My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO  Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.96 n.3 Madrid Mar. 2004
| ORIGINAL PAPERS |
Adhesive small bowel obstruction: predictive value of oral contrast
administration on the need for surgery
J. Perea García, F. Turégano Fuentes, B. Quijada García, A. Trujillo, P. Cereceda, B. Díaz Zorita,
D. Pérez Díaz and M. Sanz Sánchez
Emergency Department. Surgical Section. Universitary General Hospital Gregorio Marañón. Madrid, Spain
ABSTRACT
Introduction: adhesive small bowel obstruction (SBO) is a common cause of hospital admission. Nonoperative management is initially recommended unless there is suspicion of strangulation, but its optimal duration is controversial. The aims of our study was to evaluate the usefulness of radiographic small bowel examination with contrast medium to predict the need for surgery in SBO.
Material and methods: this prospective study carried out from January 1999 to December 2001, included 100 patients with clinical and radiological criteria of adhesive SBO. We described the past medical history, as well as clinical picture, blood tests and radiological findings in these patients. Fifty cubic centimeters of 5% barium suspension were given orally, and plain abdominal radiographs were taken at 4, 8, 16, and 24 hours afterwards. A liquid diet was given as soon as the contrast medium appeared in the right colon. Otherwise, surgical intervention was considered based on the outcome of the patient and the criteria of the emergency surgical team.
Results: in 70 patients, barium contrast appeared in the right colon, and a liquid diet was tolerated by 69 of them (98.6%). Mean hospitalization time for this group was 43 ± 17 hours. In the remaining 30 patients, no evidence of barium contrast in the right colon was seen, and 25 of them underwent surgery (75%), while the other 5 tolerated a liquid diet. Mean hospitalization time for this second group of patients was 13.8 ± 11 days. Sensitivity, specificity, positive predictive value, and negative predictive value for the absence of contrast medium in the right colon within 24 hours as a predictor of surgery were 93, 96, 98 and 83%, respectively. There was a statistical significant relationship (p < 0.01) between the "Presence of contrast medium in the right colon" and "Oral diet tolerance". Only the variable "Number of previous surgical interventions" tended to reach statistical significance (p = 0.07). Tolerance of liquid diet was more likely when patients had more than one previous abdominal surgery.
Conclusions: early oral administration of a radiological contrast medium in patients with adhesive SBO can effectively predict the need for a surgical procedure. It can shorten not only hospital stay, but also the potential morbidity of late surgery, secondary to a prolonged and unsuccessful nonoperative treatment.
Key words: Small bowel obstruction. Adhesive syndrome. Radiological contrast. Surgery.
Perea García J, Turégano Fuentes F, Quijada García B, Trujillo A, Cereceda P, Díaz Zorita B, Pérez Díaz D, Sanz Sánchez M. Adhesive small bowel obstruction: predictive value of oral contrast administration on the need for surgery. Rev Esp Enferm Dig 2004; 96: 191-200.
Recibido: 24-07-03.
Aceptado: 14-10-03.
Correspondencia: José Perea García. C/ Meléndez Valdés, 54, 4º C. 28015 Madrid. Telf.: 915498994.
INTRODUCTION
Adhesive small bowel obstruction (SBO) is a common cause of hospital admission. Clinical evolution is unpredictable and its management is controversial. Surgery is immediately performed when there are signs and symptoms suggesting intestinal strangulation (1); otherwise, and in most cases, initial treatment must be nonoperative (2,3). However, the duration of this treatment remains controversial (from 12 hours to 5 days) (2,4-6), and, from a clinico-radiographic point of view, it is very difficult to predict initially which patients will ultimately need an operation. In our hospital many patients undergo surgery after 72 hours or more of nonoperative treatment, which potentially may contribute to increase the morbidity of these patients. Moreover, there are cases of spontaneous resolution after 4 to 5 days of nonoperative management, and surgery may be avoided in these patients.
This potential use of a radiological contrast has been recently evaluated. It has been suggested that its appearance in the cecum would be indicative of spontaneous resolution of the obstruction. Otherwise, the need for a surgical intervention is predicted (5,7-9). There is also a possible therapeutic effect of water-soluble contrast media (Gastrografin™: sodium diatrizoate, meglumide ditrizoate, humidifying agent) on obstruction resolution (6,7,10-12).
We describe a prospective trial of patients who presented with adhesive SBO, to whom a radiological contrast medium was given early, with the objective of assessing its use in predicting the need for surgery, the mean hospital stay, and the potential morbidity of a surgical procedure.
