My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 n.4 Madrid Apr. 2009
Assessing the short- and long-term prognosis of patients with cirrhosis and acute variceal bleeding
Valoración del pronóstico a corto y largo plazo de pacientes con cirrosis y hemorragia digestiva por hipertensión portal
L. Sempere, J. M. Palazón, J. Sánchez-Payá1, S. Pascual, E. de Madaria, M. J. Poveda2, F. Carnicer, P. Zapater3 and M. Pérez-Mateo
Liver Unit. 1Epidemiology Service. Hospital General Universitario. Alicante, Spain.
2Gastroenterology Unit. Hospital General Universitario. Alcoy, Alicante, Spain.
3Clinical Pharmacology Unit. Hospital General Universitario. Alicante, Spain
This work was supported by grants from Instituto de Salud Carlos III (PI 04/90023 and PI 05/1574). Madrid, Spain.
ABSTRACT
Objective: to evaluate the efficacy of various indicators in predicting short- and long-term survival in patients with cirrhosis and acute variceal bleeding.
Material and methods: prognostic indicators were calculated for a cohort of 201 cirrhotic patients with acute variceal bleeding hospitalized in our center, a third-level teaching hospital. The studied variables were: age, sex, etiology of cirrhosis, endoscopic findings, previous variceal bleeding episodes, human immunodeficiency virus (HIV) infection, hepatocellular carcinoma (HCC), infection during episode, and Child-Turcotte-Pugh (CTP) and Model for End-stage Liver Disease (MELD) scores within 24 hours of bleeding onset. Patients were followed up for at least 6 months until death, liver transplantation, or end of observation.
Results: median follow-up was 66.85 weeks (range 0-432.4). The 6-week, 3-month, 12-month and 36-month mortality rates were 22.9, 24.9, 34.3, and 39.8%, respectively. Age ≥ 65 years, presence of HCC, CTP score ≥ 10, and MELD score ≥ 18 were the variables associated with mortality in the multivariate analysis. The accuracy of MELD scores as predictors of 6-week, 3-month, 12-month, and 36-month mortality was better than that of CTP scores (c-statistics: 6 week MELD 0.804, CTP 0.762; 3-month MELD 0.794, CTP 0.760; 12-month MELD 0.766, CTP 0.741; 36 month MELD 0.737, CTP 0.717).
Conclusion: MELD and CTP scores together with age and a diagnosis of hepatocellular carcinoma are useful indicators to assess the short- and long-term prognosis of patients with acute variceal bleeding.
Key words: Prognosis. Variceal bleeding. Portal hypertension. Child-Turcotte-Pugh score. MELD score.
RESUMEN
Objetivo: evaluar la eficacia de los diferentes indicadores pronósticos de supervivencia a corto y largo plazo en pacientes con cirrosis y hemorragia digestiva alta por hipertensión portal (HTP).
Material y métodos: calculamos los indicadores pronósticos en una cohorte de 201 pacientes con cirrosis y hemorragia digestiva por HTP ingresados en el Hospital General Universitario de Alicante. Las variables a estudio fueron: edad, sexo, etiología de la cirrosis, hallazgos endoscópicos, episodios previos de hemorragia digestiva por HTP. Infección por el virus de la inmunodeficiencia humana (VIH), hepatocarcinoma (HCC), infección bacteriana durante el episodio de hemorragia digestiva y clasificación de Child-Turcotte-Pugh (CTP) y el modelo para enfermedades terminales del hígado (MELD score) calculados dentro de las primeras 24 horas del inicio de la hemorragia. Los pacientes fueron seguidos al menos 6 meses hasta su muerte, trasplante hepático o final del seguimiento.
Resultados: la mediana de seguimiento fue de 66,85 semanas (rango 0-432,4). La mortalidad a las 6 semanas, 3 meses, 12 meses y 36 meses fue de 22,9, 24,9, 34,3 39,8%, respectivamente. La edad ≥ 65 años, la presencia de HCC, una clasificación de CTP ≥ 10 y un MELD score ≥ 18 fueron las variables asociadas a la mortalidad en el estudio multivariante. La precisión del MELD score como predictor de mortalidad a las 6 semanas, 3 meses, 12 meses y 36 meses fue superior a la de la clasificación de CTP (valor c-estadístico: 6 semanas MELD 0,804, CTP 0,762; 3 meses MELD 0,794, CTP 0,760; 12 meses MELD 0,766, CTP 0,741; 36 meses MELD 0,737, CTP 0,717).
