Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 no.10 Madrid oct./nov. 2012
https://dx.doi.org/10.4321/S1130-01082012001000004
Factors associated with complete endoscopic resection of an invasive adenocarcinoma in a colorectal adenoma
Factores asociados a la resección endoscópica completa del adenocarcinoma invasivo sobre adenoma de colon
Paola Quintas1, Joaquín Cubiella1, Ignacio Couto2, Luis Bujanda3, Carol Cobian3, Inés Castro1 and Javier Fernández-Seara1
1Department of Gastroenterology. Complexo Hospitalario Universitario de Ourense. Ourense, Spain.
2Department of Gastroenterology. Complexo Hospitalario Universitario de A Coruña. A Coruña, Spain.
3Hospital Donostia. Instituto Biodonostia. Universidad del País Vasco (UPV/EHU). CIBERehd. San Sebastián, Guipúzkoa. Spain
ABSTRACT
Background and objective: endoscopic polypectomy may allow curative resection of invasive adenocarcinoma on colorectal adenoma. Our goal is was to determine the factors associated with complete endoscopic resection of invasive adenocarcinoma.
Methods: retrospective observational study. We included 151 patients with invasive adenocarcinoma on adenomas endoscopically resected between 1999 and 2009. We determined those variables independently related to incomplete resection by a logistic regression. Relation was expressed as Odds Ratio (OR) and its 95% confidence interval (95% CI).
Results: patients were predominantly male (66.2%) and their mean age was 68.03 ± 10.65 years. Colonoscopy was incomplete in 84% of the patients and 60.3% had synchronous adenomas. Invasive adenocarcinoma was mainly located in distal colon (90.7%) and morphology was pedunculated in 75.5%. The endoscopic average size was 22.61 ± 10.86 mm. Submucosal injection was required in 32.5%. Finally, the resection was in one piece in 73.5% and incomplete in 8.6% of the adenocarcinomas. Factors independently associated with incomplete endoscopic resection were size (mm) (OR 1.08, 95% CI 1.03-1.14, p = 0.002), sessile or flat morphology (OR 8.78, 95% CI 2.24-34.38, p = 0.002) and incomplete colonoscopy (OR 4.73, 95% CI 1.15-19.34, p = 0.03).
Conclusions: endoscopic polypectomy allows complete resection of 91.4% of invasive adenocarcinomas on colorrectal adenoma in our series. Factors associated with incomplete resection were the size of the lesion, sessile or flat morphology and incomplete colonoscopy.
Key words: Colorectal cancer. Adenoma. Endoscopic resection.
RESUMEN
Antecedentes y objetivo: la polipectomía endoscópica puede permitir la resección con intención curativa del adenocarcinoma invasivo sobre adenoma de colon. Nuestro objetivo es determinar los factores asociados a la resección endoscópica completa del adenocarcinoma invasivo.
Métodos: estudio retrospectivo observacional. Se incluyeron 151 individuos con un adenocarcinoma invasivo sobre adenoma resecado endoscópicamente entre 1999 y 2009. Se determinaron las variables relacionadas de forma independiente con la resección incompleta mediante una regresión logística. La relación se expresó como Odds Ratio (OR) y su intervalo de confianza (IC 95%).
Resultados: los pacientes fueron predominantemente hombres (66,2%) y la edad media fue 68,03 ± 10,65 años. El 84% de las colonoscopias fueron completas y en el 60,3% se detectaron adenomas sincrónicos. La localización del adenocarcinoma fue principalmente distal (90,7%) y la morfología pediculada en el 75,5%. El tamaño endoscópico de la lesión fue de 22,61 ± 10,86 mm. En el 32,5% de las resecciones se inyectó suero salino submucoso, en el 73,5% se realizó en bloque y en el 8,6% la resección fue incompleta. Los factores que se asociaron de forma independiente a la resección endoscópica incompleta fueron el tamaño (mm) (OR 1,08, IC 95% 1,03-1,14; p = 0,002), la morfología no pediculada (OR 8,78, IC 95% 2,24-34,38; p = 0,002) y la colonoscopia incompleta (OR 4,73, IC 95% 1,15-19,34; p = 0,03).
