Quality of life (QoL) is the perception that a person has of his or her life based on his or her context, culture, and value system in relation to his or her goals, standards, concerns, and expectations (WHOQOL Group, 1993), and is generally studied to identify factors that improve or deteriorate it. Mindfulness is considered a temporary state, in which conscious attention is paid to the present experience without judgment (Kabat-Zinn, 1990), or a personality trait that involves the ability to maintain attention in the present with an open and non-judgmental attitude (Brown & Ryan, 2003). Mindfulness, introduced to psychology by Jon Kabat-Zinn in 1979 through the Mindfulness-Based Stress Reduction Program (MBSR, Kabat-Zinn, 2003), may have positive effects on various dimensions of QoL, as it has been shown to have benefits at the bio-psycho-social level (Garcia & Demarzo, 2018).
Systematic reviews (SR) and meta-analyses (MA) have explored the relationship between QoL and mindfulness, but most have focused on clinical populations (Cavalcante et al., 2022; Chen et al., 2021; Goyal et al., 2014; Han, 2021a; Hearn & Cross, 2020; Li et al., 2022; Newland & Bettemcourt, 2020; Nnate et al., 2021; Zhang et al., 2019a; Zhang et al., 2019b). Other MAs sought to assess the relationship in family caregivers of people with dementia (Han, 2021b), and in an Iranian population (Aghaie et al., 2018). Still others evaluated the relationship as part of one of their axes, however, Stynes et al. (2022) only considered three studies with clinical population, Taylor et al. (2021) included QoL and well-being as one and the same category, and Khoury et al. (2015) evaluated the efficacy of MBSR in non-clinical populations, only measuring anxiety and stress.
All the previous SRs and MAs have a common purpose, to evaluate the effectiveness of different Mindfulness-Based Interventions (MBIs), mainly in clinical populations, referring to the state induced through practice; however, to date no SRs have been found that consider the relationship between QoL and trait mindfulness (TM).
Low QoL in non-clinical population has been related to problems with physical and psychological health, education, social relationships, and even suicide risk (Hidalgo-Rasmussen, 2015; Hidalgo-Rasmussen et al., 2019). On the other hand, mindfulness has been associated with bio-psycho-social benefits (Garcia & Demarzo, 2018). Given that the study of TM is important, understanding more about the relationship between QoL and TM in non-clinical adult population could provide relevant information for improving QoL, as well as for future studies to consider it. Therefore, the aim of this review is to synthesize the evidence related to the interaction of QoL with TM in non-clinical adult populations.
Method
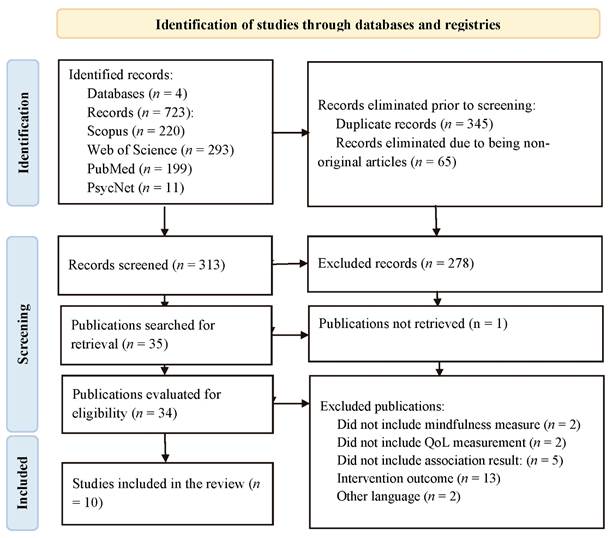
The review was carried out following the criteria established by the PRISMA methodology for systematic reviews (Page et al., 2021).
Study Selection Criteria
Inclusion criteria: a) primary outcomes measuring the association between QoL and TM in adults aged 18 to 65 years; b) quantitative articles; c) articles published between 1979 and 2022; d) articles in English and Spanish; e) articles with access to the full text.
Exclusion criteria: a) review articles, psychometric properties, or protocols; b) articles that do not use psychometric instruments to measure both QoL and TM; c) qualitative articles; d) articles that require participants to have a physical or mental health condition, or be patients in an institution; e) association results following an MBI.