Conclusión: el MELD score y la clasificación de CTP, junto con la edad y la presencia de HCC, son marcadores útiles en la valoración pronóstica de supervivencia a corto y largo plazo de los paciente con cirrosis y hemorragia digestiva por HTP.
Palabras clave: Pronóstico. Hemorragia digestiva varicosa. Hipertensión portal. Clasificación de Child-Turcotte-Pugh. MELD score.
Introduction
Acute variceal bleeding is a frequent complication of cirrhosis with high mortality (1). Advances in pharmacological and endoscopic therapies have led to a decrease in mortality over the past two decades (2,3). Mortality at 6 weeks seems to be more related to stage of liver disease than to bleeding severity (4). Nowadays the adequate management of portal hypertension with the prophylactic treatment of variceal rebleeding has increased survival for patients with a history of variceal bleeding permitting the progression of liver disease (5).
Many prognosis models for liver disease have been developed for patients with cirrhosis. At present the most highly used ones are the Child-Turcotte-Pugh (CTP) and Model for End-stage Liver Disease (MELD) scores (6-8). Recent papers have validated the ability of both models to predict short-term survival in patients with acute variceal bleeding (9-11). It seems interesting to assess the ability of prognosis models to predict survival beyond 12 months since variceal bleeding. On the other hand important changes in the natural history of cirrhosis - increased incidence of hepatocellular carcinoma (HCC) and co-infected hepatitis with hepatitis C virus (HCV) and human immunodeficiency virus (HIV) - have occurred in the last few years (12,13).
Changes in the natural history of cirrhosis made it necessary to review all factors implicated in the survival of patients with acute variceal bleeding. Thus, the main objective of this study was to assess the prognostic indicators of short- and long-term survival in patients with cirrhosis and acute variceal bleeding in a recent series of patients.
Patients and methods
Study population
We present a retrospective study of patients with cirrhosis and acute variceal bleeding admitted to Hospital General Universitario, Alicante, between January 1996 and December 2003. Cases were identified by prospective database searching and variables were extracted from clinical records. We included only the earliest episode for each patient (one episode per patient). The diagnosis of liver cirrhosis was based on liver histology or a combination of clinical, biochemical, and ultrasonographic findings. The diagnosis of acute variceal bleeding was based on the presence of hematemesis and/or melena at admission, and active variceal bleeding or nonbleeding varices but evidence of blood with no other potential source of gastrointestinal bleeding on endoscopy. Our exclusion criteria included age younger than 18 years, significant cardiopulmonary comorbidity, organic renal disease, neurological disease, malignant tumors (except HCC), previous severe infection (except spontaneous bacterial peritonitis), severe immunodeficiency (except HIV infection), liver transplantation, and inability to obtain scores on the first day of variceal bleeding.
Predictor variables
Laboratory data and scores were determined within 24 hours of bleeding onset, with the first available laboratory test performed before blood derivative transfusions. For the calculation of the CTP score we used the Pugh score modification (6). The MELD score was calculated using the original formula without including the cause of liver disease (7).
MELD score = 0.957 x loge (creatinine mg/dL) + 0.378 X loge (bilirubin mg/dL) + 1.120 x loge (INR) + 6.43.
The additional variables studied were: age, sex, etiology of cirrhosis, endoscopic findings, previous episodes of variceal bleeding, HIV infection, presence of HCC, and infection during episode.
The diagnosis of HCC was made according to the Barcelona-2000 conference on the clinical management of hepatocellular carcinoma (14). Bacterial infection at admission and its development during hospitalization were defined as the presence of non-contaminated positive cultures of organic fluids or fever ≥ 38 ºC lasting more than 24 hours.
All patients, including the cohort with HCC, were managed for acute bleeding and rebleeding prevention according to Baveno Consensus guidelines (15-17).
Outcome variables
Survival was calculated from the date of variceal bleeding. Patient outcome was obtained from hospital records and phone contacts. Patients were followed until death, liver transplantation, or end of observation (June 30, 2004). Transplanted patients were censored on the day of liver transplantation. Patients lost to follow-up before end of observation were censored at the last date known to be alive.
Mortality due to the episode of variceal bleeding included in the study was defined as death within 6 weeks of episode onset. Late mortality was defined as death after 6 weeks from variceal bleeding onset.
Short-term survival was defined as the interval from the date of bleeding to 3 months later. Long-term survival was defined as survival after 12 months from bleeding onset.
