Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.8 Madrid ago. 2010
LETTERS TO THE EDITOR
Multifocal hepatic inflammatory pseudotumor: spontaneous regression in a diabetic patient
Pseudotumor inflamatorio multifocal hepático: regresión espontánea en paciente diabética
Key words: Inflammatory pseudotumor. Hepatic mass. Liver. Diabetes mellitus.
Palabras clave: Pseudotumor inflamatorio. Masa hepática. Hígado. Diabetes mellitus.
Dear Editor,
The inflammatory pseudotumor of the liver is an exceptional hepatic lesion first described in 1953 by Pack et al. (1,2) that mimics a malignant tumor but has benign histology and good clinical outcome. Its exact etiology is still unknown (2-4) but has been associated with some systemic inflammatory disorders (1,3). We present a case of a multiple hepatic inflammatory pseudotumor with spontaneous resolution in a patient with type 2 diabetes.
Case report
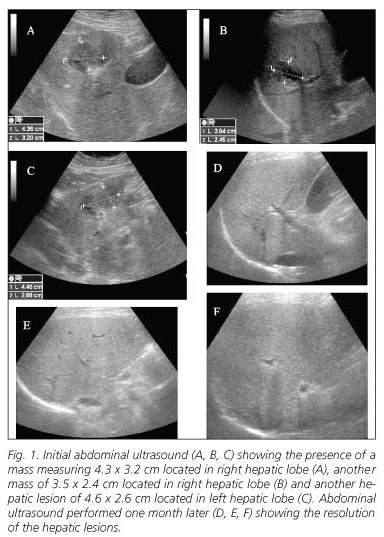
A 66-year-old woman with medical history of type 2 diabetes, on biphasic insulin therapy (using pre-mixed insulin 16 IU - 0 - 18 IU) presented abdominal pain in the last month, with no other symptom, except the need to increase the insulin dose to (54 IU -0 - 54 IU) for adequate glycemic control. The physical examination was negative and laboratory data showed elevated platelet count (601,000 /L) and globular sedimentation rate (107 mm/ 1 hour), with normal values for other results including transaminases, autoimmunity, thyroid hormone, immunoglobulins and IgG4, tumor markers and infections with hepatitis viruses A, B and C, cytomegalovirus, HIV, Epstein-Barr virus, amebiasis and hydatid disease. The abdominal ultrasonography (US) study showed two solid space-occupying lesions in the right hepatic lobe each measuring 4.3 x 3.2 cm and 3.5 x 2.4 cm in size, and another lesion of 4.6 x 2.6 cm located in the left hepatic lobe (Fig. 1 A, B, C) and the enhanced computed tomography (CT) also showed the presence of two hepatic masses in the right lobe of 4 and 3.5 cm and another 3 cm mass located in the left lobe, all with unspecific densitometric features. To rule out malignancy, a percutaneus needle biopsy was performed under US control. The histopathologic analysis revealed an extensive infiltration of plasma cells with lower number of lymphocytes and fibroblasts, and also some multinucleate giant cells, suggesting inflammatory pseudotumor. Immunohistochemical findings showed that plasma cells contained equal amounts of kappa- and lambda- chains and that IgG chains were predominant, while IgG4-positive plasma cells were not present. From these findings and considering the patient was asymptomatic, with better glycemic control and lower insulin dose needed, we decided to reevaluate the patient by carrying out a new ultrasonographic study one month later founding that the lesions had spontaneously regressed (Fig. 1 D, E, F). After this time the patient remained asymptomatic and required a lower insulin dose, finally needing the initial insulin dose.
Discussion
The inflammatory pseudotumor of the liver is an exceptional hepatic lesion with a benign histology and good clinical outcome that can mimic a malignant tumor (1,2). It has been described as a single lesion in many different locations, but it is unusual to find multiple lesions placed in the same organ (2), as observed in our patient who presented multiple hepatic lesions. Diagnosis is difficult because the laboratory data and the radiologic findings are inconclusive; so the histopathologic study of the lesion is needed to show a characteristic histology (2-4).