Search Procedures
Searches were conducted during March 2023, in the following databases: Scopus, Web of Science, PubMed, and PsycNet, considering journal articles published between 1979 and 2023, by title, abstract, and keywords in Scopus and Web of Science, by title and abstract in PubMed, and by first page in PsycNet, in Spanish and English, with the following terms and Boolean operators:
(("quality of life" OR QOL OR "calidad de vida" OR “health-related quality of life” OR “calidad de vida relacionada con la salud” OR HRQOL OR CVRS) AND (mindfulness OR "atención plena" OR "conciencia plena") NOT (disease* OR enfermedad* OR cancer OR cáncer OR HIV OR VIH OR "multiple sclerosis" OR “esclerosis múltiple” OR patient* OR paciente* OR menopaus* OR dementia OR demencia OR disorder* OR trastorno* OR "clinical population*" OR “población clínica” OR disabilit* OR discapacidad* OR obesity OR obesidad OR diabet* OR fibrom* OR pain OR dolor OR pregnan* OR embaraz* OR incontinenc* OR infertili* OR adolescen* OR "older adult*" OR “adultos mayores” OR child* OR niñ*)).
A prior review was conducted following the Peer Review of Electronic Search Strategies guide (PRESS; McGowan et al., 2016).
Coding of Variables
All retrieved articles were imported into the Endnote manager and duplicates were removed. Through the Rayyan software, two reviewers read the titles and abstracts and discussed inconsistencies. Subsequently, the full texts were examined and checked for compliance with the criteria and relevant data were extracted in Excel.
Risk of Bias Assessment of Studies
A Risk of Bias Assessment (RBA) of the studies was performed by both reviewers. The Hawker et al. (2002) methodological rigor scoring tool was used, which addresses nine domains: a) title and abstract; b) introduction and objectives; c) method and data; d) sampling; e) data analysis; f) ethics and bias; g) results; h) transfer or generalization; i) implications and usefulness; with a Likert scale ranging from "good" to "very poor".
Results
Selection of Studies
A total of 723 records were found. After eliminating duplicates and non-original articles, 313 remained, of which 278 did not meet the eligibility criteria and one could not be retrieved in full text. Thus, 34 documents were reviewed, of which 10 articles were included. Figure 1 shows the flow chart of the selection process.
Characteristics of the Studies
Table 1 shows the characteristics of the included studies, which were generated in the last five years, with Iran being the country with the most studies, followed by Spain.
Table 1. Characteristics of the Studies
| Author and year | Country | Sample | Population/Age | Design/Intervention | Quality of life instrument | Mindfulness instrument | Effect size | Mediating/moderating variables |
|---|---|---|---|---|---|---|---|---|
| Azad et al., 2018 | Iran | 315 | Male soldiers serving in military facilities/ (18-33 years; M = 23.85, SD = 2.94) | Transversal/No | WHOQOL-BREF: overall score | MAAS |
Differences between QoL and low (LM), moderate and high (HM) levels of mindfulness. F = 43.58, n2 = .21, p = .001. Correlations QoL and LM: r = .43, p < .01; QoL and HM: r = .30, p < .05. |
No/No |
| Calvete et al., 2021 | Spain | 78 | Caregivers of persons with acquired brain injury (22 to 80 years; M = 57.42, SD = 12.2) | Transversal/No | WHOQOL-BREF: global score | MAAS | r = .52, p < .001 | Rumination/No |
| Cheung et al., 2020 | China | 905 | Vocational high school students in an impoverished county (18 years) | Transversal/No | PedsQL | Mindful Attention Awareness Scale for Adolescents (MAAS-A) |
r = .45, p < .001; β = 0.41, p < .001 |
Resilience/No |
| Fernandes et al., 2019 | Brazil | 26 | Health professionals in primary care (18 years of age or older; M = 37.9, SD = 12.5) | Quasiexperimental/Yes | The COOP Function questionnaire | FFMQ |
QoL and Mindfulness dimensions Describe positive: r = -.52, p = .01; All other dimensions: p > .05. |
No/No |
| Im et al., 2020 | United States of America | 157 | College students (18-48 years old; M = 22.60, SD = 4.84) | Transversal/No | WHOQOL-BREF: global score | FFMQ |
QoL and Mindfulness dimensions Note: p > .05; Describe: r = .41, p < .001; Acting attentively: r = .47, p < .001; Non-reactivity: r = .33, p < .001; Non-judgmental: r = .40, p < .001 |
No/No |
| My-Quyen et al., 2020 | Vietnam | 283 | Yoga training service clients (18-45 years) | Transversal/No | WHOQOL-BREF: Physical Health, Psychological Health and Social Relationships. Global item | 4 items based on Brown and Ryan (2003) | β = .66, p = .003 | Client's cocreation effort/No |
