Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.4 Madrid Abr. 2011
https://dx.doi.org/10.4321/S1130-01082011000400011
LETTERS TO THE EDITOR
Acute gastric volvulus: a surgical emergency
Vólvulo gástrico agudo: una urgencia quirúrgica
Key words: Gastric volvulus. Diafragmatic hernia. Paraesophageal hernia.
Palabras clave: Vólvulo gástrico. Hernia diafragmática. Hernia paraesofágica.
Dear Editor,
Paraesophageal hernia is a small part of all hernias of the gastroesophageal junction. Anatomically it is characterized by intra-abdominal position of the gastroesophageal junction associated with a lateral hernial defect to the esophageal hiatus. It can lead to development of serious complications, thus representing a true surgical emergency.
Clinical report
A 68 year-old woman with hypercholesterolemia, osteoarthritis and common symptoms of dysmotility-like dyspepsia was admitted at our institution because of severe epigastric pain with nausea and vomiting. On physical examination the patient appeared affected, with severe epigastric pain on palpation but without peritonitis signs.
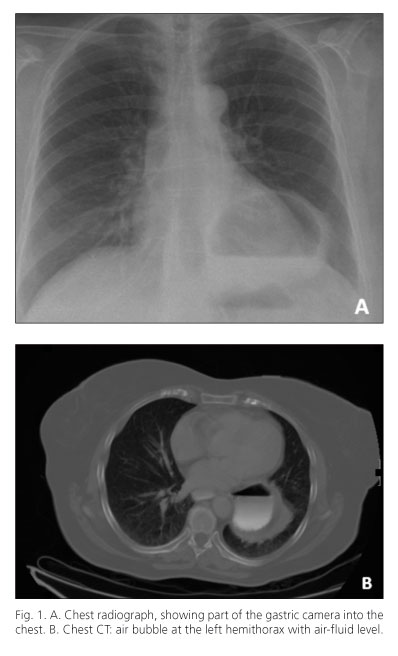
Leucocytosis (15,860 cells) with 86% neutrophils was the only abnormality on laboratory tests. On plain chest radiography (Fig. 1A) a large air bubble in the lower mediastinum with a fluid level was observed. Thoraco-abdominal CT scan showed the esophagogastric junction below the esophageal hiatus, with intrathoracic displacement of the gastric fundus adjacent to the distal esophagus, findings consistent with paraesophageal hiatal hernia with possible volvulus of the herniated fundus (Fig. 1B).
Given the suspicion of gastric volvulus associated with paraesophageal hernia a nasogastric tube placement was attempted, without success. An urgent upper endoscopy was performed showing a wide area of proximal gastric torsion, consistent with volvulus. Endoscopic devolvulation was not achieved (Fig. 2a).
The patient underwent surgery urgently. Through bilateral subcostal laparotomy was accessed the hiatal region, observing the orifice of the left paraesophageal hernia with herniation and torsion of the gastric fundus without ischemic changes. Reduction, gastric detorsion and excision of the hernial sac were then performed. Hernial repair was performed with primary suture associated with Toupet fundoplication (Fig. 2b).
Discussion
Hiatal hernia is a very common disease in the general population, anatomically subdivided into three types: in type I (95%), there is a displacement of the gastro-esophageal junction into the chest, while in type II or paraesophageal, the gastroesophageal junction remains in its normal intraabdominal position, moving the gastric fundus into the mediastinum lateral to the esophagus. Type III or mixed hernia has the two previous components. Hernia types II or III can be associated with complications as incarceration, strangulation or volvulus of hernial contents.
Gastric volvulus is a rare entity, without a clearly established prevalence (1). According to the rotational axis of the stomach are two main types, the organ-axial (59% of cases) and mesentery-axial (29% of cases). About 2% of all cases are mixed volvulus, remaining unclassified about 10% (2). Maximun incidence of gastric volvulus occurs in the fifth decade of life and up to 70% of cases are associated with diaphragmatic defects or pathology of the gastroesophageal junction.
Clinically, acute gastric volvulus is characterized by epigastric pain associated with nausea and vomiting, and dysphagia. In severe cases, respiratory failure may also occur and even sepsis. The plain chest radiography is useful to guide the diagnosis, but most published work considers the computer tomography as the diagnostic test of choice (3).
If no signs of ischemia are suspected, endoscopic devolvulation can be attempted especially in patients at high surgical risk (4). In case of ischemia or failure of endoscopic detorsion, surgery still remains as the treatment of choice. If feasible, most authors prefer a primary suture using nonabsorbable material. For large defects are advised to use prosthetic material.
It is still debated the performing of routine antireflux surgery, gastrostomy or gastropexy to prevent the risk of new volvulus. Partial or total gastrectomy is indicated in the presence of necrosis or associated neoplasia.
Laparoscopic approach has been proven to be safe and feasible for the treatment of gastric volvulus, with low morbidity and mortality and with the benefits associated to minimally invasive surgery. However, it is not advisable this type of approach when there is a high clinical suspicion of associated visceral perforation (3,5).
Lucía Lesquereux Martínez1, Fernando Macías García2, Rocío Ferreiro2, Jorge Martínez Castro1,
Elena Gamborino Caramés1 and Alejandro Beiras Torrado1
Departments of 1Digestive Surgery, and 2Gastroenterology. University Hospital of Santiago de Compostela. A Coruña, Spain
References
1. Sánchez Santacruz YL, Fernández Marín IP. Gastric volvulus like infrequent cause of abdominal pain. Rev Esp Enferm Dig 2009;101: 509-10. [ Links ]
2. Abraldes A, Rodríguez Ramos C, García Trujillo I, Fernández Collado J, Ramírez F, González V. Intrathoracic location of mixed-type acute gastric volvulus. Rev Esp Enferm Dig 2007;99:231-2. [ Links ]
3. Chang CC, Tseng CL, Chang YC. A surgical emergency due to an incarcerated paraesophageal hernia. Am J Emerg Med 2009;27:134.e1-3. [ Links ]
4. Siu WT, Yau KK, Luk YW, Law BKB, Li MKW. Endoscopic reduction of gastric volvulus associated with paraesophageal hernia. Endoscopy 2005; 37:787. [ Links ]
5. Bawahab M, Mitchell P, Church N, Debru E. Management of acute paraesophageal hernia. Surg Endosc 2009;23:255-9. [ Links ]











 texto em
texto em