MATERIAL AND METHODS
Study design and selection of patients
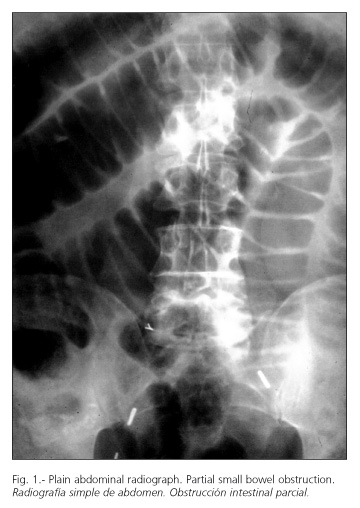
An evaluation study for a diagnostic method defined as Radiological Contrast Trial to establish need of surgery, in patients admitted to our Emergency Department from January 1999 to December 2001 with clinical and radiological features of adhesive SBO (Fig. 1). Exclusion criteria included patients with clinical evidence of intestinal strangulation and those who developed SBO within 30 days after surgery.
Technique
Once a clinical and radiological diagnosis of adhesive SBO was made, patients were managed with intravenous fluids and a nasogastric tube for 2 hours. No analgesic treatment was given. Then, 50 cc of 5% diluted barium suspension were given orally or through the nasogastric tube, which was clamped thereafter.
Abdominal radiographs were taken at 4, 8, 16 and 24 hours afterwards. As soon as barium appeared in the right colon (Fig. 2) oral liquids were given. Otherwise, an indication of surgery was established based on clinical and radiological outcome and the decision of the attending surgeon. Patients with increased abdominal pain at any time underwent laparotomy and were excluded from the study. We used barium suspension instead of Gastrografin™, since our preliminary study with this water-soluble contrast medium did not allow a proper view of the gastrointestinal tract in most cases. The concentration of barium was chosen by our radiologists, and was low enough to prevent complications in case of surgery.Variables
Primary variable: effective tolerance of a liquid diet in the absence of vomiting, nausea, or abdominal pain. Secondary variables: Age, sex, previous abdominal surgery, previous hospitalizations because of SBO, clinical features, complementary data (fever, tachycardia, leukocytosis), plain abdominal radiographs at admission (partial or complete obstruction, depending on the presence or absence of gas within the distal colon). Possible complications because of contrast administration were assessed, as well as intraoperative findings, surgical technique, postoperative complications, and mean hospital stay.
Statistical analysis
Data were included in a data base and analyzed with the statistical software program SPSS (v 9.0 for Windows). Confidence intervals (95%) for sensitivity, specificity, positive and negative predictive value, and overall test value were calculated with the EPIDAT program, version 2.1. Data are given using frequency values (absolute and proportions) for categorical variables, and mean, standard deviation and range values for quantitative measurements. The diagnostic test was evaluated using sensitivity, specificity, predictive values, and overall efficiency, with their respective confidence intervals (95% ICs). Looking for a variable related to effective tolerance, Student's t test was used for quantitative variables, and a Chi-square test (or its non-parametric equivalent: Fi-sher's test) in case of dicotomic variables. A p < 0.05 was considered significant.
RESULTS
Male to female ratio was 44/56, with a mean age of 64 years (range: 23-100). Previous abdominal surgery and stays due to adhesive SBO, as well as clinical outcome, are shown in tables I and II. They all had at least one previous abdominal operation, only one in most cases (67 cases), with a mean of 1.4 previous operations, and a median time between present admission and last abdominal surgery of 5.5 years.
All 100 patients were included in the trial, with a mean time from admission to our Emergency Department to barium administration of 16 hours. Seventy patients had contrast medium in the right colon at a median 8 hours since administration, and an effective liquid diet was tolerated by 69 of them. The remaining patient underwent surgery 48 hours after admission, and an internal hernia was found during laparotomy. None of them experienced complications related to contrast medium administration. The 69 patients who tolerated liquid diet had a clinical and radiological resolution of SBO at 43 ± 17 hours after admission to the Emergency Department and were discharged from hospital.
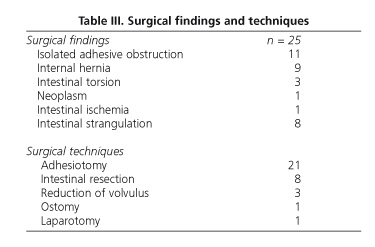
The remaining 30 patients had no contrast medium in the right colon in none of the abdominal radiographs, al-though the medium appeared in the small bowel in 15 of them (50%). In 25 of these 30 patients, surgery was performed because of lack of improvement at a mean 43 hours after admission (minimum: 6 hours; maximum: 72 hours); meanwhile, the remaining 5 patients were put on a liquid diet because of clinical improvement. The minimum time of 6 hours occurred in a patient who had markedly increased abdominal pain and underwent surgery without ever completing the trial. Findings and surgical techniques are described in table III. No cases of perforation with barium spillage in the peritoneal cavity were found, and the presence of barium did not increase the difficulty of small bowel resection. One patient who had small bowel ischemia of thrombotic origin was originally misdiagnosed of SBO. Five patients developed postoperative complications (20%), including three wound infections, one urinary tract infection, and one ileus. One patient died at day 4 after surgery because of congestive heart failure (postoperative mortality was 4%, and 1% overall in the series).