Statistical methods
In order to investigate the efficacy of the parameters to discriminate groups of different survival rates we used survival curves. Univariate survival curves were estimated using the Kaplan-Meier method and compared using the Log-rank test. We selected score cut-offs by means of receiver operating characteristic (ROC) curves with specificity around 90% to avoid a high number of false positive results. The multivariate analysis was performed using the Cox regression test to identify independent predictors of mortality. For all analyses a p value lower than 0.05 was considered statistically significant.
To compare the accuracy of scores as predictors of mortality we employed concordance c-statistics; this index is equivalent to the area under the ROC curve. A score with a c-statistic > 0.7 should be considered useful. C-statistics were applied for 6-week, 3-month, 12-month, and 36-month survival.
An additional statistical analysis was made to validate the UNOS-modified MELD score. The UNOS-modified MELD score was calculated using the formula available at: http://www.mayoclinic.org/gi-rst/mayomodel6.html.
Results
Between January 1996 and December 2003, 270 variceal bleeding episodes were recorded for 215 cirrhotic patients admitted to our Unit. We included only the earliest bleeding episode for each patient. Fourteen patients were excluded from the analysis (6 patients had organic renal disease, 1 patient had a malignant tumor other than HCC, 1 patient had a previous severe infection, 2 patients had undergone liver transplantation, and 4 patients were impossible to score on the first day of variceal bleeding).
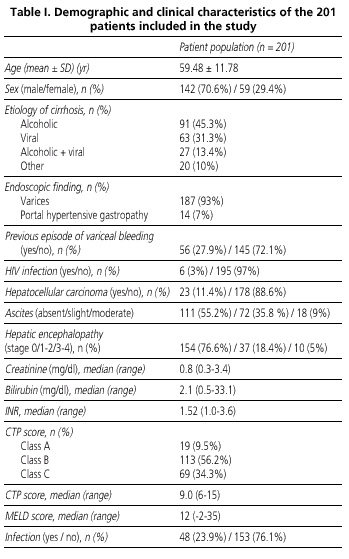
The demographic and clinical characteristics of the 201 patients eligible for the study are summarized in table I. Median follow-up was 66.85 weeks (range 0-432.4) and median survival was 207 weeks (range 0-432.4). The survival rate of the cohort was 77.1% at 6 weeks, 75.1% at 3 months, 65.7% at 12 months, and 60.2% at 36 months (Fig. 1). During follow-up, 96 patients (47.8%) died, 12 patients (6%) underwent liver transplantation, and 7 patients (3.5%) were lost to follow-up after discharge.
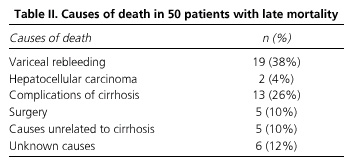
Of all 96 deaths, 46 (47.9%) patients died from the episode of variceal bleeding included in the study. The mortality rates of these episodes according to the presence of HCC were: patients without HCC 32/178 (17.2%) and patients with HCC 14/23 (60.8%). The causes of death in patients with late mortality are reported in table II - rebleeding was the main cause of late mortality.
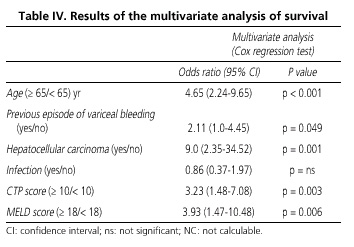
Tables III and IV report the statistical analysis of survival. On the univariate analysis (Table III) age ≥ 65, previous variceal bleeding, presence of HCC, infection during the episode, a CTP score ≥ 10, and a MELD score ≥ 18 were significantly associated with survival. The multivariate analysis (Table IV) confirmed age ≥ 65, presence of HCC, CTP score ≥ 10, and MELD score ≥ 18 as the independent predictors of mortality. Infection did not show significant differences, and previous variceal bleeding showed significant correlations but with confidence intervals (CIs) including the unit. Age ≥ 65 and presence of HCC were the variables with a higher odds ratio, 4.65 (95% CI 2.24-9.65) and 9.0 (95% CI 2.35-34.52), respectively. Figures 2, 3, 4 and 5 show survival curves according to independent predictor variables. Presence of HCC and a MELD score ≥ 18 were highly effective as predictors of short-term survival after bleeding (Figs. 3B and 5B). The four parameters discriminated between patients who survived and those who died after 12 months from bleeding, but age was the only variable that increased differences between both groups during the long-term survival study (Fig. 2).
The accuracy of the CTP and MELD scores in predicting mortality after variceal bleeding is shown in figure 6. MELD scores had a better discriminatory power than CTP scores at 6 weeks, 3 months, 12 months, and 36 months. The difference in accuracy between both models decreased in the prediction of long-term survival.
