Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 no.2 Madrid feb. 2012
https://dx.doi.org/10.4321/S1130-01082012000200002
ERCP during pregnancy
CPRE durante el embarazo
Jesús García-Cano1, Manuel Pérez-Miranda2, Francisco Pérez Roldán3, Pedro González-Carro3, Ferrán González-Huix4, Claudio Rodríguez Ramos5, Antonio Naranjo5, Juan Ángel González Martín6 and Carlos de la Serna2
Departments of Digestive Diseases. 1Hospital Virgen de la Luz. Cuenca, Spain. 2Hospital Río Hortega. Valladolid, Spain. 3Hospital La Mancha-Centro. Alcázar de San Juan. Ciudad Real, Spain. 4Hospital Josep Trueta. Girona, Spain. 5Hospital Puerta del Mar. Cádiz, Spain. 6Hospital Ramón y Cajal. Madrid, Spain
ABSTRACT
Background and aims: ERCP during pregnancy is always challenging for the entire team performing the endoscopic intervention. In this study techniques and different interventional aspects used at several centres about the clinical experience on ERCP in pregnant women are analyzed.
Patients and methods: the practice on ERCP in pregnant women in six centers during a period of ten years is reported.
Results: eleven patients were included in the study. Mean age was 30.6 years. Indication for ERCP was always symptomatic common bile duct stone (CBDS) disease. Before the procedure abdominal ultrasound was performed at all times and magnetic resonance cholangiopancreatography in four occasions. Conscious sedation by means of midazolam and fentanyl or meperidine was applied. Sphincterotomes and guidewires were used for bilary cannulation. Sometimes, rapid exchange platforms with short-length guidewires controlled by the same endoscopist were employed. Biliary cannulation was confirmed in 9 occasions by bile aspiration. In five procedures, a mean of 30 seconds of fluoroscopy was used, both to verify cannulation and to corroborate complete CBDS clearance. These patients had the pelvic zone protected with a lead shield and radiation dose was measured. Ten biliary sphincterotomies were performed followed by CBDS extraction. Two plastic stents were inserted. Relief of biliary obstruction was attained in all circumstances. Only one patient had hyperamylasemia after ERCP. All pregnant women had healthy foetuses with normal deliveries.
Conclusions: with experience, ERCP appears to be a safe technique during pregnancy. With simple measures fluoroscopic time can be diminished or even abolished. It seems that ERCP during pregnancy is underused in our working areas, although it has shown to be a useful technique for relieving biliary obstruction.
Key words: Endoscopic retrograde cholangiopancreatography (ERCP). Pregnancy. Common bile duct stones. Bile duct diseases. Pregnancy complications.
RESUMEN
Antecedentes y objetivos: la CPRE realizada durante el embarazo constituye siempre un reto para todo el equipo que participa en la intervención endoscópica. En este estudio se analizan los diferentes aspectos y técnicas en varios centros sobre la experiencia clínica de la CPRE realizada en mujeres gestantes.
Pacientes y métodos: experiencia en seis centros sobre las CPRE en embarazadas durante 10 años.
Resultados: se incluyeron 11 pacientes con edad media de 30,6 años. La indicación fue siempre coledocolitiasis sintomática. Antes de la CPRE se realizó ecografía abdominal en todos los casos y colangiorresonancia en 4. Se utilizó sedación consciente con midazolam y fentanilo o meperidina. Para la canulación biliar se utilizaron esfinterotomos y guías. A veces con sistemas de intercambio rápido y guías cortas manejadas por el endoscopista. En 9 ocasiones la confirmación de canulación biliar fue por aspiración de bilis. Se utilizó fluoroscopia (media de 30 segundos) en 5 procedimientos, para confirmar la canulación biliar y asegurar la extracción completa de coledocolitiasis. En estos casos se protegió la zona pélvica con un mandil de plomo y se midió la radiación. Se realizaron 10 esfinterotomías biliares con extracción de las coledocolitiasis y se insertaron dos prótesis plásticas resolviéndose en todos los casos la obstrucción biliar. Tras la CPRE solo hubo hiperamilasemia en una paciente. Todas las gestantes dieron a luz fetos sanos con partos normales.
Conclusiones: con experiencia, la CPRE es una técnica segura durante el embarazo. El tiempo de fluoroscopia puede reducirse incluso suprimirse con medidas sencillas. Parece que, en nuestro medio, la CPRE es poco utilizada en la gestación, aunque es una forma útil para desobstruir la vía biliar.
