Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.3 Madrid mar. 2010
Large lymph node size harvested as prognostic factor in gastric cancer?
¿Es el diámetro ganglionar mayor un factor pronóstico en cáncer gástrico?
F. Espín1, A. Bianchi1, S. Llorca1, L. Pulido1, J. Feliu1, J. de-la-Cruz1, E. Palomera2, O. García3, J. Remon4 and X. Suñol1
1 General Surgery Department. Universidad Autònoma de Barcelona.
2 Epidemiology and Estatistics Department,
3 Histology and Pathology Department, and
4 Clinical Oncology Department. Hospital de Mataró. Mataró. Barcelona, Spain
ABSTRACT
Objective: knowledge regarding prognostic factors in gastric cancer is essential to decide on single patient management. We aim to establish the value of large lymph node size in order to improve perioperative approach.
Material and methods: charts of one hundred and twenty-eight consecutive patients undergoing gastrectomy for resectable gastric cancer were reviewed between January 1996 and December 2005. Patients were split in two groups according to large lymph node size harvested, group I, lymph node size ≤ 10 mm and group II, lymph node size > 10 mm. Overall five-year survival related to cancer were analyzed as a main endpoint. Prognostic factors as TNM classification and degree of differentiation have been considered.
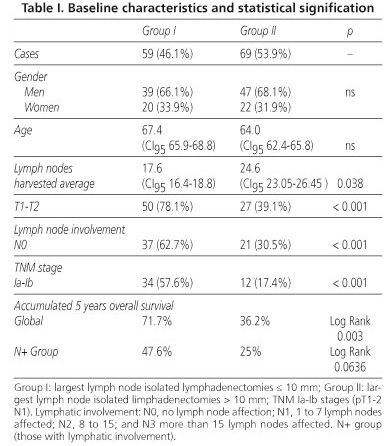
Results: there were no differences regarding age and gender (67.4 vs. 64; p = 0.34 and 66,1 vs. 68,1%; p = 0.27, respectively). Nevertheless, a significant difference has been found according to T1-T2 of TNM stage (78.1 vs. 39.1% p = < 0.001), for N grade staging, has statistical signification for grade N0 (62.7 vs. 30.5%; p < 0.001), and for Ia and Ib stages (57.6 vs. 17.4%). Five years overall survival has a great statistical signification (p log-rank = 0.0003), however, overall survival between groups with positive lymph nodes according to lymph node size was close to signification, (p log-rank = 0.0636).
Conclusions: our data indicates that large lymph node size could be a powerful predictor for overall survival in gastric cancer, when it could be evaluated in preoperative period. In our opinion lymph node size should be considered for perioperative chemotherapy schemas. Detection and staging techniques for lymph node affection acquire much more importance.
Key words: Gastric cancer. Lymphadenectomy. TNM staging. Postoperative survival.
RESUMEN
Objetivo: valorar el interés del diámetro del ganglio mayor extirpado como factor pronóstico en los pacientes intervenidos por cáncer gástrico, para determinar si su detección puede ser un factor de interés en el periodo preoperatorio, para indicar tratamiento neoadyuvante.
Material y métodos: se analiza un registro de 128 casos consecutivos de pacientes afectos de adenocarcinoma gástrico resecable, durante un periodo de 10 años en los que en el estudio anatomopatológico se determinó el diámetro del ganglio mayor aislado. Se estudia la relación del mismo con factores pronósticos universalmente aceptados, el grado de penetración, la presencia y extensión de metástasis ganglionares y el estadio TNM, y con la supervivencia a 5 años, estudiándose dos grupos, el grupo I compuesto por aquellos enfermos con diámetro menor o igual a 10 mm, y el grupo II con diámetros superiores a 10 mm.
Resultados: no se han detectado diferencias estadísticas respecto a edad y sexo (67,4 vs. 64; p = 0,34 y 66,1 vs. 68,1%; p = 0,27, respectivamente). Existen diferencias significativas entre ambos grupos en el grado de penetración tumoral, T1-T2, (78,1% por 39,1%, p < 0,001), en el porcentaje de pacientes sin metástasis ganglionares (62,7 vs. 30,5%; p < 0,001), así como en el porcentaje de estadios precoces (Ia y Ib, 57,6% por 17,4, p < 0,001). La supervivencia global acumulada a los 60 meses fue significativa entre ambos grupos (p log-rank = 0,0003), aunque sin alcanzar significación estadística en los pacientes N+ (p < 0,006).
