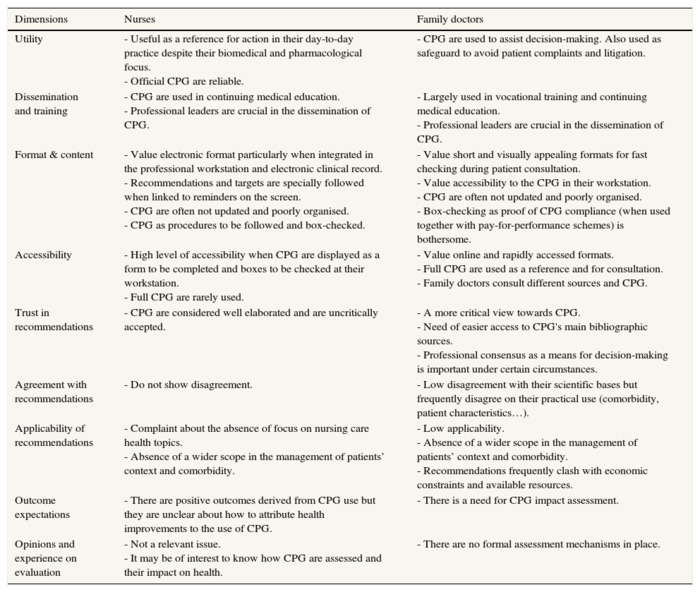
CPG: clinical practice guidelines.
When asked about the importance of the organisational context as barrier or enabler to CPG implementation (Table 2), family doctors fear that objectives to be achieved in the pay-for-performance scheme may interfere with their patients' demands and care needs. The electronic professional workstation is highlighted as very useful for registry purposes (some improvements are suggested), but it is also seen as a control mechanism. Box-checking in the electronic clinical record is found to be of little value, bureaucratic, and imposed by the upper management structure. Nurses claim there is a strong organisational inertia that could act as an obstacle for CPG use and suggest that professional leaders should take an active role in dissemination for CPG be more sensitive to their day-to-day practice.
Table 2. The importance of the context as barrier or enabler to clinical practice guidelines
implementation as perceived by nurses and family doctors. 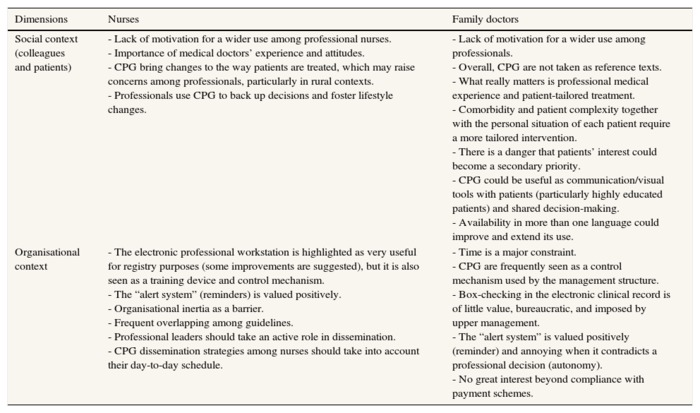
CPG: clinical practice guidelines.
When asked more explicitly to identify barriers and enablers to CPG implementation (Table 3), we find it is frequent the case that a particular barrier, when overcome, act as a facilitator, and vice versa. For example, professionals feel that specific CPG characteristics, professional motivation, dissemination strategies could act both as enablers and barriers to their implementation. From nurses and doctors' responses. Family doctors and nurses recognize that electronic reminders facilitate implementation but state that they simultaneously constrain medical autonomy and impede patient-tailored decisions. According to views expressed by both groups of professionals, neither the pay-for-performance scheme nor the CPG themselves allow for much room for patient participation.
Table 3. Barriers and enablers to clinical practice guideline implementation according to nurses and family doctors. 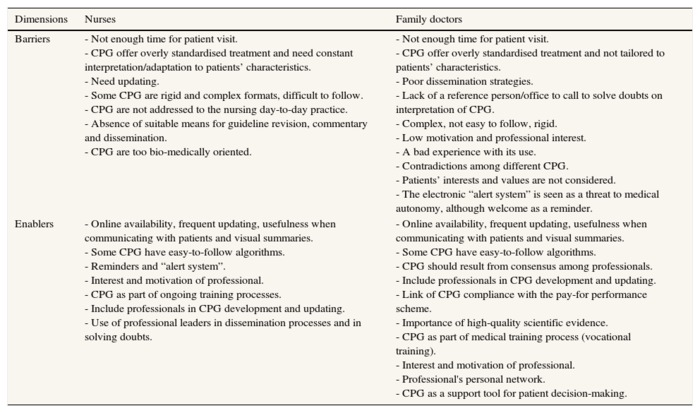
CPG: clinical practice guidelines.