| Ruiz-Fernández et al., 2020 | Spain | 506 | Attending physicians and nurses in COVID-19 (M = 46.7, SD = 10.2) | Transversal/No | ProQoL: Compassion Fatigue, Burnout and Compassion Satisfaction | One dimension of the Self-Compassion Scale |
Mindfulness and QoL dimensions Compassion satisfaction: r = .32, p < .01; Burnout: r = -.39, p < .01; Compassion fatigue: r = -.40, p < .01 |
No/No |
| Světlák et al., 2021 | Czech Republic | 227 | Undergraduate students of the School of Medicine (M = 22.3, SD = 2.1) | Not defined/Yes | The Subjective Quality of Life Analysis (SQUALA) | FFMQ |
QoL dimensions and mindfulness dimensions QoL SatisfactionObserve: r = -.08, p = < .05; Describe: r = -.09, p = < .05; All other dimensions: p > .05. Importance of QoL Observe: r = -.08, p = < 0.05; Describe: r = -.17, p = < .001; Act attentively: r = -.24, p = < .001; Non-reactivity: r = -.33, p = < .001; No judgments: r = -.22, p = < .001 |
No/No |
| Valikhani et al., 2020 | Iran | 315 | Soldiers serving in military facilities (18 -33 years; M = 23.85, SD = 2.94) | Transversal/No | WHOQOL-BREF: overall score | MAAS | r = .60, p = .001 | Perceived stress/No |
| Yaghoubian & Babakhani, 2019 | Iran | 148 | Middle-aged women (40-65 years old; M = 47.8, SD = 6.2) | Transversal/No | Health Survey (SF-36) | MAAS |
Mindfulness and QoL r = .38, p = .001; R2 = .22, p = .001. Mindfulness and QoL dimensions Physical Functioning r = .22, p = .001; Physical Role r = .27, p = .001; Body Pain r = .19, p = .01; General Health r = .17, p = .01; Vitality r = .29, p = .001; Social Functioning r = .41, p = .001; Emotional Role r = .32, p = .001; Mental Health r = .24, p = .001 |
No/No |
Four studies did not define QoL (Azad et al., 2018; Calvete et al., 2021; Fernandes et al., 2019; Valikhani et al., 2020), two agreed on the WHOQOL Group (1993) definition, one was based on Hijmans et al. (2010), Karasimopoulou et al. (2012), and Utsey et al. (2002), another was based on Roney and Acri (2018) and Stamm (2005), another on Zannotti and Pringuey (1992), and one on Ayranci et al., (2010). Half of the studies measured QoL with the WHOQOL-Bref questionnaire, four of them by global score and the remaining one with three dimensions; as for instruments aimed at specific populations, one used an instrument for the occupational area (Professional Quality of Life Scale [ProQoL]) and another used one for children and adolescents (Pediatric Quality of Life Inventory [PedsQL]).
Eight of the ten studies considered mindfulness as a trait, as the other two aimed to evaluate an intervention; among these eight studies, two did not include the definition (Cheung et al., 2020; Ruiz-Fernández et al., 2020), three were based on Baer (2003), one on Kabat-Zinn (2003), another on Brown and Ryan (2003) and on Nezlek et al. (2016), and another was based on Desbordes et al. (2014). Most measured mindfulness through the Mindful Attention Awareness Scale (MAAS), followed by the Five Facet Mindfulness Questionnaire (FFMQ), and even a dimension of the Self-Compassion-Scale and a four-item scale were used.
The population was varied, with two studies evaluating university students, another two Iranian soldiers, and two more health professionals; the remaining four included caregivers, high school students, yoga clients, and middle-aged women. Most were young adults. Upon completion, ages ranged from 18 to 80 years, due to the study by Calvete et al. (2021), which included people aged 22 to 80 years, with a mean age of 57. Most designs were cross-sectional, with the exception of the two interventions, one of these was classified as quasi-experimental (Fernandes et al., 2019), while the other did not define the design (Světlák et al., 2021).
All studies that associated QoL and TM as global scores obtained significant relationships with moderate to high effect sizes (Domínguez-Lara, 2017), but two of the studies that considered the dimensions of QoL and mindfulness obtained non-significant results (Fernandes et al., 2019; Světlák et al., 2021). As for third variables between QoL and TM, four studies considered mediating variables, including perceived stress (Valikhani et al., 2020) with high effect size (Domínguez-Lara, 2017), resilience (Cheung et al., 2020), and client cocreation effort (My-Quyen et al., 2020) with a low size, and rumination (Calvete et al., 2021), for which it is only reported to be significant. No studies considered moderating variables.
