Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.8 Madrid ago. 2011
https://dx.doi.org/10.4321/S1130-01082011000800013
LETTERS TO THE EDITOR
Refractory pseudomembranous colitis
Colitis pseudomembranosa refractaria
Key words: Recurrent pseudomembranous colitis. Immunoglobulins.
Palabras clave: Colitis pseudomembranosa recurrente. Inmunoglobulinas.
Dear Editor,
Costridium difficile-associated diarrhea is an important complication of antibiotic use. It is in many instances hospital-acquired and affects more commonly elderly patients with significant co-morbidities, accounting for a significant number of deaths. Approximately 20% of all cases of diarrhea in developed countries are estimated to be secondary to antibiotic use. The most implicated antibiotics predisposing to this condition are clindamycin, penicilins, cephalosporins and fluoroquinolones (1). In recent years the disease has become more frequent, more severe in its clinical course, more refractory to conventional therapy and more prone to recurrences (1). Once diagnosis is established, previous antibiotic treatment should be discontinued and metronidazole (250 mg orally tid or 500 mg intravenous qid) or vancomycin 125 mg qid for 7-14 days must be administered.
Case report
An 83 year-old female patient was admitted for several occasions in our institution during the year of 2008 for chronic diarrhea. At first presentation she reported five to seven bowel movements per day, sometimes with bloody stools. These complaints were accompanied by loss of appetite, weight loss and malaise. Laboratory data: leucocytes 4000 mL, hemoglobin 11.4 g/dL, VGM 89.2 fL, creatinine 89 mmol/L, blood urea nitrogen 3.6 mmol/L; Na+ 144 mmol/L; K+ 2.9 mmol/L, total serum proteins 50 g/L, albumin 20 g/L, CRP 171 mg/L.
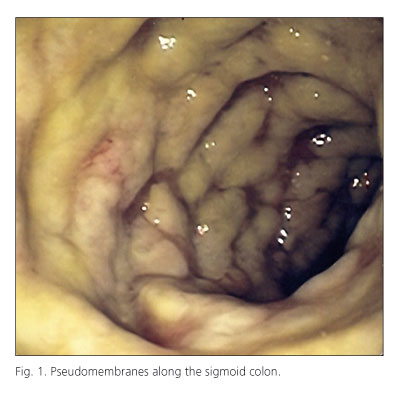
A colonoscopy was performed, disclosing exuberant mucosal adherent plaques throughout the entire colon suggesting pseudomembranous colitis (Fig. 1). The patient was started on oral vancomycin 125 mg qid for seven days with favourable clinical response.
After this admission, the patient was admitted five times further with multiple bowel movements of foul-smelling stools and fever. During these admissions she underwent several courses of treatment with metronidazole, vancomycin and probiotics, always with successive recurrences. Since clinical symptoms were persistent and associated with endoscopic typical findings and important analytical disturbances, it was made the diagnostic of chronic refractory Clostridium difficile-associated colitis. In face of these facts, it was decided to initiate perfusion of immunoglobulins 400 mg/kg associated with prolonged oral vancomycin treatment. The patient has since then been asymptomatic.
Discussion
Clostridium difficile is a gram positive bacillus first described in 1935, responsible for a specific type of diarrhea-pseudomembranous colitis.
In recent years, a more virulent strain classified as NAP1/ B1/027 has been identified and it has been held responsible for Clostridium difficile-associated diarrhea breakthroughs with higher morbidity and mortality (2). Three factors are important for this bacterial virulence: a higher production of specific A and B toxins, resistance to fluoroquinolones and production of a binary toxin (2). The risk of recurrence after a first episode has been estimated as 20% and this figure may reach 40% after a first recurrence. Recurrence may be explained by re-infection with different strain or by persistence of bacteria after the first acute episode (2). Hypoalbuminemia and previous therapeutic failure of metronidazole are associated with recurrences (3), as was seen with our case.
The mortality rate associated with Clostridium difficile-associated diarrhea raised in the USA between 1999 and 2004 from 5.7 to 23.7 per million individuals (3). Is has been stated that resistant strains are due to indiscriminate use of antibiotics, mainly fluoroquinolones, cephalosporins and penicilins. The incorrect use of antibiotics will thus have its impact on hospital admission rates, mortality rate and higher costs with diagnostic examinations and treatments.
Sheila Ferreira1, Manuela Canhoto2, Filipe Silva2, Amália Pereira1 and Renato Saraiva1
Departments of 1Internal Medicine and 2Gastroenterology. Hospital de Santo André, EPE. Leiria, Portugal
References
1. Hurley BW, Nguyen CC, The spectrum of Pseudomembranous Enterocolitis and antibiotic-associated diarrhea. Arch Intern Med 2002;162 (19):2177-84. [ Links ]
2. Kelly CP, La Mont JT, Clostridium difficile-more difficult than ever. N Engl J Med 2008;359(18):1932-40. [ Links ]
3. Hookman P, Barkin JS, Clostridium difficile associated infection, diarrhea and colitis. World J Gastroenterol 2009;15(13):1554-80. [ Links ]