Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.9 Madrid sep. 2010
Use of fully covered self-expanding metal stents for the management of benign biliary conditions
Utilización de prótesis metálicas autoexpandibles totalmente recubiertas en procesos biliares benignos
J. García-Cano1, L. Taberna Arana2, C. Jimeno Ayllón1, R. Martínez Fernández1, L. Serrano Sánchez1, A. K. Reyes Guevara1, M. Viñuelas Chicano1, C. J. Gómez Ruiz1, M. J. Morillas Ariño1, J. I. Pérez García1, G. Pérez Vigara1 and A. Pérez Sola1
1Department of Digestive Diseases. 2Patient's Admission Unit. Hospital Virgen de la Luz. Cuenca, Spain
ABSTRACT
Background and aim: biliary self-expanding metal stents (SEMS) have the advantage of being inserted undeployed with very small sizes and provide, when fully opened, large diameters for biliary drainage. However, their use in benign conditions has been very limited, mainly because of difficulty in their extraction. We present our initial experience with a fully covered SEMS (Wallflex) for the management of benign problems of the bile duct.
Patients and methods: in a prospective study, stents of 8 mm in diameter and 4, 6 or 8 cm long were inserted by means of ERCP. These SEMS were chosen when according to medical judgement it was thought that diameters greater than 10 French (3.3 mm) were needed for proper biliary drainage. Stents were extracted also endoscopically, several months later when deemed clinically appropriate.
Results: twenty biliary SEMS were inserted. Reasons for insertion were: large intrahepatic biliary fistula after hydatid cyst surgery (1), perforation of the papillary area following endoscopic sphincterotomy (2), coaxial insertion to achieve patency in obstructed uncovered stents inserted in benign conditions (3), benign strictures (7), multiple and large common bile duct stones that could not be extracted because of tapering and stricturing of the distal common bile duct (7). In all cases, successful biliary drainage was achieved and there were no complications from insertion. Stents were easily extracted after a mean time of 132 days (36-270) in place. Complete resolution of biliary problems was obtained in 14 patients (70%).
Conclusions: in our initial experience, the fully covered Wallflex biliary stent was removed without any complication after being in place in the common bile duct for a mean time of over four months. Therefore, it could be used in the management of benign biliary conditions.
Key words: Self-expanding metal stents. Benign biliary diseases. ERCP.
RESUMEN
Introducción y objetivo: las prótesis metálicas autoexpandibles biliares (PMAB) tienen la ventaja de introducirse plegadas con calibres muy pequeños y proporcionar, al abrirse completamente, diámetros grandes para el drenaje biliar. Su utilización en procesos benignos ha estado muy limitada, fundamentalmente por la dificultad en su extracción. Presentamos nuestra experiencia inicial con una PMAB totalmente recubierta (Wallflex) para tratar patología benigna de la vía biliar.
Pacientes y métodos: en un estudio descriptivo prospectivo se insertaron por CPRE prótesis de 8 mm de diámetro y 4, 6 u 8 cm de longitud, cuando se consideró que para el drenaje biliar eran precisos diámetros superiores a 10 french (3,3 mm). Las prótesis se retiraron también por endoscopia varios meses después según se consideró oportuno clínicamente.
Resultados: se insertaron 20 PMAB. Los motivos fueron: gran fístula biliar intrahepática tras cirugía de quiste hidatídico (1), perforación del área papilar por esfinterotomía endoscópica (2), recanalización de prótesis no recubiertas insertadas en procesos benignos (3), estenosis benignas (7), coledocolitiasis múltiples y de gran tamaño con afilamiento-estenosis del colédoco distal que no pudieron extraerse (7). En todos los casos se logró un drenaje biliar satisfactorio y no se produjeron complicaciones por la inserción. Las prótesis se extrajeron con facilidad a los 132 días de media (36-270). La resolución completa de los procesos se obtuvo en 14 pacientes (70%).