Risk of Bias Assessment
Table 2 provides the RBA for each study. Regarding overall risk, all studies presented risk. The study with the most irregularities was Fernandes et al. (2019), while the study with the best score was Valikhani et al. (2020).
Table 2. Risk of Bias Assessment
| Author and year | Title and summary | Introduction and objectives | Method and data | Sampling | Data analysis | Ethics and bias | Results | Transfer or generalization | Implications and usefulness |
|---|---|---|---|---|---|---|---|---|---|
| Azad et al., 2018 | Good | Good | Good | Average | Good | Good | Average | Average | Good |
| Calvete et al., 2021 | Average | Good | Good | Average | Average | Average | Good | Average | Good |
| Cheung et al., 2020 | Average | Good | Average | Good | Average | Good | Good | Good | Good |
| Fernandes et al., 2019 | Average | Average | Poor | Poor | Poor | Average | Average | Poor | Average |
| Im et al., 2020 | Average | Average | Good | Average | Poor | Average | Good | Average | Good |
| My-Quyen et al., 2020 | Average | Good | Poor | Average | Average | Very poor | Good | Average | Average |
| Ruiz-Fernández et al., 2020 | Average | Good | Good | Average | Good | Good | Good | Average | Average |
| Světlák et al., 2021 | Good | Good | Good | Average | Poor | Good | Average | Good | Poor |
| Valikhani et al., 2020 | Good | Good | Good | Average | Good | Good | Good | Average | Good |
| Yaghoubian & Babakhani, 2019 | Average | Average | Good | Average | Poor | Good | Average | Average | Good |
Discussion
The SR points to an increased interest in the relationship between QoL and TM in the adult population, especially in young adulthood, in the last five years. Approximately one third of the studies were conducted in Iran, mainly in soldiers, due to the fact that the characteristics and demands of their context can become highly stressful and they tend to present worrying mental health outcomes; therefore, there is the expectation that TM helps to reduce their stress and improve their QoL (Azad, et al., 2018; Valikhani, 2020). No studies were found that considered Latin American population.
It is noteworthy that almost half of the studies do not define QoL (Azad et al., 2018; Calvete et al., 2021; Fernandes et al., 2019; Valikhani et al., 2020). Although half of them use the World Health Organization instrument (WHO; WHOQOL-Bref; Azad et al., 2018; Calvete et al., 2021; Im et al., 2020; My-Quyen et al., 2020; Valikhani et al., 2020), only in two studies does the instrument match the definition proposed by the WHO (Im et al., 2020; My-Quyen et al., 2020), and most of them (Azad et al., 2018; Calvete et al., 2021; Im et al., 2020; Valikhani et al., 2020) considered QoL as a global score despite the fact that the WHOQOL-Bref is made to be measured with four dimensions, thus omitting the possibility of determining which dimensions have a greater or lesser relationship with respect to TM. Finally, some studies (Fernandes et al., 2019; Yaghoubian & Babakhani, 2019) used instruments to measure general health status, such as the SF-36 and the COOP Function questionnaire.
Regarding the definition of TM, most studies cited Baer (2003; Calvete et al., 2021; My-Quyen et al., 2020; Valikhani et al., 2020), however, six studies used the MAAS instrument (Azad et al., 2018; Calvete et al., 2021; Cheung et al., 2020; Valikhani et al., 2020; Yaghoubian & Babakhani, 2019) and not the Baer et al. (2006; FFMQ) one, despite the fact that in recent years it is considered to be the best instrument for mindfulness (Garcia & Demarzo, 2018). Only three studies used the FFMQ (Fernandes et al., 2019; Im et al., 2020; Světlák et al., 2021), two of which were interventions.
There is strong criticism of the MAAS instrument, since its function is to measure the state of mindful attention in habitual tasks, omitting other important principles of mindfulness, such as those that the FFMQ integrates, like the description of experience, conscious action, nonjudgmental experience, or non-reactivity, and not only that, but due to the inverse characteristic of its items, it is thought that what it measures is inattention (García & Demarzo, 2018; Rau & Williams, 2015).