Conclusiones: la relación del diámetro ganglionar mayor puede ser un factor pronóstico útil y junto con otros factores pronósticos facilitaría la valoración de quimioterapia neoadyuvante. Su detección mediante exploraciones complementarias adquiriría por consiguiente un mayor interés.
Palabras clave: Cáncer gástrico. Linfadenectomía. Estadificación TNM. Supervivencia postoperatoria.
Introduction
As it is well known, in order to face multidisciplinary treatment in many digestive neoplasms, it is basic to consider all of prognostic factors which can benefit patients undergoing perioperative therapy, trying to optimize long term results (1).
Main prognostic factors are based on histological assessment as type and degree of tumor differentiation, depth invasion and macroscopic appearance. Complete preoperative staging will be provided by image or endoscopic techniques that will allow us to evaluate tumor extension and affection of neighbour tissues, as well as, the presence of suspicious lymph nodes. To pursue an extended assessment sophisticated data based on genetics or tumoral markers could be done (2,3).
On the other hand, prognosis staging in gastric cancer is based on TNM classification, published by the International Union Against Cancer in 1997 (4). Lymph node affection is considered, for resectable patients, the most important prognosis-related factor which will also make the difference in patients' survival.
Lymph node size is directly related to metastatic affection, and with its detection in complementary explorations, like CT-scans or endoscopic ultrasound. Otherwise, lymph nodes size could take us directly to the hypothesis of having by itself a great prognosis value.
We have studied a group of patients operated on gastric cancer with curative intention during ten years period, and we have measured the influence of the largest lymph node diameter on staging, global and specifically accumulated survival.
Material and methods
Charts of 128 consecutive patients undergoing gastrectomy between January 1996 and December 2005 for resectable gastric carcinoma were reviewed. Patients included in the study were those who underwent a total or subtotal gastrectomy with an en bloc D2 lymphadenectomy.
All surgical ressected specimens were studied according a specific pathology schema; size of the largest lymph node harvested was measured. Patients were split into two groups according to large lymph node size; group I, largest lymph node sized ≤ 10 mm, and group II, those with largest lymph node sized > 10 mm.
Reliability of lymphadenectomy excision was analyzed due to average number of ressected lymph nodes in each group. Prognostic factors directly related with gastric cancer were analyzed; T stage or tumor depth of invasion, N stage or lymphatic affection, therefore we could differentiate in two subgroups, one containing all patients with affected lymph nodes (N1, N2, N3) in a single group named N+, and another without lymphatic involvement. M or distant metastatic affection contraindicates surgery and was not considered.
All of these TNM staging related factors allow us to establish six possible stages, of which we have finally analyzed the percentage of Ia and Ib stages in each group, in order to define a better prognostic group.
The main endpoint of our study was to analyze overall survival after 5 years follow-up, and interaction between overall survival and largest lymph node diameter in N+ patient.
Statistical analysis
The prognostic significance of lymph node size was determined by univariate analysis, Chi-square test and t-Student - U Mann-Whitney tests were used for testing differences between two case series, qualitative and quantitave variables respectively. For a 95% confidence interval values of p < 0.05 were considered to be significant.
Patients' survivals were determined by the Kaplan-Meier method. Log-rank test were applied for which p < 0.05 were considered to be significant.
The statistical analysis was performed with SPSS software (Version 10.0; SPSS, Chicago, IL).
Results
Of our 128 patients, 59 had a lymph node diameter less than 10mm (46.1%), and 69 over 10mm (53.9%), without statistical signification regarding age and gender (Table I).
When we analyzed our results, we found differences that arise statistical signification according to the mean number of lymph nodes removed in each group. For group I a mean of 17.6 lymph nodes were resected (IC95 23.05-26.45). A significant difference was found according to better prognosis factors in group I. T1 and T2 stages prevail in group I, 50 patients (78.1%) vs. 27 (39.1%) in group II, p < 0.001.