We finally asked participants to convey which elements could define a valuable CPG. Table 4 shows the main results in this respect. Overall, participants argue that for CPG to be an asset they must be brief, available at their clinical workstation, comprehensive and far-reaching, as well as sensitive to specific patient needs, among other characteristics. Professional participation and updating and a better inter-connection among CPG when various pathologies coincide were also claimed as relevant aspects for future CPG. Family doctors insist in the need to conceive CPG as a helping hand, not as a control mechanism.
Table 4. What constitutes a valuable CPG according to nurses and family doctors. 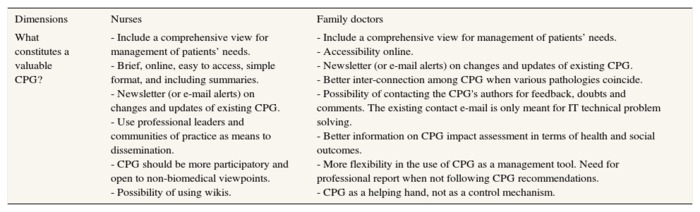
CPG: clinical practice guidelines;
IT: information technologies.
Discussion
Our study has conveyed the main results of physicians and nurses' views on the use of CPG in primary care in Catalonia. Both groups of professionals largely see CPG as part of the incentive scheme (i.e., pay-for-performance) laid out by the management structure, using a comprehensive information system, and being continuously monitored in this respect. Indeed, compliance with CPG is used as a key indicator of professionals' performance in many health care organisations in Catalonia, which apparently turns it into a control mechanism to monitor their professional activities. This may help to explain professionals' claims in favour of improved participation in the design and implementation of CPG, which would also allow for such CPG to be better adapted to the particularities of a primary care setting.
CPG, particularly when integrated into the electronic clinical record, seem to be better accepted by nurses than by family doctors. Their different professional backgrounds could help in explaining this. Despite nurses claiming that CPG are overly bio-medically orientated, they tend to be more comfortable with the idea of complying with computer-assisted instructions. This attitude might be related to a traditional professional identity linked to obedience and compliance with hierarchy. It is worth noting in this regard that box-ticking in front of a computer does not support the nursing profession's progression towards the attainment of a modern, more autonomous professional role based on new conceptual models and nursing theories25. Physicians, on the contrary, perceive CPG as an obstacle and as an additional burden on the management of patients' needs and demands.10 Informal interaction among primary care team members creates an effective knowledge of practice.26 Family doctors feel comfortable when behaving according to these procedures informally agreed with their primary care team. Therefore, here CPG are seen as tools for bureaucratic control rather than as a helping hand in incorporating scientific evidence into the medical practice. The literature points to physicians relying on some form of "mindlines",26 that is, on collectively reinforced, internalised, tacit guidelines in their decision-making process. These mindlines are informed by reading briefs, by their own professional experiences, by their interaction with other colleagues and opinion leaders, with patients and pharmaceutical representatives, and by accessing other sources of tacit knowledge.
