Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 no.11 Madrid Nov. 2009
LETTERS TO THE EDITOR
Syphilitic hepatitis: case report
Hepatitis sifilítica: caso clínico
Key words: Hepatitis. Secondary syphilis. Clinical manifestations.
Palabras clave: Hepatitis. Sífilis secundaria. Manifestaciones clínicas.
Dear Editor,
Nowadays, the presence of secondary or tertiary syphilis as a sexually transmitted disease is unusual. Although reports exist of cases of syphilis-associated hepatitis, its onset as a form of disease presentation is very unusual. We present a case of parenchymatous jaundice in a young man who was diagnosed with secondary syphilis after the appearance of cutaneous symptoms of the disease.
Case report
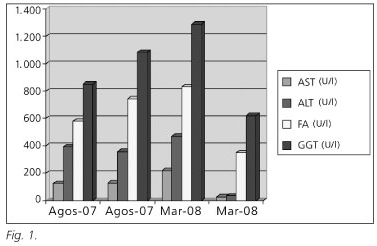
We treated a patient who presented to the emergency department with a one-month history of asthenia, accompanied by painless jaundice that had appeared several days earlier. Personal history of note included reflux disease and erosive duodenitis that had been successfully treated five years previously. The patient was not currently receiving any treatment. Risk factors for liver disease included risky sexual relations four months beforehand. Physical examination showed a yellowish skin and mucous membranes, with no other notable findings. A blood test taken on admission showed a normal leukocyte count and formula, an increase in total bilirubin (5.46 mg/dL) at the expense of direct bilirubin (4.30 mg/dL), and raised aspartate aminotransferase (AST), 128 U/L (normal value < 39); alanine aminotransferase (ALT), 357 U/L (normal value < 40); alkaline phosphatase, 743 U/L (normal value < 129) and gammaglutamyltransferase (GGT), 1083 U/L (normal value < 50) (Fig. 1). Clotting parameters were within normal limits. An abdominal ultrasound study was normal. Evolution: given the good general state of the patient and the absence of data suggesting hepatocellular failure, the patient was discharged and given an outpatient's appointment for further study. Serological tests for HAV, HBV, HCV, HIV, EBV, herpes simplex virus 1 and 2, and CMV were all negative for acute infection, as were tests for atypical bacteria, including Chlamydia pneumoniae, Mycoplasma pneumoniae, Coxiella burnetti and Legionella. Screening tests for Brucella, Salmonella Typhi and Paratyphi were also negative. An autoimmune disorder was ruled out by negative tests for ANA, AMA, Anti-LKM, anti-smooth muscle antibodies and P-ANCA. Immunoglobulins, including IgE, were all normal. Studies of iron metabolism, urinary copper and ceruloplasmin were normal, as was alpha-1 antitrypsin. During this period the levels of bilirubin and aminotransferase became normal, but the levels of alkaline phosphatase (832 U/L) and GGT (1289 U/L) remained high. At the outpatient's visit, the patient reported small macular, erythematous, nonconfluent lesions on the trunk, back, both arms, palms and soles (Figs. 2 and 3).
Given the history of at risk sexual behaviour and the skin lesions, a lues serology was ordered and proved positive, with a rapid plasma reagin (RPR) of 1/64 and a Treponema Pallidum haemagglutination (TPHA) titre of 1/1280, validated by ELISA. The patient was treated with penicillin G benzathine at a dose of 2.4 mill IU per week over four weeks. The patient is currently clinically asymptomatic, with normalisation of the analytical parameters (four-fold reduction in RPR) with persistence of a low titre of TPHA (1/20) and improvement of the cutaneous symptoms. He is being followed up by the Infectious Diseases Unit of the hospital. Diagnosis: syphilitic hepatitis.
Discussion
Syphilitic hepatitis is becoming less and less common, given the possibilities for early diagnosis and treatment that are now available. It occurs as a consequence of invasion of the liver by spirochetes during the dissemination phase. Analytically, it is characterised by a very marked rise in alkaline phosphatase and a positive lues serology. We believe that syphilis should be included in the differential diagnosis of predominantly cholestatic hepatitis and in cases of hepatitis with no known cause, especially in at risk groups.
C. Albandea-Moreno, V. M. Aguilar-Urbano, R. Rivera-Irigoin, J. Gonzalo-Marín, J. M. Rosales-Zabal,
A. Moreno-García, F. Fernández-Pérez, G. García-Fernández, A. Pérez-Aisa, I. M. Méndez-Sánchez and A. Sánchez-Cantos
Service of Digestive Diseases. Hospital Costa del Sol. Marbella, Málaga. Spain
Recommended references
1. Rodríguez Gil FJ, López Ávila A. Hepatitis sifilítica como primera manifestación de sífilis secundaria. Gastroenterol Hepatol 2006; 29(10): 652-4. [ Links ]
2. Schlossberg D. Syphilitic hepatitis: a case report and review of the literature. Am J Gastroenterol 1987; 82: 552-3. [ Links ]
3. Young MF, Sanowski RA, Manne RA. Syphilitic hepatitis. J Clin Gastroenterol 1992; 15: 174-6. [ Links ]











 texto em
texto em