Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.3 Madrid mar. 2011
PICTURES IN DIGESTIVE PATHOLOGY
Primary intestinal lymphoma
Linfoma intestinal primario
Roberto González-Soler, Elena Castro-Ortiz, Covadonga García-Suárez, Ángel Lancho-Seco, Eva Santos-Blanco, David Carral-Martínez, Pilar Olivencia-Palomar, Susana Ávila-Nasi, Abel González-Ramírez and Leopoldo López-Rosés
Deparment of Digestive Diseases. Hospital Xeral-Calde de Lugo. Spain
Case report
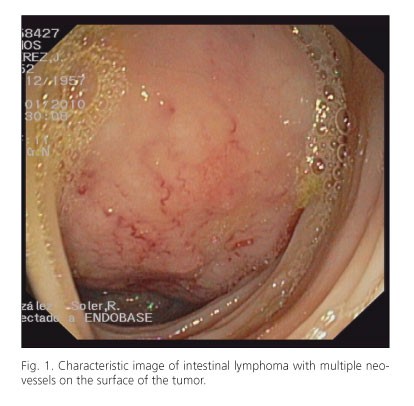
A 52 year old man had been complained of abdominal pain during the last 4-month. The pain was located in the upper left quadrant and it radiated to the epigastrium. It increased when eating and was accompanied by asthenia, anorexia and 3 kg weight loss. The patient did not report melena, rectal bleeding, fever or evening sweating. On physical examination, lymph nodes were not observed. A large and hard mass was palpable in mesogastrium. The analysis showed iron deficiency anemia with no other data of interest, and an ultrasonographic study showed a mass in the splenic flexure, with the transverse colon and descending colon apparently involved; it was compatible with colon cancer as first possibility. A colonoscopy was performed: At 60 cm from the anus, an approximately 4-5 cm in diameter lesion was seen, which had a preserved and highly vascularized mucosa, and that was suggestive of extrinsic compression or submucosal tumor (Fig. 1). Biopsies were taken, and they were reported as consistent with diffuse large B cell non-Hodgkin's lymphoma. Aspirate and bone marrow biopsies were also performed, being normal. Finally, a chest and abdominal-pelvic CT revealed a 11x 16 cm inframesocolic mass that compressed the transverse colon and infiltrated the jejunum, forming an aneurysmatic loop with a large necrotic component. It began a chemotherapy treatment, but one month later the patient was operated on because of a jejunal perforation.
Discussion
The incidence of primary gastrointestinal lymphoma is low, comprising 1-4% of tumors of the stomach, small intestine and colon (1). When it appears with intestinal involvement, there is a predilection for males, with an incidence peak between 50-70 years (2). The disease is usually advanced at diagnosis because the symptoms they cause are nonspecific. Endoscopy can have a fundamental role in diagnosis, especially if the lesion is accessible; a distinctive image of tortuous tumoral neovessels can be observed (3). Well known risk factors are inflammatory bowel disease (4), autoimmune diseases, immunodeficiency, immunosuppression, celiac disease (5) and nodular lymphoid hyperplasia (6). Treatment should be multidisciplinary, including chemotherapy, surgery and radiotherapy in selected cases.
References
1. Loehr WJ, Mujahed Z, Zahn FD, et al. Primary lymphoma of the gastrointestinal tract: a review of 100 cases. Ann Surg 1969;170:232. [ Links ]
2. Jinnai D, Iwasa Z, Watanuki T. Malignant lymphoma of the large intestine - operative results in Japan. Surg Today 1983;13:331-6. [ Links ]
3. KopµcÏovµ M, et al. New endoscopic feature of intestinal non-Hodgkin lymphoma. Endoscopy 2007;39:E95. [ Links ]
4. Ekbom A, Helmick C, Zack M, Adami HO. Extracolonic malignancies in inflammatory bowel disease. Cancer 1991;67:2015. [ Links ]
5. Catassi C, Fabiani E, Corrao G, et al. Risk of non-Hodgkin lymphoma in celiac disease. JAMA 2002;287:1413. [ Links ]
6. Matuchansky C, Touchard G, Lemaire M, et al. Malignant lymphoma of the small bowel associated with diffuse nodular lymphoid Hyperplasia. N Engl J Med 1985;313:166. [ Links ]











 texto en
texto en