Patients without lymphatic dissemination (N0) predominate in group I 62.7 over 30.5% in group II, p < 0.001, being the percentage of Ia and Ib stages higher in group I 57.6 vs. 17.4% in group II, p < 0.001.
According to accumulated 5 years overall survival, which was 71.7% for group I, and 36.2% for group II, this difference was statistically significative (p log-rank = 0.003) (Fig. 1).
Overall survival for lymphatic affected patients (group N+) with lymph nodes size under 10mm group was 47.6 vs. 25% for those over 10 mm (p log-rank = 0.0636) (Fig. 2).
Discussion
One of the most useful methods for gastric cancer staging is computed tomography, which accepts as a positive lymph node those up to 10 mm size (5,6). Therefore, we have considered 10 mm lymph node size as differentiation criteria of each study group. We pursue a possible prognosis relation between large lymph node size isolated in definitive pathological report and overall survival for gastric cancer at 60 months.
Preoperative detection of more than 10 mm lymph nodes would be especially interesting in order to indicate a possible perioperative treatment. This parameter should be related with an advanced disease where a worse prognosis course and less survival could be expected.
Although other pathological parameters are related to gastric cancer outcome, number of affected lymph node, is one of the most important. This study tries to evaluate the average lymph node size harvested, otherwise compared with major prognostic parameters and the most important outcome, overall survival.
Total number of lymph nodes isolated is wide enough in each arm to consider reliable lymph node dissection done, specially related to N staging and large lymph node size harvested parameters.
This study prove that patients with large lymph node size isolated in pathological reports equal or less than 10 mm have a T1 and T2 percentage of 78%, and more than 62% have no lymph node involved. For this group of patients more than a half are Ia or Ib stages. However we have shown a close to signification p value in N positive group overall survival, despite of having a reasonably better mortality curve patients with lymph nodes sized less than 10 mm.
Importance of lymph node size is still unclear and data updated keeps a gap of knowledge in this field. However, lymph node influence has been widely described throughout modern radiologic image approach. Only few recent studies report an independent prognostic value (7-9). In our opinion the possibility of overall survival prediction due to lymph node size in addition to other variables, could change the way we manage gastric cancer, especially in preoperative schedules, even if it was not an independent factor. Once again, Sano's concept of "tailoring treatment" explains how to adapt treatment to each individual case (3).
One of recent discussion topic and the point of interest in gastric cancer treatment is preoperative staging. In addition perioperative chemotherapy has increased relevance of preoperative staging, being described as a dream for some authors (10), while others try hard looking for a preoperative prognostic score based on the idea of improving a poor outcome disease (11).
Our data suggests that simple report of more than one centimetre lymph node size, by preoperative staging methods, could predict a worse overall survival. Our purpose is to establish an alternative schedule for this group of patients, considering perioperative treatment based on Cunningham's results, as a possibility of survival improvement.
In preoperative assessment of lymph node involvement, we have reached that patients whit lymph nodes sized over one centimetre have a high probability presence of adverse prognostic factors against patients with lymph nodes under 10 mm size. In clinical practice this group of patients could be considered as positive for N stage. Nevertheless, a high percentage of patients with large lymph nodes are not detected in general preoperative studies. This fact alerted our group being a reason of a recent publication. In our opinion recent advances could minimize this misdiagnosis fault and should be considered as part of preoperative analysis (12). Significant progress has been achieved by 64-row multidetector CT (13).
So many histology parameters have a great value regarding gastric cancer prognosis and are fundamental at time to indicate a chemotherapy treatment. However most of them are known only after surgery. Perhaps in the new era of perioperative therapy, lymph node size could be the fundamental difference, otherwise lymphatic size is still not enough considered and more studies are needed for this consideration.
According to authors' criteria, two possibilities should improve gastric cancer outcome. An undoubted effectiveness provided by early diagnose and treatment achieving excellent results (14-16), and high accuracy in preoperative staging which will directly benefits patients undergoing perioperative schedules.
Acknowledgment
To Professor Alberto Bianchi for his discipline rigor and the honesty of his speech, insignificant compared with his untiring enthusiasm.