Conclusiones: la polipectomía endoscópica permite la resección completa del 91,4% de los adenocarcinomas invasivos sobre adenoma en nuestra serie. Los factores asociados a la resección incompleta son el tamaño de la lesión, la morfología no pediculada y la colonoscopia incompleta.
Palabras clave: Cáncer colorrectal. Adenoma. Resección endoscópica.
Introduction
Colorectal adenoma is the primary precursor lesion of colorectal cancer (CRC). For this reason, endoscopic resection of adenoma is performed to prevent progression to CRC (1). In 1-2% of endoscopic polypectomies, the adenocarcinoma is observed to be invading the submucosa indicating a malignant polyp (2). This finding, usually unexpected, is associated with an 8.7% risk of residual disease and 3% risk of recurrence (3). Given this, the management of colorectal adenoma with invasive adenocarcinoma with an initial endoscopic polypectomy is controversial. There are criteria for low risk of residual disease or recurrence after endoscopic resection: well-differentiated adenocarcinoma, absence of vascular or lymphatic invasion, disease-free margin resection, and limited depth of tumour invasion measured using the Haggitt and Kikuchi classifications (3-8). When these criteria are met, endoscopic treatment as an intention-to-cure treatment can be considered, given that the risk of residual disease or recurrence after resection is similar to the risk associated with surgical treatment (2).
Although malignant polyps are uncommon, population-based screening programmes are increasing the number of cases of CRC diagnosed in the initial stages of the disease (9,10). In this context, as many as 27% of CRC cases detected are candidates for endoscopic treatment (11). In relation to this, we need accurate diagnostic criteria for assessing which cases of invasive adenocarcinoma arising in adenoma can be exclusively treated by endoscopic resection (2). A recently published retrospective study identifies factors that are independently associated with the risk of residual disease or recurrence after endoscopic resection: histological high-risk features and incomplete endoscopic resection (12).
For this reason, we decided to analyse a retrospective cohort of patients with endoscopically resected invasive adenocarcinoma arising in adenoma in order to identify factors associated with an incomplete endoscopic resection.
Patients and methods
Study design
This was a retrospective observational study based on data on cases of invasive colon adenocarcinoma, defined as carcinoma with submucosal invasion, initially treated by endoscopic polypectomy in three Spanish university hospitals in Ourense, A Coruña, and Donostia between 1999 and 2009. We only excluded patients with intraepithelial or intramucosal adenocarcinoma, that is, cases of carcinoma without submucosal invasion; and patients with invasive adenocarcinoma arising in adenomas initially resected surgically. The cases were selected from the pathology department registries (SNOMED-CT code: M-82103).
Clinical and endoscopic data collected
For each patient the following information was collected: demographic data (age and sex) and relevant medical history, including any previous diagnosis of cancer or adenoma of the colon. In all cases, endoscopic examinations was carried out by expert endoscopists: more than 2 years of specialist experience in gastroenterology including performing more than 200 colonoscopies per year. Regarding the endoscopic examination, we reviewed whether it had been possible to perform a complete colonoscopy and the presence of synchronous lesions. With respect to the adenoma with invasive adenocarcinoma, we recorded size, location of the lesion, morphology based on the Paris endoscopic classification (13), if submucosal saline injection was required and how resection was performed: complete or incomplete; en bloc or fragmented. The assessment of whether the endoscopic resection had been complete was based on the endoscopist's description. In addition, we checked whether there had been complications after endoscopic resection. Finally, to determine whether there had been a change in the rate of complete endoscopic resection during the study, two time periods were established arbitrarily: before and since 2005.
Statistical analysis
The data were entered in a dedicated database. The continuous variables were described using the mean and standard deviation, while categorical variables were described by the number of cases per category and percentages. Comparisons to identify significant differences were made with the Student's t-test for quantitative variables, and Fisher's exact test for categorical variables. Finally, the variables related to polyp characteristics and the endoscopic examination found to be statistically significant were included in a logistic regression model, to assess whether they were independently associated with the presence of residual disease. Any such associations were expressed as odds ratios (ORs) with 95% confidence intervals (95% CIs). We considered results to be statistically significant when p < 0.05. The statistical analysis was performed using the SPSS 15.0 (SPSS, Chicago, IL).