Similar results were obtained when all the statistical analyses for the UNOS-modified MELD score were repeated. The only difference was a cut-off value for the UNOS-modified MELD score of 19 points.
Discussion
Variceal bleeding represents a major complication in the natural history of cirrhosis, impairing the balance between portal pressure, and renal and liver function. Patients who suffer from liver and/or renal dysfunction during a bleeding episode can be divided into two groups. The first group comprises those who develop serious irreversible liver and/or renal dysfunction leading to death within a very short period of time. The second group of patients comprises those who suffer from temporary liver and /or renal dysfunction, the recovery of which allows them to get over the episode. In this group of patients this temporary dysfunction is likely indicative of advanced liver disease that remains unrecognized in non-stressful situations. It is not known whether this temporarily dysfunction can help us to stratify survival rates for this group. The introduction of the MELD score as a prognostic indicator in variceal bleeding, as opposed to the CTP score, allows an assessment of renal dysfunction. Impaired renal function has an important prognostic value in patients with advanced liver disease (18,19), even though the use of creatinine as marker in the presence of volume depletion is controversial given that its alteration may represent acute tubular necrosis. Probably early creatinine measurement demonstrates renal dysfunction as a reflection of previous functional renal impairment, not renal tubular necrosis. The current study supports the idea that patients with a poor clinical balance in the first day of variceal bleeding had damaged renal and liver function with prognostic value. The MELD score is a continuous system which takes into consideration objective parameters for liver and renal function. The use of these objective parameters and an accurate assessment of renal function may condition a higher predictive power as compared to the CTP score. In the CTP score the assessment of renal function by means of the presence of ascites is inadequate because it is well known that patients with ascites do not constitute a homogeneous group with similar prognoses (20,21). Albumin is another inappropriate parameter in the CTP score since protein loss during bleeding leads to early hypoalbuminemia even in non-cirrhotic patients.
The identification of patients with poor prognosis may be essential for the optimal short-term management of variceal bleeding. In the analysis of short-term survival the variables with higher discriminative power in predicting survival were the presence of HCC and the MELD score. Some authors assert that the development of HCC may accelerate the course of liver disease (22). Patients with HCC frequently have portal vein thrombosis, recurrent bleeding after endoscopic treatment, and a high mortality rate within 6 weeks of admission (4,23,24). Thus, short-term survival in patients with variceal bleeding and HCC is probably decreased as a consequence of advanced cirrhosis and difficult portal hypertension management.
In the analysis of long-term survival the discriminative power of MELD scores decreases and becomes similar to that of CTP scores (Fig. 6). We want to emphasize that this paper is the first study to evaluate the MELD score in the prediction of 36-month survival. Maybe for long-term prognosis liver disease staging could be better performed using changes in both models over time. It is well known that in patients with advanced cirrhosis an increasing MELD score is superior to initial CTP and MELD scores for the prediction of mid-term outcomes (25,26). According to the survival study (Fig. 2), the only parameter that increases differences in long-term survival is age. This fact is probably related to the presence of three factors in the older population: a longer duration of liver disease, a greater difficulty to overcome recurrent cirrhotic decompensations, and the absence of liver transplantation indications for the elderly in our country (27).
CTP and MELD scores are important indices in the evaluation of liver transplantation and other procedures, including portosystemic shunt. Our results support that both scores maintain their capacity on the first day of acute variceal bleeding. This study has the limitations of retrospective studies, but the high differences found in the statistical analysis could make these results useful for the management of patients with a recent episode of variceal bleeding.
In summary, assessing liver disease stage within 24 hours of bleeding onset, together with age and a diagnosis of HCC, is useful to assess the short- and long-term prognosis of cirrhotic patients with acute variceal bleeding. In addition, the prognostic variables obtained may be useful to define strategies for management improvement in these patients.
![]() Correspondence:
Correspondence:
Laura Sempere.
Unidad Hepática.
Hospital General Universitario.
C/ Pintor Baeza, s/n,
03010 Alicante, Spain.
e-mail: sempere_lau@gva.es
Received: 28-01-09.
Accepted: 05-02-09.