The presence of plasma cells with some multinucleate giant cells and fibrosis observed in the study of the liver lesions that presented our patient, allowed us to exclude malignancy and confirm the nature of inflammatory pseudotumor.
Even its etiology is not clear, it has been associated with some autoimmune disorders (1,3), and occasionally with diabetes (5,7), but without establishing a definite causal relationship between them. One thing about our patient that caught our attention was the difficulty in optimizing glycemic control requiring high doses of insulin that progressively decreased once the pseudotumor was resolved. We think this could be explained by the severe and active inflammatory process related with the development of the hepatic pseudotumor.
When treating inflammatory pseudotumor, antibiotics, non-steroidal anti-inflammatory drugs and steroid therapy have been used (1). Few cases have required surgery because they were initially suspected to be malignancy or there was no response to conservative treatment (8). Thus, with the possibility of spontaneous regression of the inflammatory pseudotumor, it becomes very difficult to evaluate the efficacy of any of the therapies (1,3,6,9). In our patient we decided not to give any treatment because she was asymptomatic and we did not identify any associated autoimmune process. The clinical follow-up was excellent, with spontaneous resolution of the inflammatory pseudotumor and without evidence of recurrence after one year.
A. Brage Varela1, P. Estévez Boullosa1, J. Pombo Otero2, M. Blanco Rodríguez1, M. Lago Novoa3 and F. Arnal Monreal2
Departments of 1Digestive Diseases, 2Pathology and 3Radiology. Complejo Hospitalario Universitario. A Coruña, Spain
References
1. Sasahira N, Kawabe T, Nakamura A, Shimura K, Shimura H, Itobayashi E, et al. Inflammatory pseudotumor of the liver and peripheral eosinophilia in autoimmune pancreatitis. World J Gastroenterol 2005; 11(6): 922-5. [ Links ]
2. Fukuya T, Honda H, Matsumata T, Kawanami T, Shimoda Y, Muranaka T, et al. Diagnosis of inflammatory pseudotumor of the liver: value of CT. AJR 1994; 163: 1087-91. [ Links ]
3. Koide H, Sato K, Fukusato T, Kashiwabara K, Sunaga N, Tsuchiya T, et al. Spontaneous regression of hepatic inflammatory pseudotumor with primary biliary cirrhosis: Case report and literature review. Worl J Gastroenterol 2006; 12(10): 1645-8. [ Links ]
4. Colakoglu O, Unsal B, Haciyanli M, Tunakan M, Buyrac Z, Yorukoglu G, et al. A successfully managed inflammatory pseudotumour of liver without surgery: report of a case. Acta Gastroenterol Belg 2005; 68(3): 382-4. [ Links ]
5. Younis N, Khaleeli AA, Soran H, Monteith PG. Inflammatory pseudotumor of the liver associated with diabetes mellitus. Int J Clin Pract 2001; 55(10): 717-9. [ Links ]
6. López-Tomassetti Fernández EM, Díaz Luis H, Martín Malagón A, Arteaga González I, Carrillo Pallarés A. Recurrence of inflammatory pseudotumor in the distal bile duct: lessons learned from a single case and reported cases. Worl J Gastroenterol 2006; 12(24): 3938-43. [ Links ]
7. Florentine BD, Hittle TA, Bencharit S. Inflammatory pseudotumor (IPT) of the liver. Appl Radiol 2007; 36(3). [ Links ]
8. Kim YW, Lee JG, Kim KS, Yoon DS, Lee WJ, Kim BR, et al. Inflammatory pseudotumor of the liver treated by hepatic resection: a case report. Yonsei Med J 2006; 47(1): 140-3. [ Links ]
9. Yamaguchi J, Sakamoto Y, Sano T, Shimada K, Kosuge T. Spontaneous regression of inflammatory pseudotumor of the liver: report of three cases. Surg Today 2007; 37(6): 525-9. [ Links ]











 texto en
texto en