Ethical considerations
The study was approved by the Clinical Research Ethics Committee of Galicia (ref. 2008/250, 9 December 2008). To gain access to patient medical records for research purposes, we followed the protocols established by the Health Information Management Departments of the hospitals.
Results
Baseline characteristics
We analysed 151 patients diagnosed with invasive adenocarcinoma in adenoma. The mean age of patients was 68.03 ± 10.65 years, mainly men (66.3%). Sixteen patients had a previous diagnosis of cancer, including four cases of CRC. The baseline characteristics are reported in table I.
Endoscopic findings
The endoscopic findings are summarised in table II. Notably, colonoscopy was complete in 84% of the patients and, overall, synchronous adenomas were found in 60.3% (91) patients. The most advanced histological features of the synchronous adenomas were villous histology in almost half the cohort (43 cases, 47.3%) and high-grade dysplasia in 17 patients (18.7%). Synchronous adenomas were found in the following locations: rectum, 22 cases; sigmoid colon, 48; descending colon, 30; transverse colon, 24 and ascending colon, 33.
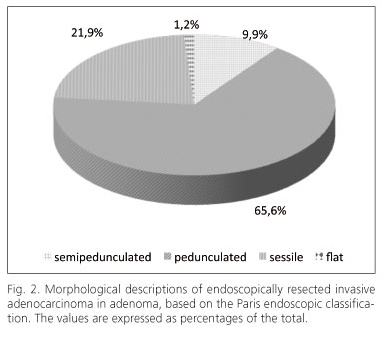
As for the invasive adenocarcinoma in the adenoma, the most common location was distal to the splenic flexure (rectum, 26 cases; sigmoid colon, 93; descending colon, 18; transverse colon, 6; and ascending colon, 8), as illustrated in figure 1. The mean diameter of malignant polyps was 22.61 ± 10.86 mm, with 114, 35 and 2 being classified as pedunculated, sessile and elevated, respectively (Fig. 2). Saline was injected into the submucosa prior to resection in 49 patients and resections were piecemeal in 40 patients, 13 of these being incomplete. Only 5 patients (3.3%) had complications after the endoscopic procedure in the form of self-limiting haemorrhage. In the period prior to 2005, 12% of the endoscopic resections were incomplete while since 2005 only 2.9% of these resections have been incomplete, but the difference was not statistically significant, as can be observed in table II.
Variables associated with incomplete resection
The factors found to be associated with incomplete endoscopic resection in the univariate study were: incomplete colonoscopy (p = 0.036), a sessile or flat morphology (p = 0.003), polyp diameter (mm) (p = 0.002), and fragmented resection (p < 0.001). Including these variables in the logistic regression model, the factors found to be independently associated with incomplete endoscopic resection were polyp diameter (mm) (OR 1.08, 95% CI: 1.03-1.14; p = 0.002), non-pedunculated morphology (OR 8.78, 95% CI: 2.24-34.38; p = 0.002) and incomplete colonoscopy (OR 4.73, 95% CI 1.15-19.34; p = 0.03).
Discussion
In our series, the rate of complete endoscopic resection in invasive adenocarcinoma arising in adenoma was high and has increased with time. In piecemeal resections there is a greater risk of incomplete resection than when en bloc resection is performed. Finally, the diameter and morphology of the lesion, as well as the quality of colonoscopy are independently associated with complete resection of invasive adenocarcinoma.
The diameter and morphology of the lesion have been associated not only with the risk of incomplete endoscopic resection (14-16), but also with the probability of the adenoma transforming into invasive adenocarcinoma (17). In many cases, this is an incidental finding on histological analysis. On the other hand, only complete en bloc resection makes possible to assess whether the surgical margins are disease free or not, and to measure the depth of the tumour invasion (6,10,18). In our series, we have previously found a statistically significant relationship between incomplete resection and the risk of residual disease or recurrence (12). These relationships highlight the need for using complex endoscopic techniques that achieve complete endoscopic resection in advanced adenomas. Both endoscopic mucosectomy and endoscopic submucosal dissection allow the complete en bloc resection of large colonic cancerous lesions with flat or sessile morphologies (19). In this way, we can achieve a complete resection and a proper histological assessment of the risk of residual disease or recurrence.