References
1. Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology 1981; 80: 800-9. [ Links ]
2. Chalasani N, Kahi C, Francois F, Pinto A, Marathe A, Bini EJ, et al. Improved patient survival after acute variceal bleeding: a multicenter, cohort study. Am J Gastroenterol 2003; 98: 653-9. [ Links ]
3. Carbonell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology 2004; 40: 652-9. [ Links ]
4. D'Amico G, De Franchis R and Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology 2003; 38: 599-612. [ Links ]
5. Bosch J, García-Pagan JC. Prevention of variceal rebleeding. Lancet 2003; 361: 2244-5. [ Links ]
6. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973; 60: 646-9. [ Links ]
7. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000; 31: 864-71. [ Links ]
8. Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003; 124: 91-6. [ Links ]
9. Chalasani N, Kahi C, Francois F, Pinto A, Marathe A, Bini EJ, et al. Model for end-stage liver disease (MELD) for predicting mortality in patients with acute variceal bleeding. Hepatology 2000; 35: 1282-4. [ Links ]
10. Lee JY, Lee JH, Kim SJ, Choi DR, Kim KH, Kim YB, et al. Comparison of predictive factors related to the mortality and rebleeding caused by variceal bleeding: Child-Pugh score, MELD score, and Rockall score. Taehan Kan Hakhoe Chi 2002; 8: 458-64. [ Links ]
11. Amitrano L, Guardascione MA, Bennato R, Manguso F, Balzano A. MELD score and hepatocellular carcinoma identify patients at different risk of short-term mortality among cirrhotics bleeding from esophageal varices. J Hepatol 2005; 42: 820-5. [ Links ]
12. Bosh X, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology 2004; 127: s5-s16. [ Links ]
13. Mohsen AH, Easterbrook PJ, Taylor C, Portmann B, Kulasegaram R, Murad S, et al. Impact of human immunodeficiency virus (HIV) infection on the progression of liver fibrosis in hepatitis C virus infected patients. Gut 2003; 52: 1035-40. [ Links ]
14. Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 2002; 37: 874. [ Links ]
15. de Franchis R. Developing consensus in portal hypertension. J Hepatol 1996; 25: 390-4. [ Links ]
16. de Franchis R. Updating consensus in portal hypertension: report of the Baveno III consensus workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol 2000; 33: 846-52. [ Links ]
17. de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 2005; 43: 167-76. [ Links ]
18. Llach J, Gines P, Arroyo V, Rimola A, Tito L, Badalamenti S, et al. Prognostic value of arterial pressure, endogenous vasoactive systems, and renal function in cirrhotic patients admitted to the hospital for the treatment of ascites. Gastroenterology 1988; 94: 482-7. [ Links ]
19. Fernández-Esparrach G, Sánchez-Fueyo A, Gines P, Uriz J, Quinto L, Ventura PJ, et al. A prognostic model for predicting survival in cirrhosis with ascites. J Hepatol 2001; 34: 46-52. [ Links ]
20. Arroyo V, Rodes J, Gutiérrez-Lizarraga MA, Revert L. Prognostic value of spontaneous hyponatremia in cirrhosis with ascites. Am J Dig Dis 1976; 21: 249-56. [ Links ]
21. Arroyo V, Bosch J, Gaya-Beltran J, Kravetz D, Estrada L, Rivera F, et al. Plasma renin activity and urinary sodium excretion as prognostic indicators in nonazotemic cirrhosis with ascites. Ann Intern Med 1981; 94: 198-201. [ Links ]
22. D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 2006; 44: 217-31. [ Links ]
23. Yeo W, Sung JY, Ward SC, Chung SC, Lee WY, Li AK, et al. A prospective study of upper gastrointestinal hemorrhage in patients with hepatocellular carcinoma. Dig Dis Sci 1995; 40: 2516-21. [ Links ]
24. Sung JJ, Yeo W, Suen R, Lee YT, Chung SC, Chan FK, et al. Injection sclerotherapy for variceal bleeding in patients with hepatocellular carcinoma: cyanoacrylate versus sodium tetradecyl sulphate. Gastrointest Endosc 1998; 47: 235-9. [ Links ]
25. Merion RM, Wolfe RA, Dykstra DM, Leichtman AB, Gillespie B, Held PJ. Longitudinal assessment of mortality risk among candidates for liver transplantation. Liver Transpl 2003; 9: 12-8. [ Links ]
26. Huo TI, Wu JC, Lin HC, Lee FY, Hou MC, Lee PC, et al. Evaluation of the increase in model for end-stage liver disease (DeltaMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J Hepatol 2005; 42: 826-32. [ Links ]
27. Prieto M, Clemente G, Casafont F, Cuende N, Cuervas-Mons V, Figueras J, et al. Consensus document on indications for liver transplantation 2002. Gastroenterol Hepatol 2003; 26: 355-75. [ Links ]











 text in
text in