Primary care works rather like a black box in which medical doctors and nurses need to have a mix of medical, caring and personal management skills to properly address an individual patient's needs, often beyond mere medical treatment. Managers, however, need to control the process of delivering care to ensure evidence-based procedures are implemented, and they do this by monitoring a given set of indicators linked to each professional's performance. The extent to which available CPG, instead of addressing real patients' needs, become an obstacle to effective patient management is still to be determined.27
Moreover, CPG could be perceived by rather indulgent physicians as an obstacle to satisfying a patient's demands. Addressing such demands may improve patients' satisfaction, albeit that, as evidence shows, it could also lead to overtreatment. In this respect, an American study showed that a higher level of patient satisfaction was associated with less emergency department use but also with greater inpatient use, higher overall health care and prescription drug expenditures, and increased mortality.28
When making clinical decisions, Catalan doctors feel less autonomous than their Swedish colleagues. The Nordic context may be more respectful of physicians' criteria and their managed care practice might be of a softer type. Yet, doctors in both contexts agree to be playing on the safer side when following CPG.29 Despite the efforts to develop CPG oriented towards comorbidity in patient care,30 these guidelines are mostly concerned with an individual disease, clinical condition, or risk factor. In addition, the evidence used by CPG is frequently generated in contexts different from the ones to which they are later applied. Furthermore, clinical trials are mostly performed in hospital settings on patients with a specific age range and low degree of comorbidity. It is thus reasonable to concur with professionals' complaint about the non-applicability of CPG in certain primary care patients.31,32
Furthermore, family doctors feel more pressured when compliance with CPG is linked to pay-for-performance schemes. Catalan family doctors, unlike their British colleagues, do not have the option of reasonably excluding individual patients from their professional performance evaluation,33 which may raise doubts about what comes first, meeting targets or responding to a patient's needs. Pay-for-performance schemes could actively change professionals' behaviour.34 When improvements to particular indicators are linked to financial incentives, these may be at the expense of other aspects of care that were not promoted, which suffer detrimental effects.35 Little is known about their impact on the response to patients' demands for care and on patients' health.
Family doctors and nurses are far from critical of the scientific basis of CPG. Nonetheless, they do not use CPG as their only support tool in clinical practice, rather as reliable sources of information to validate their already existing "midlines" and decision shortcuts used in patient care.26 Despite the prevalent discourse in favour of evidence-based medicine, Catalan doctors, as well as their British and Swedish counterparts, accept CPG more positively if they are disseminated and introduced by their colleagues and professional leaders with special interest in the topic.26,29 Professional consensus, extensively criticised by the evidence-based medicine movement, is fully accepted by practising physicians. This may explain why pharmaceutical companies continue financing and promoting expert consensus meetings, even on topics with more than enough empirical evidence available. As is the case in other contexts, Catalan family doctors fear the cost-containment bias of the official CPG more than the potential conflicts of interests among their clinical leaders.29
Our results show family doctors demanding an assessment of the impact of this pay-for-performance scheme on patients' health, but not nurses. Indeed, currently, the Catalan health system places more effort in evaluating professional adherence to top-down objectives than in assessing whether the proposed policy scheme is effectively improving patients' health. It therefore becomes necessary to assess whether management strategies that use CPG are really contributing to better patient management-and ultimately to better health-or if such strategies (management through objectives, payment scheme based on performance) are just box-checking exercises that consume huge amounts of health resources and reduce the health system's responsiveness to real patient demands. Current schemes must prove they have a positive effect on a patient's health, which would in turn lower existing professionals concerns.
Both groups of professionals claim that CPG do not give sufficient consideration to patient preferences. However, in Catalonia this apparent weakness might not have a high impact on CPG implementation. In practical terms, patient involvement in health decisions in Catalonia remains largely a matter of discourse, rather than practice. Spain is the European country with the highest degree of clinical paternalism and with the highest percentage of citizens believing "my doctor knows best", and thus not willing to be involved in clinical decisions.36
In general terms, electronic clinical record reminders on the use of CPG are well accepted by both family doctors and nurses, although empirical evidence shows that family doctors typically respond to roughly half of the total number of clinical decision support prompts they receive.37 Family doctors, unlike nurses, tend to skip reminders when they contradict personal clinical criteria and "mindlines". Both types of professionals accept personal computer workstations as a central component of their professional practice and use them for patient interaction. Workstations are not seen as the problem but are frequently referred to as a management control tool.
When asked, participants believe an ideal guideline should be brief, integrated into the electronic clinical record, targeted to the specific patient's needs, adaptable to patient preferences, disseminated by clinical leaders with special interest in the topic, built by credible and accessible sources, flexible and not compulsory in its implementation. In this respect, there is vast room for improvement when it comes to already existing CPG.
Conclusions
Modern primary health care should be evidence-based and tackle patients' health needs rather than respond exclusively to patients' demands. CPG seem to be the best available tool to this end. However, when CPG are viewed as management tools, they may enter into conflict with primary care decision-making processes and with existing professional "mindlines". To allow evidence-based medicine and CPG to be incorporated into clinical practice, it is imperative to ease the management pressure on professionals and to improve local leaders' participation in their design.