Conclusiones: en nuestra experiencia inicial, la prótesis Wallflex biliar totalmente recubierta pudo extraerse sin complicaciones tras permanecer en el colédoco hasta una media de más cuatro meses, por lo que podría utilizarse en el tratamiento de procesos biliares benignos.
Palabras clave: Prótesis metálicas autoexpandibles biliares. Enfermedades biliares benignas. CPRE.
Abbreviations
SEMS: Self-expanding metal stent.
FCSEMS: fully covered self- expanding metal stent. ERCP: endoscopic retrograde cholangiopancreatography.
F: French.
Introduction
Stent insertion by means of endoscopic retrograde cholangiopancreatography (ERCP), besides with sphincterotomy, are the main techniques to solve biliary obstruction. Until 1979, it was only possible to insert plastic stents with 5 F (1.6 mm) in diameter (1). The initial endoscopists inventive and, mainly, the increase in diameter of the duodenoscope working channel, allowed in 1982 to use 10 F (3.3 mm) plastic stents (2). This is the largest caliber in plastic stents adequate for draining the bile duct. The use 11.5 or 12 F diameters increase technical difficulty for insertion but not the patency of the stent (1).
Plastic stents are routinely used in benign biliary conditions to treat strictures of various etiologies (3), leaks (4), bile duct perforations (5) and in a temporary or permanent way for the management of common bile duct stones that have not been completely extracted after an ERCP session (6,7).
For years, technology improvement has enabled the use of different materials to construct the so called biliary self-expanding metal stents (SEMS). As it is well known, these stents are inserted undeployed with a diameter much smaller than they can reach after they are fully opened. As a consequence, with a simple insertion technique, a size well suited for biliary drainage up to 30 F or 10 mm, can be achieved. However, until recently, most biliary SEMS were bare, that is, they had no coating material on the metal. For this reason, they remained soon embedded in body tissues and could hardly be removed after insertion (8).
They have appeared increasingly SEMS which metal is coated with different materials. If the entire stent is covered, they are named fully covered SEMS (FCSEMS). This enables, in general, not to be trapped in the bile tissue and have the possibility to be extracted (9).
We present our initial experience with the biliary Wallflex, a FCSEMS, in the management of benign biliary disorders. The study aimed to observe the effectiveness of insertion of these SEMS when a diameter for drainage greater than 10 F was needed for the treatment of a biliary problem. At the same time, we would like to ascertain the ease of their removal.
Material, patients and methods
In a prospective, nonrandomized and descriptive study they have been included patients with benign biliary conditions who needed biliary drainage by ERCP with stents having a caliber greater than 10 F. Patients gave their informed consent for the endoscopic intervention (10). No special mention was made of the use of biliary Wallflex FCSEMS, because there were already data on the use of another similar type of stents (11,12).
ERCP was performed with patients in the prone position under conscious sedation with midazolam and fentanyl or petidine, administered by the endoscopist. Access to the bile duct, sphincterotomy and basic manoeuvres of biliary endoscopy were made according to established techniques described previously (13).
The need for a caliber of biliary drainage greater than 10 F was determined in each specific ERCP by the endoscopist who performed the procedures (JGC).
Inserted Wallflex had a diameter of 8 mm and a length that varied between 4, 6 and 8 cm. The decision of not to use, by protocol, the largest SEMS caliber (10 mm), was based in an attempt of not to obstruct the cystic duct. Cholecystitis for this reason is a known complication of FCSEMS (14). However, we tried to have a Magnetic Resonance cholangiopanctreatograpy study prior to the procedure and make an effort to adjust the length of the stent to the take off the cystic duct. The protocol of placement stents with 8 mm in diameter was not altered in patients with previous cholecystectomy. The Wallflex biliary stent (Boston Scientific) is made of Platinol and is entirely covered with Permalume. This membrane is resistant to corrosion that may cause the bile and other juices of the upper gastrointestinal tract. For SEMS insertion, a guidewire was previously placed beyond the stricture in the usual manner.