Palabras clave: Colangiopancreatografía retrógrada endoscópica (CPRE). Embarazo. Coledocolitiasis. Enfermedades del conducto biliar. Complicaciones del embarazo.
Introduction
It is known that hormonal changes during pregnancy increase bile lithogenicity and decrease gallbladder emptying. These facts contribute both to gallstone formation and to suffer from their complications. Cholecystolithiasis prevalence in pregnant women is in the range between 3 and 12% (1). Risk of gallstone cholecystitis during pregnancy is as high as 8 per 10,000 pregnancies and it is the second most common cause of emergency admission for non-obstetric causes after acute appendicitis. Symptomatic common bile duct stone (CBDS) -cholangitis, pancreatitis, jaundice, colicky pain- may occur up to one in every 1,200 pregnancies (2). Acute pancreatitis during pregnancy is usually secondary to biliary causes (3) and it has been related with increased mortality risk for the mother and foetus (4).
Traditionally, in these circumstances, treatment of gallstone disease complications has been conservative, because surgery may be associated with problems such as preterm labour and spontaneous abortion (5,6).
Since the advent of endoscopic retrograde cholangiopancreatography (ERCP) as a minimally invasive procedure and treatment of choice for the majority of biliary obstructions (7) it has also been applied for common bile duct conditions such as symptomatic CBDS during pregnancy (8).
In our country, there are few and isolated references (9,10) on ERCP during pregnancy. Therefore, we decided to conduct a multicenter study on its use.
Patients and methods
A survey was sent to 16 Spanish hospitals about the experience in each centre of ERCP in pregnant women in the last 10 years. Ten hospitals had no experience. Four of these centres had no obstetric departments.
Patients presented in the Emergency Department with symptoms related to bile duct obstruction (colicky pain, cholangitis, jaundice, pancreatitis). Transcutaneous abdominal ultrasound was the first imaging test performed, followed in some cases, by magnetic resonance cholangiopancreatography (MRCP). Endoscopic ultrasound (EUS) was not performed in any patient. Neither abdominal radiographs nor computed tomography (CT) scans were taken. Generally, patients were admitted in Digestive departments, although its evolution was followed also by obstetric specialists.
For ERCP patients were placed in left lateral decubitus (as for normal gastroscopy). The prone position was avoided because of the discomfort resulting from the volume of pregnant uterus. Besides, this position appears to increase uterine blood perfusion.
ERCP was performed with conscious sedation using midazolam, fentanyl or meperidine administered by the same endoscopist. Buscopan was sometimes used to reduce duodenal motility. Patients were monitored by pulse oximetry. Electrocardiography and blood pressure measurements were occasionally done during the procedure. Only in some hospitals the foetus was monitored during and after the ERCP.
When fluoroscopy was employed, patient´s abdomen and pelvis was covered with lead aprons. The upper abdomen was spare from lead shield to allow bile duct examination during endoscopic intervention. Occasionally, radiation amount was measured by personnel from the Radiophysics Department.
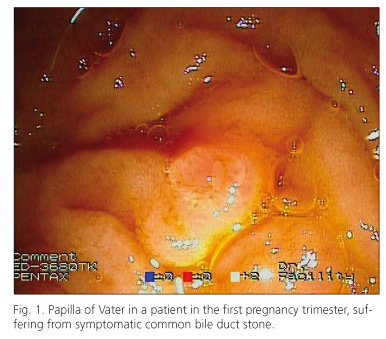
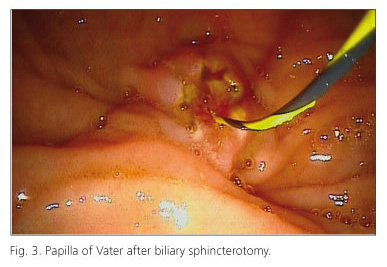
For the procedure a therapeutic duodenoscope was advanced into the papillary area (Fig. 1). Biliary cannulation was performed with sphincterotomes and guidewires. Sometimes, rapid exchange platforms and devices were employed with short-length guidewires controlled by the same endoscopist. After inserting the sphincterotome in the papilla of Vater, in the theoretical part of the common bile duct, the guide was advanced. Easy passage of the guide was a sign that correct cannulation had been achieved (Fig. 2). The sphincterotome was slid over the guidewire inside the bile duct and bile was aspirated. When fluoroscopy was not used, this was the single method to confirm that biliary cannulation had been satisfactory. Afterwards, biliary sphincterotomy was performed in the usual manner in the majority of patients (Fig. 3). The sphincterotome was subsequently withdrawn, leaving the guidewire inside the common bile duct. An extraction balloon was passed over this guidewire and several sweeps were made in the bile duct in an attempt to remove all possible CBDS. After that, to ensure complete biliary drainage, a plastic biliary stent was occasionally inserted (Fig. 4). In these cases, a new ERCP was performed after delivery to complete bile duct clearance.