Another key finding of our study is the relationship between the performance of incomplete colonoscopies and incomplete endoscopic resection. We should note that the rate of complete colonoscopies in our series is lower than the recommended by the quality practice guidelines on colonoscopy (20). It is, however, comparable to other reports of the rates currently described in our setting (21). This finding could be related to the technical skills of endoscopists. For this reason, lesions detected by colonoscopy that are candidates for endoscopic resection should be treated by endoscopists with sufficient experience to perform complex resections. This is of particular importance in screening programmes for CRC based on quantitative immunochemical tests for faecal occult blood. In this context, it is possible to detect advanced adenomas in more than 50% of colonoscopies (22). On the other hand, it is known that referral of patients with adenomas to specialised units when resection is likely to be difficult avoids surgical treatment in 32% to 90% of cases (23-25). In this way, it is possible to reduce both morbidity and healthcare costs associated with the treatment of adenomas (24).
Our study does, however, have some limitations in particular due to the nature of the research. As this was a retrospective study, looking backwards over a considerable period of time, we were not able to collect data on variables associated with the risks of submucosal infiltration (the non-lifting sign) (26) or of detecting invasive adenocarcinoma in adenoma (Kudo classification) (27). Indeed, though non-significant, we observed difference in the rate of complete endoscopic resection in adenocarcinomas resected before and since 2005. This methodological problem is, however, common to all studies analysing the risk factors associated with the natural history of invasive adenocarcinoma arising in adenoma. As this is a relatively uncommon condition, long periods of time are required to collect sufficiently large sample sizes to produce statistically significant results. On the other hand, we did not collect information either on polypoid lesions that were not considered candidates for endoscopic resection or on those endoscopically resected but with no signs of malignancy or with in situ adenocarcinoma in the same period of time. The lack of these data could limit the conclusions in our study, since information to confirm the diagnosis of invasive adenocarcinoma is only obtained from histological analysis of the polyp.
Identifying factors associated with the risk of residual disease after endoscopic resection was not the objective of this analysis. It is nevertheless interesting to note that a recently published study found two factors to be associated with the risk of residual disease or recurrence: incomplete endoscopic resection and histological high-risk features (3,12). Currently, two types of criteria are used to determine the risk of recurrence: histological high risk features (3) and the extent of submucosal invasion (6,7,18). The latter is useful for determining the risk of residual disease in invasive adenocarcionma in sessile protruding or flat elevated lesions (7,18).
In conclusion, endoscopic resection of invasive adenocarcinoma completely removes a high percentage of colonic lesions. The rate of complete endoscopic resection has progressively increased in recent years. Further, the risk of incomplete endoscopic resection was found to be independently associated with the polyp diameter, non-pedunculated morphology, and caecal intubation.
References
1. Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med 1993;329:1977-81. [ Links ]
2. Hassan C, Pickhardt PJ, Di Giulio E, Hunink MG, Zullo A, Nardelli BB. Value-of-information analysis to guide future research in the management of the colorectal malignant polyp. Dis Col Rectum 2010;53:135-42. [ Links ]
3. Hassan C, Zullo A, Risio M, Rossini FP, Morini S. Histologic risk factors and clinical outcome in colorectal malignant polyp: a pooled-data analysis. Dis Col Rectum 2005;48:1588-96. [ Links ]
4. Sakuragi M, Togashi K, Konishi F, Koinuma K, Kawamura Y, Okada M, et al. Predictive factors for lymph node metastasis in T1 stage colorectal carcinomas. Dis Col Rectum 2003;46:1626-32. [ Links ]