Mean hospitalization time was 13.8 ± 11 days (range: 5-55 days) for the 30 patients without evidence of contrast medium in the right colon.
Of the 25 patients with initial radiological evidence of complete obstruction, 17 were treated nonoperatively (68%) and 8 underwent operative management on (32%). Of the 75 patients with partial obstruction, 58 were treated nonoperatively (77%) and 17 were managed surgically (23%).
Sensitivity, specificity, positive and negative predictive values, and overall test value, of the absence of contrast medium in the right colon within 24 hours as being predictive of the need for surgery, were 93, 96, 98, 83 and 94%, respectively (Table IV). In 15 patients no contrast appeared in any abdominal radiographs, and all of them underwent surgery because of lack of clinical and radiological improvement.
There was a statistical significant relationship between the presence of contrast medium in the right colon and the effective liquid tolerance. Likewise, absence of contrast in the right colon was associated with the need for surgery (p < 0.01). Only the variable "number of previous operations" tended toward statistical significance (p = 0.07). Thus, a positive oral tolerance was more likely if the patient had more than one previous abdominal surgery (pooled variable: "effective tolerance").
DISCUSSION
Adhesive SBO is a common surgical emergency whose global management still remains controversial. Although in the absence of signs of strangulation nonoperative management is usually indicated, the duration of this treatment is very variable. Most authors recommend that this period of nonoperative treatment should not exceed 48 hours (6,13,14), although clinical evidence exists for spontaneous resolution after 4 or 5 days.
Demographic and clinical data of our patients are similar to those in other series, except the evidence of previous admissions for SBO, which was two times that of a recent report (15).
Only a few patients with adhesive SBO complain of severe abdominal pain, and the severity of such pain is a most important element for surgical decision. The presence of severe and continuous pain, with or without other signs, must make one suspect strangulation and indicate an emergency laparotomy. Nevertheless, a majority of patients will have a benign clinical presentation with abdominal distension and absent or mild pain.
Rates of operation in adhesive SBO vary between 27 and 42% (25% in our series). The fact that previous abdominal surgery of the inframesocolic compartment increases this rate is well known (2,15-17).
There are series in which predictive factors are used to help choose the best treatment in each case. Escrig et al. showed that absence of gas in the large bowel, electrolyte disorders, and inframesocolic location of previous surgery had all an independent predictive value for surgical intervention (15). In our series, only the larger numbers of previous operations seem to negatively predict the need for surgery. A complete radiological obstruction at the beginning, defined as an absence of gas in the colon, was neither predictive of absence of contrast medium in the colon, nor of possible indication for surgery. Of those who had contrast in the colon, 22% had initially a complete radiological obstruction, whereas 32% of those without contrast medium in the colon had a radiological obstruction. In our series, plain abdominal radiographs of complete SBO were not predictive of surgical management. Otherwise, the diagnostic approach we propose in this study would have been not necessary. Other authors have shown that the amount of nasogastric tube drainage, as well as the grade of dilatation of the small bowel loops, is predictive of surgical management (7). Nevertheless, it should be emphasized that clear risk factors for the failure of nonoperative treatment of this condition have yet to be identified.
The use of a water-soluble contrast medium has been recently evaluated with the aim of predicting the need for surgical intervention in SBO. The possible therapeutic role of this contrast medium still remains controversial. In a randomized study, Assalia et al. suggested that GastrografinTM administration shortened hospital stay and the need for surgery by 10% (6). On the other hand, Feigin et al., and Fevang et al. found no such advantages (11,12).
Chen et al. studied the predictive value of this type of water-soluble contrast in the management of adhesive SBO (5). They showed that patients with contrast in the right colon within 24 hours were all successfully managed with a nonoperative treatment. Laparotomy was necessary in 96% of patients who had no contrast in the right colon within 24 hours. Our study confirms the results obtained by Chen et al., but using a diluted barium suspension (5). Nevertheless, our negative predictive value was lower, as a number of patients without contrast in the right colon did not need any surgery.