In general, the relationship between QoL and TM was significant with moderate to high effect sizes (Domínguez-Lara, 2017), however, when considering dimensions, some studies (Fernandes et al., 2019; Světlák et al., 2021) found non-significant relationships, probably due to the instruments used to measure QoL:
Fernandes et al. (2019) only found a significant and high relationship between QoL and the Describe dimension of mindfulness, but The COOP Function questionnaire instrument was constructed to measure a patient's general functional health status with a single reverse item (Nelson et al., 1987; Pedrini et al., 2010). At the same time, the study by Světlák et al. (2021) used the SQUALA instrument for QoL, which has two dimensions, one referring to importance and the other to satisfaction; the relationships with the importance dimension were significant and moderate, but the satisfaction dimension of QoL, had no significant correlation with the dimensions: Acting with Attention, Non-Reactivity, and Non-Judgment, while with the rest of the dimensions the effect size was low.
Regarding third variables, only four studies reported mediating variables (Calvete et al., 2021; Cheung et al., 2020; My-Quyen et al., 2020), among which perceived stress had a high effect, as argued by Valikhani et al. (2020); this is because TM involves the ability to accept thoughts and feelings without reacting and without judgment, helping to minimize evaluations of stress, facilitating its processing, and leading to an improvement in QoL.
Another point to highlight is that all the studies presented a risk of bias, mainly with respect to data analysis, due to a minimal description of details, such as the way in which it was performed or the reasons for selecting the tests (Hawker et al., 2002). Likewise, the title and summary were considered “average” due to a lack of information; sampling, due to unjustified size and/or lack of information; and transfer and generalization due to lack of description of the context to replicate or compare, or because of sampling difficulties (Hawker et al., 2002).
Most studies reported the following as limitations: not being able to test causality over time, self-report measures, lack of instrument adaptation or low reliability, generalizability or non-probability sampling, small sample sizes and using the MAAS as a unidimensional measure (Azad et al., 2018; Calvete et al., 2021; Cheung et al., 2020; Fernandes et al., 2019; Im et al., 2020; My-Quyen et al., 2020; Ruiz-Fernández et al., 2020; Světlák et al., 2021; Valikhani et al., 2020; Yaghoubian & Babakhani, 2019). Also, some studies (Calvete et al., 2021; Fernandes et al., 2019; Ruiz-Fernández et al., 2020; Světlák et al., 2021) did not report psychometric properties beyond Cronbach's alpha, or whether the instruments used were adapted (Cheung et al., 2020; Im et al., 2020).
This study had a number of limitations: other languages such as Portuguese or French were not considered, interventions were integrated as long as they had a measure of association at baseline, one of the studies that passed the screening measured mindfulness using a dimension of the Self-Compassion-Scale because the abstract specified that mindfulness had been measured, however, during the screening other studies that used this scale were discarded because it was not considered an instrument to measure mindfulness in its entirety. In addition, the RBA tool used (Hawker et al., 2002) does not consider some important items such as adaptations or psychometric properties of the instruments.
Most studies included (Azad et al., 2018; Calvete et al., 2021; Cheung et al., 2020; Im et al., 2020; My-Quyen et al., 2020; Ruiz-Fernández et al., 2020; Valikhani et al., 2020; Yaghoubian & Babakhani, 2019) conclude that TM can improve people's QoL moderately to highly, because they tend to accept and cope with their thoughts and emotions in a mindful, non-reactive, and non-judgmental way, minimizing negative effects such as stress, by generating a more positive cognitive evaluation process, and thus increasing well-being and QoL, as well as enabling the ability to respond more appropriately.
The above coincides with what Baer (2003) proposed about how mindfulness skills can help to reduce symptoms and change behaviors through exposure, by focusing attention on sensations of pain or discomfort, assuming a nonjudgmental attitude towards cognitions, emotions, and impulses that usually accompany these sensations; cognitive change, which arises after this process, creating an understanding that thoughts are not an accurate representation of reality and there is no need to avoid them; self-management, since self-observation promotes the recognition of early signs of a problem as well as the use of coping skills; relaxation, which can occur in certain cases; and acceptance, by experiencing an event without trying to change the present experience.
The results show a positive relationship between QoL and TM. Therefore, it is advisable to encourage this trait in the adult population, and it is possible to integrate mindfulness training through formal and informal practices as part of interventions and public policies to increase the QoL of adults. However, considering the few studies that define TM and QoL as multidimensional constructs, the heterogeneity among the definitions and measures, and the bivariate relationship studied, together with the limitations reported, it is suggested that future studies continue to investigate this relationship, report the adaptations and psychometric properties of the instruments used, consider the various dimensions of QoL and TM, and explore the mechanisms that may explain the relationship.