My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 n.10 Madrid Oct. 2009
LETTERS TO THE EDITOR
Thoracic pseudocyst of pancreatic origin with cervical involvement
Pseudoquiste torácico de origen pancreático con afectación cervical
Key words: Pancreatic pseudocyst. Cervical pseudocyst. Chronic pancreatitis.
Palabras clave: Pseudoquiste pancreático. Pseudoquiste cervical. Pancreatitis crónica.
Dear Editor,
Pancreatic pseudocysts often occur in the setting of acute or chronic pancreatitis. Their usual location is the abdominal cavity, surrounding the pancreas. Less commonly, they can spread into the thoracic cavity as an esophago-pleural fistula or as a true mediastinal pseudocyst (1,2). Very uncommon, however, is the existence of communication with the cervical region (2-4).
Case report
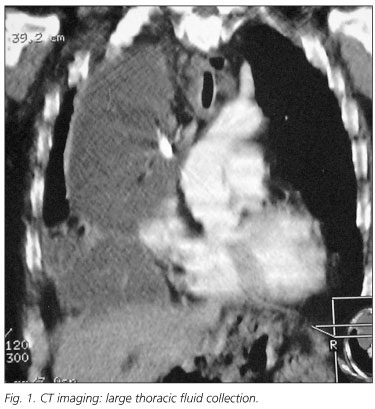
We report the case of a 59-year-old man with antecedents of alcoholic chronic pancreatitis admitted because of respiratory failure. A right pleural effusion was shown after physical examination and chest X-ray. After diagnostic thoracocentesis the patient had dyspnea, superior vena cava syndrome and mediastinal widening, observed on a second chest X-ray. A large thoracic fluid collection was found on CT with no pathological findings in the abdomen (Fig. 1). It was drained by means of a thoracic tube. The fluid had high amylase concentration (104,000 U/ml). An area of swelling also appeared in the neck and, after stab incision, an amylase-rich fluid was drained (90,000 U/ml). The drainage of both cervical and thoracic collections improved the dyspnea and stabilized the patient. Then, studies to confirm the suspected pancreatic origin of the collections were performed. The Wirsung duct appeared on ERCP to be irregular but without dilation and communicated with the pleura. A plastic stent was inserted into the pancreatic duct leading to fistula closing, resulting in a fast patient recovery without need of surgery. The stent was in place for 3 months and then endoscopically removed. He was still doing well two years later.
Discussion
Pseudocysts can be classified into acute and chronic. Chronic pseudocysts are constituted by pancreatic juice enclosed by a wall of fibrous or granulation tissue, arising as a consequence of chronic pancreatitis - as is our case - without any antecedent episode of acute pancreatitis (5). The reported incidence of chronic pseudocysts is 20-40% of chronic pancreatitis (5). On the other hand, acute pseudocysts have the same histologic features but are associated with an episode of acute pancreatitis. The usual location of pseudocysts is around the pancreas although extension into the abdominal cavity, pelvis, groin and even the scrotum has been described. However, the fluid occasionally reaches the pleura or the mediastinum (1,2,6) through the aortic and esophageal hiatus and, less commonly, through the foramen of Morgagni or directly eroding the diaphragm. Mediastinal pseudocyst symptoms are variable: abdominal, back or chest pain, dyspnea, dysphagia, odynophagia, weight loss and even cardiac tamponade (1,2). A location exceptionally reported is the cervical region (2-4) as in our case, which is usually due to spreading of mediastinal collections. The diagnosis of mediastinal pseudocysts is usually made by CT scanning, although can be suspected if mediastinal widening is seen on chest X-ray. The diagnosis can be even more difficult if radiological abdominal findings are lacking, as in this case. The treatment of mediastinal pseudocysts needs drainage, either percutaneous or surgical. The cervical collection should also be drained. Then, a possible underlying pancreatic duct disruption must be searched and treated if confirmed to lead to complete pseudocyst resolution. Two main successful endoscopic options have been described: transpapillary insertion of a pancreatic stent (7) and transgastric drainage of the abdominal part of the pseudocyst followed by stent insertion (2,6). Since in our case there was neither Wirsung duct dilation on ERCP nor abdominal collection on CT, and thus the pseudocyst was classified as D'Edigio type 2, we thought that immediate surgery was not needed and chose the endoscopic option (8,9). In conclusion, mediastinal and cervical location of a pancreatic pseudocyst is possible but uncommon and can be successfully treated by external drainage and transpapillary endoscopic stenting.
J. C. Rodríguez Sanjuán, M. González Noriega, L. A. Herrera and M. Gómez Fleitas
Department of Surgery. University Hospital Marqués de Valdecilla. University of Cantabria. Santander, Spain
References
1. Rose EA, Haider M, Yang SK. Mediastinal extension of pancreatic pseudocyst. Am J Gastroenterol 2000; 95: 3638-9. [ Links ]
2. Topa L, Lászlo F, Sahin P, et al. Endoscopic transgastric drainage of a pancreatic pseudocyst with mediastinal and cervical extensions. Gastrointest Endosc 2006; 64: 460-3. [ Links ]
3. Karantanas AH, Sandris V, Tsikrika A, et al. Extension of pancreatic pseudocysts into the neck: CT and MR imaging findings. AJR Am J Roentgenol 2003; 180: 843-5. [ Links ]
4. Petropoulos AE, Cheney ML, Agathos A, et al. A peripatetic pancreatic pseudocyst in the neck. J Otolaryngol 2000; 29: 247-50. [ Links ]
5. Andrén-Sandberg A, Dervenis C. Pancreatic Pseudocysts in the 21st Century. Part I: Classification, Pathophysiology, Anatomic Considerations and Treatment. JOP. J Pancreas (Online) 2004; 5: 8-24. Available at: http://www.joplink.net/ [ Links ]
6. Mohl W, Moser C, Kramann B, et al. Endoscopic transhiatal drainage of a mediastinal pancreatic pseudocyst. Endoscopy 2004; 36: 467. [ Links ]
7. Mallavarapu R, Habib TH, Elton E, et al. Resolution of mediastinal pancreatic pseudocysts with transpapillary stent placement. Gastrointest Endosc 2001; 53: 367-70. [ Links ]
8. D'Edigio A, Schein M. Pancreatic pseudocysts: a proposed classification and its management implications. Br J Surg 1991; 78: 981-4. [ Links ]
9. Bergman S, Melvin WS. Operative and nonoperative management of pancreatic pseudocysts. Surg Clin N Am 2007; 87: 1447-60. [ Links ]











 text in
text in