Family doctors and nurses' compliance with CPG recommendations would improve if guidelines were brief, not compulsory, not aimed at cost containment, more based on nursing care models, sensitive to specific patients' needs in primary care, and integrated into the computer workstation. Clinical local leaders should play a more active role in CPG's dissemination and implementation. The generation of adequate and contextualised evidence in primary care settings should also be encouraged. This will allow for more appropriate CPG and, when needed, facilitate the inclusion of patients' viewpoints. Following these strategies will alleviate the bureaucratic pressure perceived by doctors, increase compliance by both doctors and nurses with CPG and better address patients' needs.
Editor in charge
Carme Borrell.
Transparency declaration
The corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributions
All authors have explicitly accepted the content of the manuscript in its latest version. All authors participated in a relevant manner in the design and development of the study in its different phases. J. Gené-Badia, P. Gallo, J. Caïs, E. Sánchez, C. Carrion and M. Aymerich contributed to the conception and design of the study; J. Gené-Badia, C. Carrion and L. Arroyo to data acquisition; J. Gené-Badia, P. Gallo, J. Caïs, E. Sánchez, C. Carrion, L. Arroyo and M. Aymerich to the analysis and interpretation of data; J. Gené-Badia, P. Gallo and J. Caïs wrote the draft article; E. Sánchez, C. Carrion, L. Arroyo and M. Aymerich contributed substantially to the critical review of its intellectual content.
Conflicts of interest
None.
Acknowledgements
We would like to thank the professionals who participated in the focus groups and the University Institute in Primary Care Research Jordi Gol (IDIAP Jordi Gol) for their help in conducting them.
References
1. Brusamento S, Legido-Quigley H, Panteli D, et al. Assessing the effectiveness of strategies to implement clinical guidelines for the management of chronic diseases at primary care level in EU Member States: a systematic review. Health Policy. 2012;107:168-83. [ Links ]
2. Institute of Medicine. Clinical practice guidelines we can trust. Washington DC: The National Academies Press; 2011. p. 290. [ Links ]
3. Hayward RS, Guyatt GH, Moore KA, et al. Canadian physicians' attitudes about and preferences regarding clinical practice guidelines. CMAJ. 1997;156:1715-23. [ Links ]
4. Llor C, Cots JM, Hernández S, et al. Effectiveness of two types of intervention on antibiotic prescribing in respiratory tract infections in primary care in Spain. Happy Audit Study. Aten Primaria. 2014;46:492-500. [ Links ]
5. Gómez Marcos MA, Rodríguez Sánchez E, Ramos Delgado E, et al. Durability of the effects of a quality improvement intervention in hypertensive patients on long-term follow-up (CICLO-RISK study). Aten Primaria. 2009;41:371-8. [ Links ]
6. Hormigo Pozo A, Viciana López MA, Gómez Jiménez L, et al. Improved effectiveness in the management of cardiovascular risk among type 2 diabetic patients in primary health care. Aten Primaria. 2009;41:240-5. [ Links ]
7. Francke AL, Smit MC, de Veer AJE, et al. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Medical Informatics and Decision Making. 2008;8:38. [ Links ]
8. Midlöv P, Ekesbo R, Johansson L, et al. Barriers to adherence to hypertension guidelines among GPs in southern Sweden: a survey. Scand J Prim Health Care. 2008;26:154-9. [ Links ]
9. Johnston KN, Young M, Grimmer-Somers KA, et al. Why are some evidence-based care recommendations in chronic obstructive pulmonary disease better implemented than others? Perspectives of medical practitioners. Int J Chron Obstruct Pulmon Dis. 2011;6:659-67. [ Links ]
10. Strain WD, Cos X, Hirst M, et al. Time to do more: addressing clinical inertia in the management of type 2 diabetes mellitus. Diabetes Res Clin Pract. 2014;105:302-12. [ Links ]
11. Gené-Badia J, Escaramis-Babiano G, Sans-Corrales M, et al. Impact of economic incentives on quality of professional life and on end-user satisfaction in primary care. Health Policy. 2007;80:2-10. [ Links ]