Following the procedure patients were monitored to rule out complications such as acute pancreatitis, bleeding, cholangitis or perforation.
Results
In the 6 hospitals that responded affirmatively to the survey, a total of 11 ERCP (1.83 per hospital) were performed in 11 pregnant women. Patients´ mean age was 30.6 years. ERCP indication was always symptomatic CBDS, such as biliary colicky pain, cholestasis and obstructive jaundice in 10 cases and cholangitis/pancreatitis in another one. Before ERCP transcutaneous abdominal ultrasound was performed in all cases and MRCP in four. Common bile duct cannulation was achieved in all ERCP. In nine cases biliary cannulation was confirmed exclusively for bile aspiration (Table I). In one occasion the sphincterotome was used for cannulation without a guidewire. Nine times CBDS extraction was complete with a single procedure. Another ERCP after delivery was performed in two patients to extract plastic stents and complete stone extraction. One of these patients presented with multiple gallstones and had to undergo in the third trimester a laparoscopic cholecystectomy. In another patient with pancreatitis, cholecystolithiasis, CBDS, gallbladder hydrops and a splenic vein thrombosis, was treated with low molecular weight heparin, which was discontinued for ERCP.
In four occasions a gynecologist was present in the procedure for foetus monitoring. In three ERCP the amount of radiation, both foetal and maternal, was measured by personnel from the Radio physics Department. Fluoroscopy was used in total in five interventions for an average time of 30 seconds (range 6-48). After ERCP hyperamylasemia was noted in only one patient. All pregnant women gave birth healthy foetuses with normal deliveries.
Discussion
In this study, ERCP rate in pregnant women is very small. For example, in one participating hospital in which it was possible to know precisely the number of births in the whole health district covered, ERCP was performed 1 per 8,500 pregnancies at term. The highest rate was reported by Tang et al. (2) with 1 ERCP per 1,415 births.
It is possible that many of these pregnant women in our area had been treated conservatively without gastroenterologist consultation.
Due to the retrospective nature of our study, it is not possible to know with certainty the evolution of patients that had suffered from CBDS in the different participating hospitals during the study period and who did not undergo ERCP.
The first report on ERCP in pregnant women was published in 1990 (3). Since then, isolated cases have been reported (8-13) and some series (Table II) that, together, do not reach the number of 300 procedures during pregnancy.
Results from these reports show that ERCP is an effective and safe technique for treating symptomatic biliary obstruction during pregnancy. Our data are consistent with these previous experiences. Biliary obstructive disease in our patients was always due to symptomatic CBDS whichtogether with acute cholecystitis, is the most common cause of bilio-pancreatic illness in pregnant women (22). The possible radiation damage to the foetus is one of the key issues of concern in this type of procedures. The effects of radiation on intrauterine development derived primarily from observational studies in atomic bomb survivors. Animal studies have also been reported. It appears that doses below 5 rad or 50 mGy have no deleterious effects (23). Tham et al. (18) observed a maximum dose of 3 mGy to the foetus during 3 minutes of fluoroscopy. Kahaleh et al. (19) showed a maximum of 1.8 mGy in their group of patients. It seems that the radiation threshold for foetal malformations can start at the dose of 100 mGy (24). These figures are rare in diagnostic radiology. Besides, in ERCP the foetus is not in the centre of the radiation beam. Still radiographs produce more radiation than fluoroscopy and should be avoided.
However, in many cases endoscopists prefer not to use radiation and concentrate solely on the technique (20). One reason may be to avoid psychological pressure that fluoroscopy time measurement may have. Especially, if the same endoscopist should be aware of other important aspects such as patient sedation. In our series, more than half of ERCP (6 of 11) were successfully performed without fluoroscopy. Perhaps it should be desirable that another doctor, different from the endoscopist performing the ERCP could be responsible for sedation. Often this is not possible and in almost all of our series, the same physician had to deal with both aspects.
Non-fluoroscopic techniques are facilitated by the use of guidewires to cannulate the papilla of Vater and the employ of rapid exchange devices that allow the endoscopist to control the guide in case there are not trained endoscopist assistants (25).
