My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.7 Madrid Jul. 2011
https://dx.doi.org/10.4321/S1130-01082011000700009
PICTURES IN DIGESTIVE PATHOLOGY
Gastric splenosis: a rare cause of digestive bleeding
Esplenosis gástrica: una causa rara de hemorragia digestiva
Bruno Arroja1, Nuno Almeida1, Charl Rafael Macedo2, Ana Paula Moreira2, Pedro Oliveira3, Luis Tomé1, Hermano Gouveia1 and Carlos Sofia1
Departments of 1Gastroenterology, 2Nuclear Medicine and 2Radiology. Hospitais da Universidade de Coimbra, E.P.E., Portugal
A 68 year-old male presented at the emergency department with coffee grounds vomit and melena during the previous 48 hours. He had been subject to a major abdominal surgery with splenectomy at age of 38, after a traumatic injury. Regular medication was low-dose acetylsalicylic acid. On physical examination: blood pressure was 100/73 mmHg; heart rate 74 bpm; cardiac-pulmonary auscultation was normal and abdomen was tender and painless; rectal examination confirmed melena.
Laboratory data: hemoglobin 11.7 g/dL; platelets 221 x 10ˆ3/µL; INR 1.2; aPTT 24.5; BUN 44 mg/dL; creatinine 0.7 mg/dL.
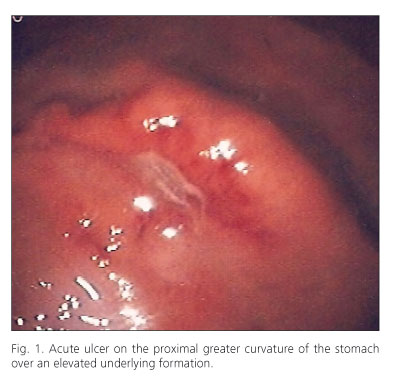
Esophagogastroduodenoscopy visualized an ulcer located on the greater curvature of the proximal gastric body with well delimited borders over an elevated formation (Fig. 1). On computed tomography there was a solid nodular lesion on the greater curvature of the stomach with enhancement on arterial phase highly suggestive of gastric splenosis (Fig. 2A). This hypothesis was confirmed with scintigraphy (Fig. 2B). The patient was medicated with pantoprazole. Three weeks after discharge, endoscopy was repeated revealing frank ulcer healing.
Discussion
The term splenosis was introduced in 1939 by Buchbinder and Lipkoff to designate the heterotopic autotransplantation of splenic tissue which generally occurs after traumatic splenic rupture or surgery (1-5). The most common location for splenic implants, which are generally multiple, is the greater omentum followed by the serosal surface of the small bowel (2). Rare extra-peritoneal locations have been described as well (2,4).
Despite asymptomatic and incidentally diagnosed in most patients, gastrointestinal bleeding, torsion and spontaneous rupture are possible complications (2-4).
Differential diagnosis of splenosis includes tumours, lymphomas and metastatic disease and it should be kept in mind when approaching a digestive bleeding (2-5).
References
1. Buchbinder JH, Lipkoff CJ. Splenosis: multiple peritoneal implants following abdominal injury. Surgery 1939;6:927-34. [ Links ]
2. Margari A, Amoruso M, D'Abbicco D, Notarnicola A, Epifania B. Massive gastrointestinal bleeding due to splenotic nodule of the gastric wall. A case report. Chir Ital 2008;60:863-5. [ Links ]
3. Kuru L, Andac N, Ince L, Bayraktar, Yalcin H. Paragastric splenosis. JBR-BTR 2005;88:142-3. [ Links ]
4. Basile RM, Morales JM, Zupanec R. Splenosis. A cause of massive gastrointestinal hemorrhage. Arch Surg 1989;124:1087-9. [ Links ]
5. Agha FP. Regenerated splenosis masquerading as gastric fundic mass. Am J Gastroenterol 1984;79:576-8. [ Links ]











 text in
text in