The biliary Wallflex is designed to be inserted with a short guidewire system, its folded or undeployed diameter is 8 F (2.7 mm). The deployment mechanism is similar to most SEMS. The outer cover that maintains folded the stent is pulled back and the release begins in its distal part. As the SEMS is being opened, a progressive shortening occurs that must be corrected continuously to ensure the fully opening takes place in the correct position and not entirely within the bile duct. To facilitate extraction, the duodenal portion of the stent was placed into the duodenum more prominent than in SEMS placed permanently in tumors. The Wallflex stent has a distal washer completely braided with the filamentary structure in a way that does not break when pulling it and facilitates its removal (Fig. 1).
The exact timing for stent extraction was determined according to clinical grounds and individual assessment of each patient. Therefore, not a rigid schedule was applied. For the extraction, a new ERCP was performed. The stent was grasped by the retrieval loop or by its distal end with a foreign body forceps. After pulling it a bit, the stent was taken inside the working channel of the duodenoscope and extracted through it without the need of removing the entire instrument (Fig. 2). Cholangiography was also performed to assess whether the initial problem responsible for stent insertion had been solved.
When stents were inserted for not extracted common bile duct stones further extraction attempts were made in additional procedures. After ERCPs (both for stent insertion and extraction), patients were admitted at least overnight, to rule out possible complications (15-17).
For follow up, stent position was checked with plain abdominal radiographs (18). Indeterminate biliary conditions were further evaluate after stent insertion with several imaging modalities as EUS (19).
Preliminary results of the 12 first stents inserted have been reported previously in abstract form (20).
Results
Twenty patients were prospectively included over a period of 2 years. During this time a total of 300 ERCP were performed. Fourteen patients were men. Mean age was 72.75 (range 50-91, SD 11). Fifteen had gallbladder in place. Ten inserted stents were 8 cm long, nine 6 cm and one 4 cm. Etiologies responsible for biliary FCSEMS insertion and its evolution are shown in figure 3.
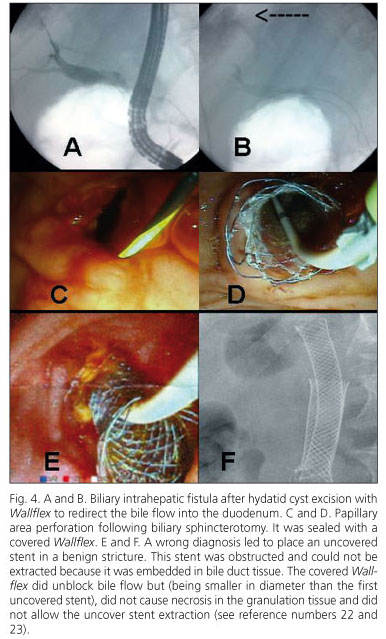
One patient had a large intrahepatic fistula after excision of a hydatid cyst (Fig. 4 A and B). It seemed appropriate, to redirect the bile flow into the bile duct to insert a great diameter stent that had a good apposition with the bile duct wall and produce certain suction into the duodenum. The external drainage stopped 24 hours after insertion.
In two patients (Fig. 4 C and D), stents were placed to seal a perforation occurred after biliary sphincterotomy. Although one of them had to undergo surgery for another duodenal perforation far from the papilla, ERCP perforations of the papillary area subsided in both patients.
In three patients (Fig. 4 E and F), Wallflex FCSEMS were inserted in an attempt to extract previously placed uncovered SEMS. These stents had been wrong placed in benign strictures because of the initial suspicion of malignancy. The uncovered SEMS could not be extracted because they were embedded in bile duct tissues. Insertion of Wallflex FCSEMS tried both to recover patency and to produce necrosis in the hyperplasic tissue on the initial SEMS and in this way, they possibly could be removed. However, although adequate biliary drainage was achieved it was not possible to extract the uncovered stents.