12. Gené Badia J, Gallo de Puelles P. Variable payment linked to quality of care. Aten Primaria. 2004;15:198-201. [ Links ]
13. Catalán A, Borrell F, Pons A, et al. Patient safety in primary care: PREFASEG project. Med Clin (Barc). 2014;143(Suppl 1):32-5. [ Links ]
14. Lizano-Díez I, Modamio P, López-Calahorra P, et al. Evaluation of electronic prescription implementation in polymedicated users of Catalonia, Spain: a population-based longitudinal study. BMJ Open. 2014;5:e006177. [ Links ]
15. Gené Badia J. Basta de clicar casillas. Aten Primaria. 2007;39:169-70. [ Links ]
16. Gallo P, Gené-Badia J. Cuts drive health system reforms in Spain. Health Policy. 2013;113:1-7. [ Links ]
17. Gené-Badia J, Gallo P, Hernández-Quevedo C, et al. Spanish health care cuts: penny wise and pound foolish. Health Policy. 2012;106:23-8. [ Links ]
18. Borrell F, Carballo F, Gadea I, et al. Ética de los incentivos a profesionales sanitarios. Madrid: Fundación de Ciencias de la Salud; 2009. p. 132. [ Links ]
19. Solà I, Carrasco JM, Díaz del Campo P, et al. Attitudes and perceptions about clinical guidelines: a qualitative study with Spanish physicians. PLoS One. 2014;5:e86065. [ Links ]
20. Kotzeva A, Guillamón I, Gracia J, et al. Use of clinical practice guidelines and factors related to their uptake: a survey of health professionals in Spain. J Eval Clin Pract. 2014;20:216-24. [ Links ]
21. Morgan DL, Krueger RA, editores. The focus group kit., Thousand Oaks, CA: Sage Publications; 1997. p. 692. [ Links ]
22. Green J, Thorogood N, editors. Qualitative methods for health research, 2nd ed. London: Sage Publications; 2009. p. 320. [ Links ]
23. Pope C, Mays N, editors. Qualitative research in health care. London: BMJ books; 2000. p. 168. [ Links ]
24. Carrion C, Gallo P, Sánchez E, et al. Barriers and facilitators to research translation into health care decision making: reviewing the evidence. Evidence Live, 25-26 March 2013. England: Oxford; 2013. [ Links ]
25. Miró Bonet M. Conceptual models; a power strategy with professional implications. Enferm Clin. 2010;20:360-5. [ Links ]
26. Gabbay J, le May A. Evidence based guidelines or collectively constructed mindlines? Ethnographic study of knowledge management in primary care. BMJ. 2004;329:1013. [ Links ]
27. Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta-synthesis of GPs' attitudes to clinical practice guidelines. Br J Gen Pract. 2007;57:971-8. [ Links ]
28. Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405-11. [ Links ]
29. Milos V, Westerlund T, Midlöv P, et al. Swedish general practitioners attitudes towards treatment guidelines: a qualitative study. BMC Fam Pract. 2014;15:199. [ Links ]
30. Bernabeu-Wittel M, Alonso-Coello P, Rico-Blázquez M, et al. Development of clinical practice guidelines for patients with comorbidity and multiple diseases. Aten Primaria. 2014;14:328-35. [ Links ]
31. Freeman AC, Sweeney K. Why general practitioners do not implement evidence: qualitative study. BMJ. 2001;323, 1100-2A. [ Links ]
32. Heselmans A, Donceel P, Aertgeerts B, et al. The attitude of Belgian social insurance physicians towards evidence-based practice and clinical practice guidelines. BMC Fam Pract. 2009;10:64. [ Links ]
33. Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355:375-84. [ Links ]
34. Doran T, Kontopantelis E, Valderas JM, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK quality and outcomes framework. BMJ. 2011;342:d3590. [ Links ]
35. Van Herck P, De Smedt D, Annemans L, et al. Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv Res. 2010;10:247. [ Links ]
36. Coulter A, Crispin J. European patients' views on the responsiveness of health systems & health providers. Eur J Publ Health. 2005;15:355-60. [ Links ]
37. Hendrix KS, Downs SM, Carroll AE. Pediatricians' responses to printed clinical reminders: does highlighting prompts improve responsiveness. Acad Pediatr. 2015;15:58-164. [ Links ]
![]() Correspondence:
Correspondence:
Pedro Gallo
pgallodep@ub.edu
Received 20 November 2015
Accepted 14 January 2016