A barium contrast concentration of 5%, as determined by the Radiology Department, theoretically prevented the risk of complications. This was calculated as the minimum concentration needed to allow a proper view of contrast in the bowel lumen. However, the use of a barium suspension avoided the osmotic properties of GastrographinTM, which may play a role in the spontaneous resolution of the SBO. An important aspect in our results is the total absence of contrast -in either the small or large bowel- in the plain abdominal radiographs of 15 patients. All of them underwent surgery because of lack of clinical improvement. We believe that a most probable explanation is that the absence of contrast was due to severe loop distension, with subsequent fluid and air accumulation and contrast dilution. It is reasonable to conclude that clinical improvement after nonoperative treatment is unlikely with such an extensive obstruction.
Hospital stay was shortened by this diagnostic approach to patients who finally did not require surgery, and our data show a mean stay at the Emergency Department of 43 ± 17 hours. Recent series report a mean stay of 6 days for those who received nonoperative treatment, very similar to that of patients who underwent surgery (15). If our results are confirmed by other groups, this protocol could reduce the time to laparotomy and also the duration of nonoperative management for adhesive SBO. Shorter duration of nonoperative management, and earlier surgery could as well reduce the rate of intestinal resections and their subsequent morbidity.
In conclusion, the early use of a radiological contrast (diluted barium suspension) in patients with adhesive SBO can predict the need for surgery in an earlier and more efficient way, with a subsequent reduction in the hospitalization time and potential late-surgery morbidity.
ACKNOWLEDGEMENTS
We are grateful to the Research Unit of our Institution for their collaboration in the statistical analysis of the data.
REFERENCES
1. Playforth RH, Holloway JB, Griffin WO. Mechanical small bowel obstruction: a plea for early surgical intervention. Ann Surg 1970; 171: 783-8. [ Links ]
2. Seror D, Feigin E, Szold A, Allweiss TM, Carmon M, Nissan S. How conservative can postoperative small bowel obstruction be treated? Am J Surg 1993; 165: 121-6. [ Links ]
3. Tanphiphat C, Chittmittrapap S, Prasopsunti K. Adhesive small bowel obstruction. A review of 321 cases in Thai hospital. Am J Surg 1987; 154: 283-7. [ Links ]
4. Brolin RE. Partial small bowel obstruction. Surgery 1984; 95: 145-9. [ Links ]
5. Chen SC, Lin FY, Lee PH, Yu SC, Wang SM, Chang KJ. Water-soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg 1998; 85: 1692-4. [ Links ]
6. Assalia A, Schein M, Kopelman D, Hirshberg A, Hashmonai M. Therapeutic effect of oral Gastrografin in adhesive, partial small bowel obstruction: A prospective randomized trial. Surgery 1994; 115: 433-7. [ Links ]
7. Choi HK, Chu KW, Law WL. Therapeutic value of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment. Ann Surg 2002; 236: 1-6. [ Links ]
8. Blackmon S, Lucius C, Wilson JP. The use of water-soluble contrast in evaluating clinically equivocal small bowel obstruction. Ann Surg 2000; 66: 238-44. [ Links ]
9. Chen SC, Chang KJ, Lee PH. Oral Urografin in postoperative small bowel obstruction. World J Surg 1999; 23: 1051-4. [ Links ]
10. Assalia A, Kopelman D, Bahous H. Gastrografin for mechanical, partial, small bowel obstruction due to adhesions. Harefuah 1997; 132: 629-33. [ Links ]
11. Feigin E, Seror D, Szold A. Water soluble contrast material has no therapeutic effect on postoperative small-bowel obstruction: Results of a prospective randomized clinical trial. Am J Surg 1996; 171: 227-9. [ Links ]
12. Fevang BT, Jensen D, Fevang J. Upper gastrointestinal contrast study in the management of small bowel obstruction -a prospective randomized study. Eur J Surg 2000; 166: 39-43. [ Links ]
13. Cox MR, Gunn IF, Eastman MC. The safety and duration of non-operative treatment for adhesive small bowel obstruction. Aust NZ J Surg 1993; 63: 367-71. [ Links ]
14. Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg 1993; 59: 125-8. [ Links ]
15. Escrig VJ, Ángel V, Senent V, Villegas C, Senis L, Salvador JL. Oclusión adherencial de intestino delgado: valores predictivos de la indicación quirúrgica. Cir Esp 2002; 72: 72-8. [ Links ]
16. Cox MR, Gunn IF, Eastman MC. The operative etiology and types of adhesions causing small bowel obstruction. Aust NZ J Surg 1993; 63: 848-52. [ Links ]
17. Matter I, Khalemsky L, Abrahamson J. Does the index operation influence the course and outcome of adhesive intestinal obstruction? Eur J Surg 1997; 163: 767-72. [ Links ]











 text in
text in