In seven patients (Fig. 5 A and B), stents were placed to treat benign strictures of the distal bile duct. There were two postsphincterotomy papillary stenosis, one of them refractory to sequential insertion of plastic stents side by side and five indeterminate strictures. After Wallflex removal, all seven strictures were adequately dilated. However, a chronic pancreatitis stricture relapsed at 12 months of follow-up.
Another seven patients had large or multiple common bile duct stones that could not be extracted due to inflammatory strictures in the distal bile duct, probably related to cholangitis (Fig. 5 C and D). Stents were inserted and subsequently new sessions of ERCP performed in an attempt to remove them completely. There was success in 5/7.
Overall, complete resolution of biliary problems was obtained in 14 patients (70%).
None of the 15 patients who had gallbladder in place had cholecystitis. There were 3 mild to moderate pancreatitis secondary to maneuvers for biliary access (needle knife precut sphincterotomy in one case) and secondary to attempts to withdraw the uncovered SEMS wrong placed (two patients).
Wallflex FCSEMS were removed at a mean time of 132 days (range 36-270, SD 70). In the moment of extraction all stents, except one, have their distal end in the papillary area. The largest part of the migrated stent was still inside the bile duct but its distal end had slide a bit into the duodenum. All stents were extracted with foreign body forceps (Fig. 2), except the migrated one that needed for extraction a polypectomy snare. Stent removal was easy in all cases.
The patient having the stent for the longer period (270 days) presented with jaundice. The stent was easily removed and at cholangiography a bile duct stricture was observed. This stricture was probably located at the top of the previous Wallflex. A 10 F and 10 cm long plastic stent was inserted and jaundice subsided. This patient had advanced age and Child-Pugh C stage cirrhosis. Etiology of this stricture is uncertain and several factors may have been involved such as repeated episodes of cholangitis (the patient had multiple common bile duct stones that could not be removed and was unfit for surgery) or bile duct irritation by the top end of the Wallflex.
Follow-up time of patients after Wallflex withdrawal was 180 days (range 120-365).
Discussion
In our study, the biliary Wallflex FCSEMS was able to be extracted without any problem from the bile duct after being inserted for a mean time of just over four months. The fact that Wallflex can be removable allows its use in benign biliary conditions as was stated by Soehendra (1): until metal stents are extractable, the use of metal stents for benign strictures should be discouraged.
However, until now, the pattern to be compared with this Wallflex FCSEMS and other commercially available (11) are plastic stents. FCSEMS have been introduced in recent years and there are few studies comparing between them and even less with the plastic ones. Therefore, at present, for the treatment of benign conditions as strictures, progressive dilation by means of plastic stents remains the best choice (21).
No doubt it is easier to obtain a 10 mm diameter of dilatation with the insertion of a single FCSEMS, that to insert three 10 F plastic stents side by side to dilate a severe stricture (3). In the same way, a FCSEMS costs about 10 times more than a plastic one, but this difference diminishes when it is necessary to insert progressively multiple plastic stents in several ERCP procedures.
It is therefore necessary to individualize specific cases of benign biliary diseases necessitating stent drainage. We have used a FCSEMS in 5 types of biliary disorders.
Firstly, to treat an intrahepatic biliary fistula. It is common experience among biliary endoscopists and ours that cystic duct stump and common bile duct leaks usually heal with sphincterotomy and plastic stents, even of 7 F in caliber. However, intrahepatic fistulae require large suction pressure into the duodenum. This was achieved in our case, almost immediately, with the insertion of a biliary Wallflex FCSEMS. It has also been reported the use of similar types of FCSEMS to treat refractory leaks to plastic stents (11).
Second, we used the biliary Wallflex FCSEMS to seal two perforations after biliary sphincterotomy. Although plastic stents have also been used extensively for this purpose, in our cases, we thought that drilling would be better occluded and the patients could be discharged before using a FCSEMS.