For patient sedation it can be employed regular medication: midazolam, meperidine, fentanyl, or propofol. Buscopan is also used to reduce duodenal motility. Occasionally, ERCP can be done with general anaesthesia (20). The U.S. Food and Drug Administration (FDA) classifies benzodiazepines as a category D, i.e. unsafe during pregnancy. Some of these drugs may cause defects such as cleft palate. However, sedation with midazolam has been used in many reported cases and it seems that specific doses used for ERCP have not shown any foetal problems.
None of our patients underwent EUS, although the technique was available in some hospitals. CBDS diagnosis was made by abdominal ultrasound and MRCP. EUS is a highly specific method to diagnose CBDS, but it can prolong the time required for sedation if EUS is followed by ERCP. A very promising therapeutic aspect of EUS is the ability to perform during the same session with the linear scan echoendoscope common bile duct cannulation, sphincterotomy and stone extraction (26).
Cholangioscopy through the working channel of the duodenoscope can also help to diagnose bile duct diseases in a non-fluoroscopic way. Besides complete CBDS removal can be verified (27). When fluoroscopy is not employed, CBDS are considered completely removed if the extraction balloon is pulled out easily from the bile duct and does not break. If MRCP has been previously made, the number of CBDS is known and it can be checked if they all have came out. In case of doubt about complete common bile duct cleaning or to ensure biliary drainage, plastic stents have shown to be a safe and temporizing measure (28) until, after delivery, by means of another ERCP a complete CBDS extraction can be achieved.
To avoid possible biliary sphincterotomy complications, some authors (15) have proposed to place plastic stents as the single drainage way at the initial ERCP during pregnancy. After delivery, sphincterotomy and extraction can be performed at another procedure. However, the majority of reported studies have shown sphincterotomy as an appropriate technique to complete treatment in one single intervention. Also in our series, only one ERCP was performed in 9 out of 11 patients.
Although in some of our reported cases a gynaecologist and Radiophysics personnel were present, it is not common practice (2) and ERCP can be performed solely with the endoscopy staff.
In conclusion, ERCP appears to be a safe and effective technique during pregnancy to relief bile duct obstruction. Fluoroscopy time can be reduced and even eliminated by simple measures. It seems, however, that in our working areas ERCP is underused during pregnancy.
References
1. Basso L, McCollum PT, Darling MR, Tocchi A, Tanner WA. A study of cholelithiasis during pregnancy and its relationship with age, parity, menarche, breast-feeding, dysmenorrhea, oral contraception and a maternal history of cholelithiasis. Surg Gynecol Obstet 1992;175: 41-6. [ Links ]
2. Tang SJ, Mayo MJ, Rodriguez-Frias E, Armstrong L, Tang L, Sreenarasimhaiah J, et al. Safety and utility of ERCP during pregnancy. Gastrointest Endosc 2009;69:453-61. [ Links ]
3. Baillie J, Cairns SR, Putman WS, Cotton PB. Endoscopic management of choledocholithiasis during pregnancy. Surg Gynecol Obstet 1990;171:1-4. [ Links ]
4. McKay AJ, O´Neill J, Imrie CW. Pancreatitis, pregnancy and gallstones. Br J Obstet Gynaecol 1980;87:47-50. [ Links ]
5. Akcakaya A, Ozkan OV, Okan I, Kocaman O, Sahin M. et al. Endoscopic retrograde cholangiopancreatography during pregnancy without radiation. World J Gastroenterol 2009;15:3649-52. [ Links ]
6. Amos JD, Schorr SJ, Norman PF, Poole GV, Thomae KR, Mancino AT, et al. Laparoscopic surgery during pregnancy. Am J Surg 1996;171:435-7. [ Links ]
7. Summerfield JA. Biliary obstruction is best managed by endoscopists. Gut 1988;29:741-5. [ Links ]
8. Goldschmiedt M, Wolf L, Shires T. Treatment of symptomatic choledocholithiasis during pregnancy. Gastrointest Endosc 1993;39:812-4. [ Links ]