5. Volk EE, Goldblum JR, Petras RE, Carey WD, Fazio VW. Management and outcome of patients with invasive carcinoma arising in colorectal polyps. Gastroenterol 1995;109:1801-7. [ Links ]
6. Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD. Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterol 1985;89:328-36. [ Links ]
7. Suzuki T, Sadahiro S, Mukoyama S, Ishikawa K, Yasuda S, Tajima T, et al. Risk of lymph node and distant metastases in patients with early invasive colorectal cancer classified as Haggitt's level 4 invasion: image analysis of submucosal layer invasion. Dis Col Rectum 2003;46:203-8. [ Links ]
8. Kikuchi R, Takano M, Takagi K, Fujimoto N, Nozaki R, Fujiyoshi T, et al. Management of early invasive colorectal cancer. Dis Col Rectum 1995;38:1286-95. [ Links ]
9. Levin B, Lieberman D , McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 2008; 134:1570-95. [ Links ]
10. Bujanda L, Cosme A, Gil I, Arenas-Mirave JI. Malignant colorectal polyps. World J Gastroenterol 2010;16:3103-11. [ Links ]
11. Van Rossum LGM, van Rijn F, van Munster IP, Jansen JBMJ, Fockens P, Laheij RJF, et al. Earlier stages of colorectal cancer detected with immunochemical faecal occult blood tests. Neth J Med 2009;67:182-6. [ Links ]
12. Cubiella J, Arias MD, Penin MC, Quintas P, Couto I, Cobian C, et al. Immunohistochemical alterations in invasive adenocarcinoma in endoscopically resected adenoma and factors associated with risk of residual or recurrent disease. Col Dis 2012;14:e587-94. [ Links ]
13. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58:S3-43. [ Links ]
14. Pérez Roldán F, González Carro P, Legaz Huidobro ML, Villafáñez García MC, Soto Fernández S, de Pedro Esteban A, et al. Endoscopic resection of large colorectal polyps. Rev Esp Enferm Dig 2004;96:36-47. [ Links ]
15. Doniec JM, Löhnert MS, Schniewind B, Bokelmann F, Kremer B, Grimm H. Endoscopic removal of large colorectal polyps: prevention of unnecessary surgery? Dis Col Rectum 2003;46:340-8. [ Links ]
16. Higaki S, Hashimoto S, Harada K, Nohara H, Saito Y, Gondo T, et al. Long-term follow-up of large flat colorectal tumors resected endoscopically. Endoscopy 2003;35:845-9. [ Links ]
17. Fukami N, Lee JH. Endoscopic treatment of large sessile and flat colorectal lesions. Curr Opin Gastroenterol 2006;22:54-9. [ Links ]
18. Tominaga K, Nakanishi Y, Nimura S, Yoshimura K, Sakai Y, Shimoda T. Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Col Rectum 2004;48:92-100. [ Links ]
19. Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamoto T, Uraoka T, et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 2010;24:343-52. [ Links ]
20. Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson D, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002;97:1296-308. [ Links ]
21. Sánchez del Río A, Campo R, Llach J, Pons V, Mreish G, Panadés A, et al. Variation among endoscopy units in the achievement of the standards of colonoscopic performance indicators. Hepatogastroenterology 2008;55:1594-9. [ Links ]
22. Gimeno-García AZ, Quintero E, Nicolás-Pérez D, Hernández-Guerra M, Parra-Blanco A, Jiménez-Sosa A. Screening for familial colorectal cancer with a sensitive immunochemical fecal occult blood test: a pilot study. Eur J Gastroenterol Hepatol 2009;21:1062-7. [ Links ]
23. Lipof T, Bartus C, Sardella W, Johnson K, Vignati P, Cohen J. Preoperative colonoscopy decreases the need for laparoscopic management of colonic polyps. Dis Col Rectum 2005;48:1076-80. [ Links ]
24. Swan MP, Bourke MJ, Alexander S, Moss A, Williams SJ. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc 2009;70:1128-36. [ Links ]
25. Voloyiannis T, Snyder MJ, Bailey RR, Pidala M. Management of the difficult colon polyp referred for resection: resect or rescope? Dis Col Rectum 2008;51:292-5. [ Links ]
26. Kobayashi N, Saito Y, Sano Y, Uragami N, Michita T, Nasu J, et al. Determining the treatment strategy for colorectal neoplastic lesions: endoscopic assessment or the non-lifting sign for diagnosing invasion depth? Endoscopy 2007;39:701-5. [ Links ]
27. Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc 1996;44:8-14. [ Links ]
![]() Correspondence:
Correspondence:
Joaquín Cubiella Fernández.
Departmen of Gastroenterology.
Complexo Hospitalario de Ourense.
C/ Ramón Puga 52-54.
32005 Ourense, Spain
e-mail: joaquin.cubiella.fernandez@sergas.es
Received: 19-06-2012
Accepted: 11-09-2012











 texto en
texto en