Third, we tried to use FCSEMS to induce necrosis in the granulation tissue of uncovered SEMS inserted in benign strictures at a diagnostic stage that seemed neoplastic. This concept of "induce necrosis" with a FCSEMS on another uncover SEMS was originally used to extract Ultraflex SEMS from the esophagus (22). Pérez-Miranda et al. (23) have also applied this method for the extraction of uncover SEMS from the bile duct. We believe that in our case it was not effective because FCSEMS had 8 mm in diameter whilst uncover SEMS previously inserted had 10 mm and contact between them was not appropriate.
Benign strictures of various etiologies and secondary to cholangitis for common bile duct stones were the last two reasons because of FCSEMS were inserted. Causes that led to choose these stents instead of plastic ones were diverse: large bile duct dilatation, strictures narrowness, the presence of cholangitis or the need to reduce the time of endoscopic intervention in fragile patients under conscious sedation and in whom the ERCP could not be prolonged to insert multiple side by side plastic stents.
The ease with which the Wallflex had been removed also means that it could be used, if necessary, for the initial drainage of distal malignant or undetermined strictures, even in the case that surgery will be performed afterwards (24,25).
In conclusion, our initial experience with the biliary Wallflex FCSEMS is that it can be easily removed after insertion and remain in place for several months. Therefore, it can be used in benign biliary conditions. However, at present there is still insufficient data and it is necessary to individualize each specific situation in which it could be employed. Further studies are needed to determine its indications in benign biliary diseases and how long the Wallflex can stay in the bile duct (26).
References
1. Seitz U, Soehendra N. Which stents do we need? The case for plastic stents. Endoscopy 1998; 30(Supl. 2): A242-A246. [ Links ]
2. Huibregtse K, Tytgat GN. Palliative treatment of obstructive jaundice by transpapillary introduction of large bore bile duct endoprosthesis. Gut 1982; 23: 371-5. [ Links ]
3. Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc 2001; 54: 162-8. [ Links ]
4. Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Germanidis G, Zavos C, et al. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc 2008; 22: 101-6. [ Links ]
5. Fátima J, Baron TH, Topazian MD, Houghton SG, Igbal CW, Ott BJ, et al. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg 2007; 142: 448-54. [ Links ]
6. García-Cano Lizcano J, González Martín JA, Taberna Arana L, Racionero M, Morillas Ariño MJ, Pérez Sola A. Plastic biliary stents in endoscopically irretrievable common bile duct stones. (Spanish). Revista de la Asociación Castellana de Aparato Digestivo (ACAD) 2003; 19: 3-6. [ Links ]
7. García-Cano Lizcano J, González Martín JA, Pérez Sola A, Morillas Ariño MJ. Success rate of complete extraction of common bile duct stones at first endoscopy attempt. Rev Esp Enferm Dig 2002; 94: 340-50. [ Links ]
8. Dumonceau JM, Devière J, Delhaye M, Baize M, Cremer M. Plastic and metal stents for postoperative benign bile duct strictures: the best and the worst. Gastrointest Endosc 1998; 47: 8-17. [ Links ]
9. Kahaleh M, Tokar J, Le T, Yeaton P. Removal of self expandable metallic wall stents. Gastrointest Endosc 2004; 60: 640-4. [ Links ]
10. García-Cano J, Bermejo Saiz E. Patient information: Endoscopic retrograde cholangiopancreatography (ERCP). Rev Esp Enferm Dig 2009; 101: 580. [ Links ]