9. García-Cano J, Palomo Sánchez JC, Gómez Ruiz C. CPRE sin fluoroscopia en una paciente gestante con coledocolitiasis. Rev Esp Enferm Dig 2008;100:100-1. [ Links ]
10. Llach J, Bordas JM, Ginès A, Mondelo F, Terés J. Endoscopic sphincterotomy in pregnancy. Endoscopy 1997;29:52-3. [ Links ]
11. Axelrad AM, Fleischer DE, Strack LL, Benjamin SB, al-Kawas FH. Performance of ERCP for symptomatic choledocholithiasis during pregnancy: techniques to increase safety and improve patient management. Am J Gastroenterol 1994;89:109-12. [ Links ]
12. Binmoeller KF, Katon RM. Needle knife papillotomy for an impacted common bile duct stone during pregnancy. Gastrointest Endosc 1990;36:607-9. [ Links ]
13. Zagoni T, Tulassay Z. Endoscopic sphincterotomy without fluoroscopic control in pregnancy. Am J Gastroenterol 1995;90:1028. [ Links ]
14. Jamidar PA, Beck GJ, Hoffman BJ, Lehman GA, Hawes RH, Agrawal RM, et al. Endoscopic retrograde cholangiopancreatography in pregnancy. Am J Gastroenterol 1995;90:1263-7. [ Links ]
15. Farca A, Aguilar ME, Rodriguez G, de la Mora G, Arango L. Biliary stents as temporary treatment for choledocholithiasis in pregnant patients. Gastrointest Endosc 1997;46:99-101. [ Links ]
16. Sungler P, Heinerman PM, Steiner H, Waclawiczek HW, Holzinger J, Mayer F, et al. Laparoscopic cholecystectomy and interventional endoscopy for gallstone complications during pregnancy. Surg Endosc 2000;14:267-71. [ Links ]
17. Howden JK, Robuck-Mangum G, Jowell PS, et al. Endoscopic management of symptomatic choledocholithiasis during pregnancy: safety and efficacy of endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy (abstract). Gastrointest Endosc 2001;53:AB96. [ Links ]
18. Tham TC, Vandervoort J, Wong RC, Montes H, Roston AD, Slivka A, et al. Safety of ERCP during pregnancy. Am J Gastroenterol 2003;98:308-11. [ Links ]
19. Kahaleh M, Hartwell GD, Arseneau KO, Pajewski TN, Mullick T, Isin G, et al. Safety and efficacy of ERCP in pregnancy. Gastrointest Endosc 2004;60:287-92. [ Links ]
20. Shelton J, Linder JD, Rivera-Alsina ME, Tarnasky PR. Commitment, confirmation, and clearance: new techniques for nonradiation ERCP during pregnancy (with videos). Gastrointest Endosc 2008;67:364-8. [ Links ]
21. Daas AY, Agha A, Pinkas H, Mamel J, Brady PG. ERCP in pregnancy: is it safe? Gastroenterology & Hepatology 2009;5:851-5. [ Links ]
22. Menees S, Elta G. Endoscopic retrograde cholangiopancreatography during pregnancy. Gastrointest Endosc Clin N Am 2006;6:41-57. [ Links ]
23. American College of Obstetricians and Gynecologist. Committee on Obstetric Practice. ACOG Committee Opinion. Number 299, September 2004. Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol 2004;104:647-51. [ Links ]
24. International Commission on Radiological Protection. ICRP Publication 84: Pregnancy and Medical Radiation. Oxford, United Kingdom: Pergamon Press; 2000. [ Links ]
25. López A, Ferrer I, Villagrasa RA, Ortiz I, Maroto N, Montón C, et al. A new guidewire cannulation technique in ERCP: successful deep biliary access with triple-lumen sphincterotome and guidewire controlled by the endoscopist. Surg Endosc 2011;25:1876-82. [ Links ]
26. Artifon EL, Kumar A, Eloubeidi MA, Chu A, Halwan B, Sakai P, et al. Prospective randomized trial of EUS versus ERCP-guided common bile duct stone removal: an interim report (with video). Gastrointest Endosc 2009;69:238-43. [ Links ]
27. Girotra M, Jani N. Role of endoscopic ultrasound/SpyScope in diagnosis and treatment of choledocholithiasis in pregnancy. World J Gastroenterol 2010;16:3601-2. [ Links ]
28. García-Cano Lizcano J, González Martín JA, Pérez Sola A, Morillas Ariño MJ. Success rate of complete extraction of common bile duct stones at first endoscopy attempt. Rev Esp Enferm Dig 2002;94:340-5. [ Links ]
![]() Correspondence:
Correspondence:
J. García-Cano.
Department of Digestive Diseases.
Hospital Virgen de la Luz.
C/ Hermandad Donantes de Sangre, 1.
16002 Cuenca. Spain
e-mail: endoscopia@endoscopiaintervencionista.org
Received: 07-09-11.
Accepted: 19-10-11.











 texto en
texto en