References
1. Cunningham D, Allum W, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson MY, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006; 355: 11-20. [ Links ]
2. Roukos DH. Innovative genomic-based model for personalized treatment of gastric cancer integrating current standards and new technologies. Expert Rev Mol Diag 2008; 8: 29-39. [ Links ]
3. Sano T. Tailoring treatment for curable gastric cancer. Br J Surg 2007; 94: 263-4. [ Links ]
4. Sobin LH, Wittekind CH. TNM Classification of malignant tumours. 5th ed. International Union Against Cancer. Heidelberg, Berlin, New York and Tokio: Springer-Verlag; 1997. [ Links ]
5. Gamon Giner R, Escrig Sos J, Salvador Sanchis JL, Ruiz del Castillo J, García Vila JH, Marcote Valdivieso E. Helical CT evaluation in the preoperative staging of gastric adenocarcinoma. Rev Esp Enferm Dig 2002; 94: 593-600. [ Links ]
6. Habermann CR, Weiss F, Riecken R, Honarpisheh H, Bohnacker S, Staedtler C, et al. Preoperative staging of gastric adenocarcinoma: comparison of helical CT and endoscopic US. Radiology 2004; 230: 465-71. [ Links ]
7. Chung O, Oh ST, Kim BS, Yook JH, Kim SH, Im JT, et al. Large metastasic lymph node size, especially more than 2 cm. Independent predictor of poor prognosis in node positive gastric carcinoma. World J Surg 2008; 32: 262-6. [ Links ]
8. Dahr DK, Yoshimura H, Kinukawa N, Muruyama R, Tachibana M, Kohno H, et al. Metastasic lymph node size and colorectal cancer prognosis. J Am Coll Surg 2005; 200: 20-8. [ Links ]
9. Dahr DK, Kubota H, Maruyama R, Kyriazanosi D, Ohno S, Nagasue N. Prognostic significance of metastasic lymph node size in patients with gastric cancer. Br J Surg 2003; 90: 1522-30. [ Links ]
10. Liphman JC, De Meester TR. Preoperative diagnosis of lymph node metastasis: a dream. Gastric Cancer 2006; 9: 70-1. [ Links ]
11. Vieira Costa ML, Braga Ribeiro KC, Machado M, Vieira Costa AC, Montagnini AL. Prognostic store in gastric cancer: the importance of a combinant analysis of clinical, pathologic and therapeutic factors. Ann Surg Oncol 2006; 13: 843-50. [ Links ]
12. Espin F, Bianchi A, Pulido L, Feliu J, Moreno A, Fantova MJ. Rendimiento de la tomografía computerizada helicoidal en la predicción de afección ganglionar preoperatoria en cáncer gástrico. Med Clin 2009; 132: 214-6. [ Links ]
13. Chen CY, Hasu JS, Wu DC, Kang NY, Hsieh JS, Jaw TJ. Gastric cancer: preoperative local staging with a multidetector row CT. Correlation with surgical and histophatological results. Radiology 2007; 242: 472-82. [ Links ]
14. Butte JM, Torres J, Viviani P, Duarte I, Crovari F, Guzmán S, et al. Long term survival of patients operated for early gastric cancer. Rev Med Chi 2008; 136: 1424-30. [ Links ]
15. Onodera H, Tokunanga A, Yoshiyuki T, Kiyama T, Kato S, Matsukura N, et al. Surgical outcome of 483 patients with early gastric cancer: prognosis, postoperative morbidity and Mortality, and gastric remnant cancer. Hepathogastroenterology 2004; 51: 82-5. [ Links ]
16. Casado Martín F, Domínguez Díaz A, Rodríguez Sanjuán J, López Useros A, Cabrera García M, Moreno Muzás C, et al. Surgery of early gastric cancer: twenty five years experience. Hepathol Gastroenterol 2001; 24: 427-32. [ Links ]
![]() Correspondence:
Correspondence:
Francisco Espín.
Servicio de Cirugía General.
Hospital de Mataró.
Ctra. de Cirera, s/n . 08304 Mataró. Barcelona, Spain.
e-mail to:fran-espin@hotmail.com
Received: 22-04-09.
Accepted: 11-11-09.











 texto en
texto en