My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.9 Madrid Sep. 2011
https://dx.doi.org/10.4321/S1130-01082011000900007
PICTURES IN DIGESTIVE PATHOLOGY
Intraductal papillary mucinous neoplasm
Neoplasia intraductal mucinosa papilar
José Manuel Ramia-Ángel1, Roberto de la Plaza Llamas1, María Dolores Sánchez-Tembleque2, Belén Pérez-Mies3 and Jorge García-Parreño-Jofré1
1Unit of Hepato-bilio-pancreatic Surgery. Deparment of General and Digestive Surgery. 2Department of Digestive Diseases. 3Department of Pathology. Hospital Universitario de Guadalajara. Guadalajara, Spain
Case report
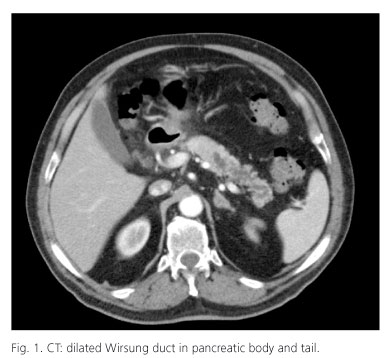
A 75-year-old male with a history of dyslipidemia, no alcohol abuse, acute pericarditis and two pancreatitis episodes 16 and 3 years ago, consulted due to a new pancreatitis episode (amylase 536 IU/l). Abdominal CT and MRI showed irregular, rosary-like dilatation of the duct of Wirsung in the body and tail (Fig. 1). In the pancreatic body-tail, echoendoscopy revealed a 15-mm duct of Wirsung with dilatation of the secondary branches and intramural ductal projections. The duct of Wirsung was punctured, yielding mucin material and ductal-type cells without atypias; amylase 38,858 IU/l, CEA 1,604 IU/l and CA19.9 46,000 IU/l. The colonoscopy findings proved normal. Serum CA19.9 was 43 IU/l. With the diagnosis of intraductal papillary mucinous neoplasm of the pancreas (IPMN), a laparoscopic distal pancreatectomy was performed with preservation of the splenic vessels (Fig. 2). The histological study showed an intraductal proliferation affecting the principal duct and secondary branches, with a cylindrical epithelium of intestinal appearance and abundant mucous secretion (Fig. 3). Lacunar mucus accumulations were observed in the pancreatic stroma, without tumour cells. The observed dysplasia proved intense, though without invasive carcinoma (Fig. 3). The surgical margins were free of disease. There has been no evidence of relapse after 18 months of follow-up.
Discussion
IPMN is an infrequent pancreatic tumour (1-3). The current denomination of the disorder was established by the WHO in the year 2000 (1). Three large groups of IPMNs are considered, according to the type of duct involvement: principal duct, secondary branches or mixed presentations. Lesions of the principal duct should be resected in all cases, since 60% present invasive carcinoma. Secondary branch presentations can be monitored provided there is no CA19.9 tumour marker elevation, the lesion measures no more than 3 cm in size, and no wall thickening is observed (1,2). The preoperative diagnosis is established by CT, MRI and echoendoscopy. Laparoscopic distal pancreatectomy with/without splenic preservation is becoming accepted as the best treatment option for disease of the pancreatic body and tail (4).
Acknowledgements
The translation of this article has been possible to Covidien.
References
1. Tanaka M, Cari S, Adasay V, Fernández del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines of intraductal papillary mucinous neoplasms and mucinous cysts neoplasms of the pancreas. Pancreatology 2006;6:17-32. [ Links ]
2. Bassi C, Crippa S, Salvia R. IPMN: is it time to (sometimes) spare the knife? Gut 2008;57:287-9. [ Links ]
3. Álvarez Cienfuegos J, Rotellar F, Marti P, Valenti V, Zozaya G, et al. Intraductal papillary mucinous neoplasms (IPMN) of the pancreas: clinico-pathologic results. Rev Esp Enferm Dig 2010;102:314-20. [ Links ]
4. Sa Cunha A, Rault A, Beau C, Laurent C, Collet D, Masson B. A single institution prospective study of laparoscopic pancreatic resection. Arch Surg 2008;143:289-95. [ Links ]