11. Wang AY, Ellen K, Berg CL, et al. Fully covered self-expandable metallic stents in the management of complex biliary leaks: preliminary data - a case series. Endoscopy 2009; 41: 781-6. [ Links ]
12. Mahajan A, Ho H, Sauer B, Phillips MS, Shami VM, Ellen K, et al. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video). Gastrointest Endosc 2009; 70: 303-9. [ Links ]
13. García-Cano J, González-Martín JA. Bile duct cannulation: success rates for various ERCP techniques and devices at a single institution. Acta Gastroenterol Belg 2006; 69: 261-7. [ Links ]
14. Ho H, Mahajan A, Gosain S, Jain A, Brock A, Rehan ME, et al. Management of complications associated with partially covered biliary metal stents. Dig Dis Sci 2010; 55: 516-22. [ Links ]
15. García-Cano LJ, González-Martín JA, Morillas-Arino J, Pérez-Sola A. Complications of endoscopic retrograde cholangiopancreatography. A study in a small ERCP unit. Rev Esp Enferm Dig 2004; 96: 163-73. [ Links ]
16. Peñaloza-Ramírez A, Leal-Buitrago C, Rodríguez-Hernández A. Adverse events of ERCP at San José Hospital of Bogotá (Colombia). Rev Esp Enferm Dig 2009; 101: 837-49. [ Links ]
17. García-Cano J, Taberna-Arana L, Jimeno-Ayllón C, Viñuelas-Chicano M, Martínez-Fernández R, Serrano-Sánchez L, et al. Biliary sphincterotomy dilation for the extraction of difficult common bile duct stones. Rev Esp Enferm Dig 2009; 101: 541-5. [ Links ]
18. De la Morena Madrigal EJ. ERCP and plain abdominal radiology (Spanish). Rev Esp Enferm Dig 2008; 100: 660. [ Links ]
19. Iglesias-García J, Lariño-Noia J, Seijo-Ríos S, Domínguez-Muñoz JE. Endoscopic ultrasound for cholangiocarcinoma re-evaluation alter Wallstent® placement. Rev Esp Enferm Dig 2008; 100: 236-7. [ Links ]
20. García-Cano J, Delgado-Torres V, Jimeno-Ayllón C, Martínez-Fernández R, Serrano-Sánchez L, Viñuelas-Chicano M et al. Initial experience with the new fully covered Wallflex® biliary stent used as a removable endoprosthesis in benign conditions. Endoscopy 2009; 41(Supl. 1) A395. [ Links ]
21. van Boeckel PG, Vleggaar FP, Siersema PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol 2009; 17(9): 96. [ Links ]
22. Evrard S, Le Moine O, Lazaraki G. Self-expanding plastic stents for benign esophageal lesions. Gastrointest Endosc 2004; 60: 894-900. [ Links ]
23. Pérez-Miranda M, González-Carro P, González-Huix F, de la Serna C, Pérez-Roldán F, Figa M. Endoscopic removal of uncovered, partially and fully covered biliary SEMS: problems and salvage techniques. A GEPED Multicenter Descriptive Study. Gastrointest Endosc 2008; 67: AB93. [ Links ]
24. Kahaleh M, Brock A, Conaway MR, Shami VM, Dumonceau JM, Northup PG, et al. Covered self-expandable metal stents in pancreatic malignancy regardless of resectability: a new concept validated by a decision analysis. Endoscopy 2007; 39: 319-24. [ Links ]
25. van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der Harst E, Kubben FJ, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 2010; 362: 129-37. [ Links ]
26. Ahaleh M, Behm B, Clarke BW, Brock A, Shami VM, de La Rue SA, et al. Temporary placement of covered self-expandable metal stents in benign biliary strictures: a new paradigm? (with video). Gastrointest Endosc 2008; 67: 446-54. [ Links ]
 Correspondence:
Correspondence:
J. García-Cano.
Department of Digestive Diseases.
Hospital Virgen de la Luz.
C/ Hermandad Donantes de Sangre, 1.
16002 Cuenca, Spain.
email: j.garcia-cano@terra.es
Received: 22-01-10.
Accepted: 25-02-10.











 texto en
texto en